Abstract
An ambition of healthcare policy has been to move more acute services into community settings. This systematic literature review presents analysis of published operational research methods for modelling patient flow within community healthcare, and for modelling the combination of patient flow and outcomes in all settings. Assessed for inclusion at three levels – with the references from included papers also assessed – 25 “Patient flow within community care”, 23 “Patient flow and outcomes” papers and 5 papers within the intersection are included for review. Comparisons are made between each paper’s setting, definition of states, factors considered to influence flow, output measures and implementation of results. Common complexities and characteristics of community service models are discussed with directions for future work suggested. We found that in developing patient flow models for community services that use outcomes, transplant waiting list may have transferable benefits.
Similar content being viewed by others
Introduction
In recent decades, an ambition of healthcare policy has been to deliver more care in the community by moving acute services closer to patient homes (Munton et al, 2011; NHS England, 2014). This is often motivated by assumed benefits such as reduced healthcare costs, improved access to services, improved quality of care, a greater ability to cope with an increasing number of patients, and improved operational performance in relation to patient health and time (Munton et al, 2011).
A scoping review analysed the evidence regarding the impact that shifting services may have on the quality and efficiency of care (Sibbald et al, 2007). It found that under certain conditions moving services into the community may help to increase patient access and reduce waiting times. Across multiple types of care, however (minor surgery, care of chronic disease, outpatient services and GP access to diagnostic tests), the quality of care and health outcomes may be compromised if a patient requires competencies – such as minor surgery – that are considered beyond those of the average primary care clinician. On the evidence for the effect on the monetary cost of services, Sibbald et al (2007) stated that it was generally expected that community care would be cheaper when offset against acute savings; however, increases in the overall volume of care (Hensher, 1997) and reductions in economies of scale (Powell, 2002; Whitten et al, 2002) may lead to an increase in overall cost in certain instances.
Considering the questions that remain over the impact of shifting services from acute to community sector, it is important to understand how community services may be best delivered. This is where applying operational research (OR) methods to community care services can contribute. For instance, services may be modelled to evaluate how goals, such as better patient access and improved outcomes, may be achieved considering constraints and objectives, such as fixed capacity or reducing operational costs. An example of one such method is patient flow modelling, the focus of this review.
Modelling patient flow
In a model of flow, the relevant system is viewed as comprising a set of distinct compartments or states, through which continuous matter or discrete entities move. Within healthcare applications, the entities of interest are commonly patients (although some applications may consider blood samples or forms of information). Côté (2000) identified two viewpoints from which patient flow has been understood, an operational perspective and, less commonly, a clinical perspective. From an operational perspective, the states that patients enter, leave and move between are defined by clinical and administrative activities and interactions with the care system, such as consulting a physician or being on the waiting list for surgery. Such states may be each associated with a specific care setting or some other form of resource but this need not be the case. In the clinical perspective of patient flow, the states that patients enter, leave and move between are defined by some aspect of the patient’s health, for instance by whether the patient has symptomatic heart disease, or the clinical stage of a patient’s tumour. A more generic view is that the states within a flow model can represent any amalgam of activity, location, patient health and changeable demographics, say, patient age (Utley et al, 2009). A key characteristic is that the set of states and the set of transitions between states comprise a complete description of the system as modelled.
Within the modelling process, characteristics of the patient population and of the states of the system are incorporated to evaluate how such factors influence flow. Examples of the former include patient demographics or healthcare requirements, whilst for the latter, capacity constraints relating to staffing, resources, time and budgets may be considered. The characteristics used depend upon the modelled system, modelling technique and questions being addressed. Considering these, the performance of a system may be evaluated through the use of output measures such as resource utilisation (Cochran & Roche, 2009), average physician overtime (Cayirli et al, 2006) and patient waiting times (Zhang et al, 2009).The output measures calculated within an application depends upon the modelled problem, modelling technique and the factors that are consider to influence flow.
