Abstract
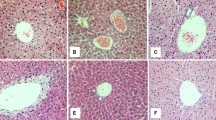
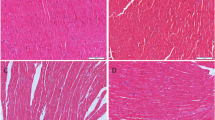
One of the most important mechanisms linking obstructive sleep apnea (OSA) to insulin resistance and type 2 diabetes involves oxidative stress. We examined whether oxidative stress-induced pancreatic injury could be reversed by the antioxidant melatonin (MEL) in male C57BL/6J mice with intermittent hypoxia(IH). Male C57BL/6J mice were randomly divided into four groups: a vehicle-treated normoxic group (CON), a melatonin-treated normoxic group (MEL), a vehicle-treated intermittent hypoxic group (IH) and a melatonin-treated intermittent hypoxic group (IH+MEL). The vehicle (2% ethanol in normal saline) or melatonin (10 mg/kg) was intraperitoneally administered daily for 2 weeks, 30 min before normoxia (intermittent air) or IH exposure. Insulin tolerance, plasma insulin levels, malondialdehyde (MDA) levels, superoxide dismutase (SOD) activity, glutathione (GSH) concentrations, b-cell apoptosis, and mRNA expression of pancreatic antioxidant enzymes glutathione peroxidase 1 (GPx1) and mitochondrial type superoxide dismutase (MnSOD) were measured in all groups. IH significantly increased the level of insulin resistance, plasma insulin content, MDA, and b-cell apoptosis when compared to the CON and MEL groups; however, SOD activity, GSH concentrations and GPx1 and MnSOD mRNA levels decreased in the IH animals. In the melatonin-treated IH mice, all of the above mentioned indices were significantly different from those in the IH mice, trending towards normal values. These results indicate that the oxidative stress induced by IH can lead to pancreatic injury, and that the injury can be partially inhibited by the antioxidant melatonin. These observations may be important to the understanding of the pathological changes noted with OSA.
Similar content being viewed by others
References
Shaw JE, Punjabi NM, Wilding JP et al. Sleep-disordered breathing and type 2 diabetes A report from the International Diabetes Federation Taskforce on Epidemiology and Prevention. Diabetes Res. Clin. Pract. 2008; 81: 2–12.
Idris I, Hall AP, O’Reilly J et al. Obstructive sleep apnoea in patients with type 2 diabetes: aetiology and implications for clinical care. Diabetes Obes. Metab. 2009; 11: 733–41.
Tasali E, Mokhlesi B, Van Cauter E. Obstructive sleep apnea and type 2 diabetes: interacting epidemics. Chest 2008; 133: 496–506.
Larsen JJ, Hansen JM, Olsen NV et al. The effect of altitude hypoxia on glucose homeostasis in men. J. Physiol. 1997; 504: (Pt 1): 241–9.
Braun B, Rock PB, Zamudio S et al. Women at altitude: short-term exposure to hypoxia and/or alpha(1)-adrenergic blockade reduces insulin sensitivity. J. Appl. Physiol. 2001; 91: 623–31.
Oltmanns KM, Gehring H, Rudolf S et al. Hypoxia causes glucose intolerance in humans. Am. J. Respir. Crit. Care Med. 2004; 169: 1231–7.
West SD, Nicoll DJ, Wallace TM et al. Effect of CPAP on insulin resistance and HbA1c in men with obstructive sleep apnoea and type 2 diabetes. Thorax 2007; 62: 969–74.
Chin K, Shimizu K, Nakamura T et al. Changes in intraabdominal visceral fat and serum leptin levels in patients with obstructive sleep apnea syndrome following nasal continuous positive airway pressure therapy. Circulation 1999; 100: 706–12.
Evans JL, Maddux BA, Goldfine ID. The molecular basis for oxidative stress-induced insulin resistance. Antioxid. Redox Signal. 2005; 7: 1040–52.
Kim JE, Kim YW, Lee IK et al. AMPactivated protein kinase activation by 5-aminoimidazole-4-carboxamide-1-beta-D-ribofuranoside (AICAR) inhibits palmitate-induced endothelial cell apoptosis through reactive oxygen species suppression. J. Pharmacol. Sci. 2008; 106: 394–403.
Reiter RJ, Tan DX, Maldonado MD. Melatonin as an antioxidant: physiology versus pharmacology. J. Pineal Res. 2005; 39: 215–16.
Tan DX, Manchester LC, Terron MP et al. One molecule, many derivatives: a never-ending interaction of melato-nin with reactive oxygen and nitrogen species? J. Pineal Res. 2007; 42: 28–42.
El-Sokkary GH, Khidr BM, Younes HA. Role of melato-nin in reducing hypoxia-induced oxidative stress and morphological changes in the liver of male mice. Eur. J. Pharmcol. 2006; 540: 107–14.
Wang WZ, Fang XH, Stephenson LL et al. Melatonin reduces ischemia/reperfusion-induced superoxide generation in arterial wall and cell death in skeletal muscle. J. Pineal Res. 2006; 41: 255–60.
