Abstract
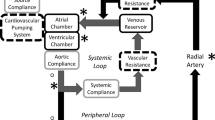
Enhanced external counterpulsation (EECP) is a noninvasive, counterpulsative method to provide temporary aid to the failing heart by sequentially inflating cuffs on the lower extremity out-of-phase with the left ventricle. Optimization of the method necessitates consideration of the hemodynamics created by EECP and the mode of action providing patient benefit. A computational model based on the governing one-dimensional equations is developed that simulates cardiovascular hemodynamics during EECP. The model includes a 30-element arterial system including the left ventricle, bifurcations, and peripheral arterial vessels. Effects of vessel collapse as external pressure is applied, arterial refilling on pressure release, changes in aortic pressure, and shear stress generated in the arteries are each investigated. Device parameters are systematically varied to determine their effect on system performance. Results show the potential for significant collapse and shear augmentation throughout the arteries of the lower extremity. Performance is strongly influenced by the mean level of external pressurization and the timing of cuff inflation, but less so by the relative timing and pressure differences between cuff segments. © 2001 Biomedical Engineering Society.
PAC01: 8719Uv, 0260Cb, 8710+e, 8780-y
Similar content being viewed by others
References
Amsterdam, E. A.et al., Clinical assessment of external pressure circulatory assistance in acute myocardial infarction. Am. J. Cardiol.45:349–356, 1980.
Anderson, D. A., J. C. Tannenhill, and R. H. Pletcher, Computational Fluid Mechanics and Heat Transfer. New York: McGraw Hill, 1984.
Applebaum, R. M., R. Kasliwal, P. A. Tunick, N. Konecky, E. Katz, N. Trehan, and I. Kronzon. Sequential external counterpulsation increases cerebral and renal blood flow. Am. Heart J.133:611–615, 1997.
Arora, R. R., T. M. Chou, D. Jain, B. Fleishman, L. Crawford, T. McKiernan, and R. W. Nesto. The multicenter study of enhanced external counterpulsation (MUST-EECP): Effect of EECP on exercise-induced myocardial ischemia and anginal episodes. J. Am. Coll. Cardiol.33:1833–1840, 1999.
Avolio, A. P. Multi-branched model of the human arterial system. Med. Biol. Eng. Comput.18:709–718, 1980.
Bai, J., D. Wu, and J. Zhang. A simulation study of external counterpulsation. Comput. Biol. Med.24:145–156, 1994.
Bai, J., K. Ying, and D. Jaron. Cardiovascular responses to external counterpulsation: A computer simulation. Med. Biol. Eng. Comput.30:317–323, 1992.
Berger, D. S., J. K.-J. Li, and A. Noordergraf. Differential effects of wave reflections and peripheral resistance on aortic blood pressure: A model-based study. Am. J. Physiol.266:35:H1626-H1642, 1994.
Berger, D. S., J. K.-J. Li, and A. Noordergraf. Arterial wave propagation phenomena, ventricular work, and power dissipation. Ann. Biomed. Eng.23:804–811, 1995.
Bottom, K. E. A numerical model of cardiovascular fluid mechanics during exernal cardiac assist. S.M. thesis. Massachusetts Institute of Technology, May 1999.
Holenstein, R., P. Niederer, and M. Anliker. A viscoelastic model for use in predicting arterial pulse waves. J. Biomech. Eng.102:318–324, 1980.
Hseih, H. J., N. Q. Li, and J. A. Frangos. Shear stress increases endothelial platelet-derived growth factor mRNA levels. Am. J. Physiol.260:H642-H646, 1991.
Kamiya, A., R. Bukhari, and T. Togawa. Adaptive regulation of wall shear stress optimizing vascular tree function. Bull. Math. Biol.46:127–137, 1984.
Kamm, R. D., and A. H. Shapiro. Unsteady flow in a collapsible tube subjected to external pressure or body forces. J. Fluid Mech.95:1–78, 1979.
Lawson, W. E.et al., Efficacy of enhanced external counterpulsation in the treatment of angina pectoris. Am. J. Cardiol.70:859–862, 1992.
Lawson, W. E., J. C. Hui, Z. S. Zheng, L. Burgen, L. Jiang, O. Lillis, Z. Oster, H. Soroff, and P. Cohn. Improved exercise tolerance following enhanced external counterpulsation: Cardiac or peripheral effect?Cardiology87:271–275, 1996.
Lueptow, R. M., J. M. Karlen, R. D. Kamm, and A. H. Shapiro. Circulatory model studies of external cardiac assist by counterpulsation. Cardiovasc. Res.15:443–455, 1981.
Ozawa, E. T. A numerical model of the cardiovascular system for clinical assessment of the hemodynamic state. PhD thesis. Massachusetts Institute of Technology, September 1996.
Parmley, W. W., K. Chatterjee, Y. Charuzi, and H. U. Swan. Hemodynamic effects of noninvasive systolic unloading (nitroprusside) and diastolic augmentation (external counterpulsation) in patients with acute myocardial infarction. Am. J. Cardiol.33:819–825, 1974.
Pedley, T. J., R. C. Schroter, and M. F. Sudlow. Energy losses and pressure drop in models of human airways. Respir. Physiol.9:371–386, 1970.
Soran, A. U., L. E. Crawford, V. M. Schneider, and A. M. Feldman. Enhanced external counterpulsation in the management of patients with cardiovascular disease. Clin. Cardiol.22:173–178, 1999.
Sorroff, H. S., C. T. Cloutier, W. C. Birtwell, L. A. Begley, and J. V. Messer. External counterpulsation, management of cardiogenic shock after myocardial infarction. J. Am. Med. Assoc.229:1441–1450, 1974.
Stettler, J. C., P. Niederer, and M. Anliker. Theoretical analysis of arterial hemodynamics including the influence of bifurcations. Part I: Mathematical model and prediction of normal pulse patterns. Ann. Biomed. Eng.9:145–164, 1981.
Suga, H., and K. Sagawa. Instantaneous pressure-volume relationships and their ratio in the excised, supported canine left ventricle. Circ. Res.35:117–126, 1974.
Suga, H., K. Sagawa, and L. Demer. Determinants of instantaneous pressure in canine left ventricle: Time and volume specification. Circ. Res.46:256–263, 1980.
Sumpio, B. E. Hemodynamic forces and the biology of the endothelium: signal transduction pathways in endothelial cells subjected to physical forces in vitro. J. Vas. Surg.13:744–746, 1991.
Suresh, K., S. Simandl, W. E. Lawson, J. C. Hui, O. Lillis, L. Burger, T. Guo, and P. F. Cohn. Maximizing the hemodynamic benefit of enhanced external counterpulsation. Clin. Cardiol.21:649–653, 1998.
Wolf, T. An experimental/theoretical investigation of parallel inhomogeneities in respiratory flows. PhD thesis. Massachusetts Institute of Technology, June 1990.
Young, D. F., and F. Y. Tsai. Flow characteristics in models of arterial stenoses-II. Unsteady flow. J. Biomech.6:547–559, 1973.
Zheng, Z. S.et al., Sequential external counterpulsation (SECP) in China. Trans. Am. Soc. Artif. Intern. Organs29:599–603, 1983.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ozawa, E.T., Bottom, K.E., Xiao, X. et al. Numerical Simulation of Enhanced External Counterpulsation. Annals of Biomedical Engineering 29, 284–297 (2001). https://doi.org/10.1114/1.1359448
Issue Date:
DOI: https://doi.org/10.1114/1.1359448