Within acute care settings patient flow modelling has been applied to various scenarios – see Bhattacharjee & Ray (2014). There are also several publications for community care settings; however, no published literature review exists. This systematic literature review was undertaken to gather and analyse two types of patient flow modelling literature relevant for community services. The first were publications that present models of operational patient flow within a community healthcare context, denoted as “Patient flow within community care”. The second were publications that present combinations of patient outcomes and patient flow modelling in any setting, denoted as “Patient flow and outcomes”. Incorporating patient outcomes within the patient flow modelling process is increasingly pertinent within community healthcare. Patient outcomes are used not only to track, monitor and evaluate patient health throughout a care pathway, but also assess the quality of care and inform improvement. The justification for increasing the provision of community care includes improved patient outcomes and satisfaction, thus in combining outcomes and patient flow modelling new and helpful metrics may be developed to evaluate this assertion. Furthermore, such methods help to inform the organisation of healthcare services according to operational capability and the clinical impact on the patient population, unifying two main concerns of providers and patients with a single modelling framework. No specific setting was sought in the “Patient flow and outcomes” to find potentially transferable knowledge and methods for community settings.
To the best of our knowledge, this is the first literature review focussing on OR methods for modelling patient flow applied to community healthcare services and the first to review methods for modelling patient flow and outcomes in combination. This review has been undertaken as part of a project in which OR methods will be developed that combine patient flow modelling and patient outcomes for community care services. The aim of this review was thus twofold. Firstly, to explore different applications of OR methods to community services. Secondly, to understand how patient outcomes have been previously incorporated within flow models. In the discussion section of this paper, we suggest directions for the future of patient flow modelling applied to community care.
Method of review
We conducted a configurative systematic literature review (Gough et al, 2012), an approach intended to gather and analyse a heterogeneous literature with the aim of identifying patterns and developing new concepts. Two searches were performed to find peer-reviewed operational research (OR) publications, relating to “Patient flow within community care” and “Patient flow and outcomes” as previously detailed. We considered all papers published in English before November 2016 with no lower bound publication date, and searched the electronic databases Scopus, PubMed and Web of Science. Using a combination of the search terms listed in Table 1, to find papers related to “Patient flow within community care” we sought records with at least one operational research method term in the article title, journal title or keywords AND at least one patient flow term in the article title, journal title, keywords or abstract AND at least one community health setting term in the article title, journal title, keywords or abstract. Likewise, to find papers related to “Patient flow and outcomes” we sought records with at least operational research method term in the article title, journal title or keywords AND at least one patient flow term in the article title, journal title, keywords or abstract AND at least one outcome term in the article title, journal title, keywords or abstract.
Initial sets of search terms relating to community healthcare settings and OR methods were informed by Hulshof et al (2012). Synonyms were added to these lists prior to the preliminary searches for papers. For patient flow terms and outcome terms, we formed initial lists that we considered relevant. The first batch of papers found using these lists was examined for further applicable search terms. The initial search terms are highlighted in bold in Table 1.
Papers obtained from the final searches were assessed for inclusion for full review at three levels. If a paper was not a literature review it was required to meet all the inclusion and none of the exclusion criteria outlined in Table 2. For each included paper, references were assessed using the same inclusion and exclusion process to find any papers that may have been missed in the searches.
Literature reviews were included at each level if they were concerned with OR methods for evaluating patient flow; focussed on operational processes of healthcare and no equivalent systematic review was included. Within the “Patient flow within community care” literature, review pieces were included if they focussed on community settings; whilst within the “Patient flow and outcome” literature, review pieces were included if they focussed on uses of patient outcomes in modelling processes.
Data tables were constructed to present key characteristics of the literature and shape our analysis. Informed by the initial readings, papers were grouped into five categories based on analytical method with five key characteristics of each model extracted and tabulated for comparison, given in Tables 4, 5 and 6.
Results of literature searches
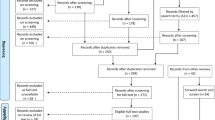
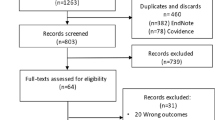
The results of the final searches for and selection of papers are shown in an adapted PRISMA flow chart (Moher et al, 2009), Figure 1. Reasons for the exclusion of texts at full text assessment are shown in Table 3.