Szarszoi O, Asemu G, Vanecek J et al. Effects of melato-nin on ischemia and reperfusion injury of the rat heart. Cardiovasc. Drugs Ther. 2001; 15: 251–7.
Lee EJ, Lee MY, Chen HY et al. Melatonin attenuates gray and white matter damage in a mouse model of transient focal cerebral ischemia. J. Pineal Res. 2005; 38: 42–52.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001; 25: 402–8.
Ip MS, Lam B, Ng MM et al. Obstructive sleep apnea is independently associated with insulin resistance. Am. J. Respir. Crit. Care Med. 2002; 165: 670–6.
Punjabi NM, Sorkin JD, Katzel LI et al. Sleep-disordered breathing and insulin resistance in middle-aged and overweight men. Am. J. Respir. Crit. Care Med. 2002; 165: 677–82.
Punjabi NM, Shahar E, Redline S et al. Sleep-disordered breathing, glucose intolerance, and insulin resistance: the Sleep Heart Health Study. Am. J. Epidemiol. 2004; 160: 521–30.
Harsch IA, Schahin SP, Radespiel-Troger M et al. Continuous positive airway pressure treatment rapidly improves insulin sensitivity in patientswith obstructive sleep apnea syndrome. Am. J. Respir. Crit. Care Med. 2004; 169: 156–62.
Furukawa S, Fujita T, Shimabukuro M et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. J. Clin. Invest. 2004; 114: 1752–61.
Laight DW, Desai KM, Gopaul NK et al. Pro-oxidant challenge in vivo provokes the onset of NIDDM in the insulin resistant obese Zucker rat. B r. J. Pharmacol. 1999; 128: 269–71.
Eşrefoğlu M, Gül M, Ateş B et al. Ultrastructural clues for the protective effect of melatonin against oxidative damage in cerulein-induced pancreatitis. J. Pineal Res. 2006; 40: 92–7.
Hung MW, Tipoe GL, Poon AM et al. Protective effect of melatonin against hippocampal injury of rats with intermittent hypoxia. J. Pineal Res. 2008; 44: 214–21.
Xu J, Long YS, Gozal D et al. b-cell death and proliferation after intermittent hypoxia: role of oxidative stress. Free Radic. Biol. Med. 2009; 46: 783–90.
Bülbüller N, Dogru O, Umac H et al. The effects of melatonin and pentoxiphylline on L-arginine induced acute pancreatitis. Ulus. Travma Acil Cerrahi Derg. 2005; 11: 108–14.
Konturek SJ, Konturek PC, Brzozowska I et al. Localization and biological activities of melatonin in intact and diseased gastrointestinal tract (GIT). J. Physiol. Pharmacol. 2007; 58: 381–405.
Munoz-Casares FC, Padillo FJ, Briceno J et al. Melatonin reduces apoptosis and necrosis induced by ischemia/ reperfusion injury of the pancreas. J. Pineal Res. 2006; 40: 195–203.
Esparza JL, Gomez M, Rosa Nogues M et al. Melatonin reduces oxidative stress and increases gene expression in the cerebral cortex and cerebellum of aluminum-exposed rats. J. Pineal Res. 2005; 39: 129–36.
Tiedge M, Lortz S, Drinkgern J et al. Relation between antioxidant enzyme gene expression and antioxidative defense status of insulin-producing cells. Diabetes 1997; 46: 1733–42.
Lenzen S, Drinkgern J, Tiedge M. Low antioxidant enzyme gene expression in pancreatic islets compared with various other mouse tissues. Free Radic. Biol. Med. 1996; 20: 463–6.
Al-Delaimy WK, Manson JE, Willett WC et al. Snoring as arisk factor for type II diabetes mellitus: a prospective study. Am. J. Epidemiol. 2002; 155: 387–93.
Elmasry A, Janson C, Lindberg E et al. The role of habitual snoring and obesity in the development of diabetes: a 10-year follow-up study in a male population. J. Intern. Med. 2000; 248: 13–20.
Chen J, Fontes G, Saxena G et al. Lack of TXNIP protects against mitochondria-mediated apoptosis but not against fatty acid-induced ER stress-mediated beta-cell death. Diabetes 2010; 59: 440–7.
Bertuglia S, Reiter RJ. Melatonin reduces microvascular damage and insulin resistance in hamsters due to chronic intermittent hypoxia. J. Pineal Res. 2009; 46: 307–13.
Polotsky VY, Li J, Punjabi NM et al. Intermittent hypoxia increases insulin resistance in genetically obese mice. J. Physiol. 2003; 552: 253–64.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, G., Hou, G., Lu, W. et al. Melatonin protects mice with intermittent hypoxia from oxidative stress-induced pancreatic injury. Sleep Biol. Rhythms 9, 78–85 (2011). https://doi.org/10.1111/j.1479-8425.2011.00486.x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1111/j.1479-8425.2011.00486.x