Overall 25 “Patient flow within community” papers, 23 “Patient flow and outcomes” papers and 5 papers in the intersection entered the full review. An analysis of this literature is now presented with in the intersection of the two searches included in the “Patient flow within community care” section.
Analysis
Papers found within the “Patient flow within community care” search
Markovian models
A Markovian model views flow within a system as a random process within which the future movement of an entity is dependent only upon its present state and is independent of time spent in that state or the pathway it previously travelled. Whilst systems of healthcare are not truly Markovian, in using these methods, a steady-state analysis of a system may be formulated from which meaningful long-run averages of system metrics can be calculated.
The settings of these publications, presented in Tables 4 and 5, include residential mental healthcare (Koizumi et al, 2005), post-hospital care pathways (Kucukyazici et al, 2011), community services and hospital care (Song et al, 2012) and community-based services for elderly patients with diabetes (Chao et al, 2014).
Within these models, states were defined as different services or stages of care. Kucukyazici et al (2011) and Chao et al (2014) also defined states of post-care outcomes. In the former these included patient mortality, admission to long-term care and re-hospitalisation, whilst the latter defined states of subsequent health progression.
Two main factors were considered to influence flow within these models: the effect of congestive blocking caused by limited waiting space (Koizumi et al, 2005; Song et al, 2012) and the diversity of patients: demographics (Kucukyazici et al, 2011) and severity of disease (Chao et al, 2014). In considering blocking, flow was influenced by the available capacity and average occupancy of each service.
The output measures were queue lengths and wait times for each state – with and without congestive blocking (Koizumi et al, 2005; Song et al, 2012) and the probability that patients would be in a given post-care outcome state (Kucukyazici et al, 2011; Chao et al, 2014). An analysis of different scenarios was undertaken in both latter papers to identify how alternative treatments may help improve post-care outcomes.
None of the papers explicitly reported implementation of their results. We consider implementation to include any action to share or use the results of the work within the modelled setting.
Non-Markovian steady-state models
An optimisation approach for resource allocation by Bretthauer & Côté (1998) defined states as services within specified pathways. The aim was to minimise overall costs whilst maintaining a certain level of care as measured by metrics such as desired waiting. Within the model, flow was influenced by capacity constraints, such as number of beds.
System dynamics analysis
System dynamics is a modelling method whereby computer simulations of complex systems can be built and used to design more effective policies and organisations (Sterman, 2000). Two applications were found, modelling systems of markedly different sizes. Taylor et al (2005) evaluated the uses of community care services to bolster acute cardiac services whilst Wolstenholme (1999) evaluated the UK’s NHS.
States were defined as community or acute services (Taylor et al, 2005) and different sectors of care, namely primary, acute, NHS continuing care and community care (Wolstenholme, 1999).
Capacity and rate variables, such as waiting list size and clinical referral guidelines were considered to influence flow within both models. A feedback mechanism was used by Taylor et al (2005) to evaluate how changes in these variables may stimulate and effect demand.
The main metrics of these models related to demand and access, namely waiting times and patient activity – for example, long-run use of services and length of queues (Wolstenholme, 1999). In both papers, a scenario analysis was performed to evaluate how changes within the model affected its output.
Wolstenholme (1999) reported that some findings were shared with NHS staff.
Analytical methods including time dependence
Applications of analytical methods with time dependence included specialist clinics (Deo et al, 2013, Izady, 2015), care after discharge from an acute stroke unit (Garg et al, 2012), long-term institutional care (Xie et al, 2005, 2006), community mental health services (Utley et al, 2009; Pagel et al, 2012) and home/community care in British Columbia (Hare et al, 2009).
The state definitions within these models related to stages of care/different services (Xie et al, 2005, 2006; Hare et al, 2009; Utley et al, 2009; Pagel et al, 2012; Garg et al, 2012); “waiting” or “in service” (Deo et al, 2013; Izady, 2015) and health states – in particular stages of health progression (Deo et al, 2013) or post-care outcomes (Garg et al, 2012).
The factors considered to influence flow included capacity of services (Pagel et al, 2012, Izady, 2015); patient demographics and care requirements (Xie et al, 2005, 2006; Hare et al, 2009; Garg et al, 2012); patient health between recurrent appointments (Deo et al, 2013) and the length of time in which a person occupied a state (Utley et al, 2009).
Commonly, the system metrics used in these papers related to the time a patient spent interacting with parts of the system – such as expected length of stay, waiting times and time spent in states. Garg et al (2012) calculated the daily cost of care and likely post-care outcome states for patients of different demographic groups. Pagel et al (2012) and Deo et al (2013) identified optimal capacity allocations subject to desired levels of queue lengths and wait times, and impact on patient health, respectively. Hare et al (2009) evaluated the possible future demand for services under different scenarios and situations.
Of these applications, Pagel et al (2012) and Utley et al (2009) reported steps towards implementation. In the former, a software tool was created, whilst in the latter the findings of the model were shared with key stakeholders. Hare et al (2009) also noted the use of their model for care planning within their given setting.
Simulation methods
The settings of these papers included long-term care (Cardoso et al, 2012; Zhang et al, 2012; Zhang and Puterman, 2013), outpatient services (Clague et al, 1997; Swisher & Jacobson, 2002; Matta & Patterson, 2007; Chand et al, 2009; Ponis et al, 2013; Pan et al, 2015), primary care and ambulatory clinics (Santibáñez et al, 2009; Fialho et al, 2011; Shi et al, 2014) and provisions of integrated acute and community services (Bayer et al, 2010; Patrick et al, 2015; Qiu et al, 2016).
States were defined as different services, clinics or sectors of care; or healthcare tasks within single clinics (Clague et al, 1997; Swisher & Jacobson, 2002; Santibáñez et al, 2009; Chand et al, 2009; Fialho et al, 2011; Shi et al, 2014). Chand et al (2009) and Pan et al (2015) modelled the flow of patient information alongside patient flow and thus defined states of information flow.
Factors considered to influence flow commonly included the healthcare requirements/demographics of patients (Clague et al, 1997; Swisher & Jacobson, 2002; Chand et al, 2009; Fialho et al, 2011; Shi et al, 2014), constrained capacity and rates of no show/reneging (Clague et al, 1997; Swisher & Jacobson, 2002; Shi et al, 2014). Bayer et al (2010), Cardoso et al (2012), Ponis et al (2013) and Qiu et al (2016) considered monetary influences such as budgetary constraints, cost of care and profitability. Chand et al (2009) used the variability of time in completing care tasks.
Common metrics related to the time that a patient spent waiting in a state or in the system as whole. Optimised capacity levels relating to key performance measures were also widely considered (Zhang et al, 2012; Zhang and Puterman, 2013; Ponis et al, 2013). Matta & Patterson (2007) calculated a single system metric – an aggregate of multiple performance measures stratified by day, facility routing and patient group. This single metric was formed of measures such as average throughput, average system time and average queue time.
The implementation of suggested changes was recorded in several applications (Clague et al, 1997; Matta & Patterson, 2007; Chand et al, 2009; Santibáñez et al, 2009; Zhang et al, 2012; Pan et al, 2015; Shi et al, 2014).
Papers found within the “Patient flow and outcomes” search
Markovian models
As outlined in Tables 5 and 6, seven publications used Markovian methods and outcomes, two of which were also included within the “Patient flow within community care” section. The five new papers modelled transplant waiting lists (Zenios, 1999; Wang, 2004; Drekic et al, 2015), intensive care units (Shmueli et al, 2003) and emergency care (Kim and Kim, 2015).
In these models, states related to whether patients were “waiting” or had obtained a service/transplant. Drekic et al (2015) defined patient priority states to reflect health deterioration.
The factors that influenced flow related to patient health with groups or states used to assign priorities (Wang, 2004; Drekic et al, 2015) or, represent patient demographics and care requirements. The reneging characteristics of different groups of patients were also considered in each transplant paper with patients modelled as leaving the waiting list due to death or for other reasons. (Zenios, 1999; Drekic et al, 2015).
The output measures of these papers commonly related to the wait time faced by patients. Other metrics included the probability of reneging per patient group (Drekic et al, 2015) and the expected number of deaths for waiting patients (Wang, 2004) or lives saved by an admission policy (Shmueli et al, 2003). Zenios (1999) calculated the average time spent in the system and in the queue for each demographic group, and the fraction of patients from each group who received a transplant.
None of the papers reported an implementation of their results within their care setting.
Non-Markovian steady-state models
The modelled settings and applications included an emergency department (Cochran & Roche, 2009) and two waiting lists, one for hospital care (Goddard & Tavakoli, 2008), the other for transplant patients (Stanford et al, 2014). States were defined as stages of hospital care and as “waiting” or “in service”.
The factors considered to influence flow were patient group and seasonality (Cochran & Roche, 2009) and resource availability and patient health (Goddard & Tavakoli, 2008; Stanford et al, 2014). Each model used metrics relating to the amount of time a patient spent within parts of the system.
Cochran & Roche (2009) reported an implementation of their results with software developed and made available for clinicians and care managers. Feedback and educational sessions were also organised to help key stakeholders to understand the work.
System dynamics analysis
Diaz et al (2015) evaluated patient flow between states of acute care and home care for patients with chronic disease. The factors considered to influence flow related to patient groups based on their care requirements and whether they possessed insurance. Congestion and capacity of resources were also considered. A scenario analysis was performed to evaluate the impact of different patient routes and resource allocations on the level of demand for services and the cost of providing care.
Analytical methods including time dependence
Nine papers were found, two of which were included in the “Patient flow within community care” section. Of the seven remaining, the settings were care for chronic diseases (Deo et al, 2015), two intensive care models (Liquet et al, 2012; Chan et al, 2012), two radiotherapy models (Thomsen & Nørrevang, 2009; Li et al, 2015) and two transplant waiting lists (Zenios & Wein, 2000; Alagoz et al, 2004).
States were defined as “in service” or “waiting”, different services or different appointment slots (Thomsen & Nørrevang, 2009; Li et al, 2015). Alagoz et al (2004), Liquet et al (2012) and Deo et al (2015) also defined multiple health states.
The factors considered to influence flow were commonly related to differences within the patient population pertaining to health (Alagoz et al, 2004; Deo et al, 2015); care requirements or demographic/health-related groups (Zenios & Wein, 2000) and the availability of resources such as organs (Zenios & Wein, 2000; Alagoz et al, 2004) or appointment slots (Thomsen & Nørrevang, 2009; Deo et al, 2015, Li et al, 2015).
Common metrics used by these methods focussed on the amount of time a patient spent waiting for a service – for example, the optimal timing of appointments (Deo et al, 2015) or transplants (Alagoz et al, 2004) subject to changes in patient health. Zenios & Wein (2000) calculated output measures for different groups of patients to evaluate equity within the process of organ allocation. Forecasts of capacity requirements and optimal allocation of resources based on patient groups were also common.
Thomsen & Nørrevang (2009) and Deo et al (2015) reported that some of their suggestions had influenced decision making.
Simulation methods
Eight applications were found with one included in the “Patient flow within community care” (Matta & Patterson, 2007). Of the seven remaining, applications included a cardiac catheterisation clinic (Gupta et al, 2007), three transplant waiting lists (Yuan et al, 1994; McLean & Jardine, 2005; Shechter et al, 2005), an evaluation of an emergency department (Panayiotopoulos & Vassilacopoulos, 1984), neonatal intensive care (DeRienzo et al, 2016) and a healthcare resource allocation model (van Zon & Kommer, 1999).
Within these papers, states were defined as healthcare tasks (van Zon & Kommer, 1999; Gupta et al, 2007), number of beds and “waiting” or “in service”.
The factors considered to influence flow within these models included demographics/care requirements (van Zon & Kommer, 1999; McLean & Jardine, 2005; Shechter et al, 2005; Gupta et al, 2007); the health, mortality and survival rates of patients (van Zon & Kommer, 1999; McLean & Jardine, 2005; Shechter et al, 2005) and resource capacity.
Several metrics were calculated within these methods, with the time patients spent interacting with or waiting within parts of the system a common measure. Other outputs of interest included capacity allocation (Yuan et al, 1994; Gupta et al, 2007; DeRienzo et al, 2016); the cost of care, health benefits of service (van Zon & Kommer, 1999) and the expected survival rate of patients (McLean & Jardine, 2005; Shechter et al, 2005).
Panayiotopoulos & Vassilacopoulos (1984) and Gupta et al (2007) both noted that some of their suggested changes had been implemented.
Summary of findings and discussion across literatures
Findings from across the literature will now be summarised and discussed, drawing together common themes and key characteristics as presented in Tables 4, 5 and 6. In combination, we reviewed 53 papers presenting models of patient flow. 30 applied to community care services which included mental health services, physical health services, outpatient care and patient flow within acute and community settings. Furthermore, 32 applications used, in some form, either queue lengths or the amount of time that a patient spent within states as output measures. The next most common metrics were monetary costs in relation to patient use and the allocation of capacity-related resources.
Within the “Patient flow and community care” literature a range of flow characteristics were considered. For instance, patients access and arrivals to community services were modelled as unscheduled (e.g. Taylor et al, 2005), by appointment (e.g. Deo et al, 2013, 2015), by external referral (e.g. Koizumi et al, 2005), or a mixture of the above (e.g. Chand et al, 2009; Song et al, 2012). Furthermore, multiple care interactions were modelled as either sequential visits to different services (e.g. Koizumi et al, 2005; Song et al, 2012) or as single visits where multiple tasks were carried out (e.g. Chand et al, 2009). In either instance patients were sometimes modelled as being able to recurrently visit the same service over time with some patients using the service more frequently (e.g. Shi et al, 2014; Deo et al, 2013).
Within the “Patient flow and outcome” literature, there were 10 models of transplant/waiting lists, 8 of community, ambulatory and outpatient services, 3 of emergency departments, 4 for intensive care, 2 for radiotherapy and 1 general model of resource allocation. Outcome measures were incorporated within the outputs of these models in three broad ways: (1) system metrics were stratified by outcome related groups; (2) variable patient or population level health was used as an objective or constraint within a model to influence resource allocation or (3) health outcomes – such as patient mortality or future use of care – were used as system metrics. Notably, 15 papers used patient groups to represent differing health/outcomes, whilst 13 papers incorporated variable health/outcome which could change during a course of care. By including variable health/outcome, a model’s output was informed by the effect of a care interaction, or absence of a care interaction, on patient outcomes and on the operation of the system.
Patient groups relating to health/outcome were used in models of each method and were commonly used in resource and service capacity allocations. Notably, their application within steady-state methods is limited since it is difficult to model differing group-dependent variables, such as service times, since the order of patients within these queues is unknown.
Variable health/outcome which could change during a course of care was commonly used within time-dependent methods. They were used to model the effect of care on a population where the modelled time period was large, such as stays with residential care or where multiple interactions were considered.
Across both literatures, queues could be categorised as either physical – constrained demand – or non-physical – unconstrained demand, as per Tables 4, 5 and 6. Physical queues form when patients wait for service within a fixed physical space. Examples include, arrivals forming a queue within a clinic or emergency care (e.g. Chand et al, 2009; Santibáñez et al, 2009; Shi et al, 2014) or when patients move between care interactions and immediately wait within another single physical location (e.g. Xie et al, 2005, 2006; Cochran & Roche, 2009). When physical queues occur, the time a patient spends waiting for service is typically of the order of their expected service time. These queues are constrained and patient demand is modelled from the point when they physically arrive to the service.
Given these dynamics, the most common analysis of physical queues related to the daily operation of single services. Such models were used to gain insight into the delivery of care (e.g. flow between multiple treatments/consultations in a single visit). Studies of physical queues were carried out using each type of method. The choice of method depended on the desired insight, factors considered to influence flow and size of the system. Steady-state methods were sufficient if queue lengths and wait times were of primary concern. However, if variability in input parameters or periodic influences were important, time variable methods were more appropriate. These models typically focus on shorter time frames of care, therefore health/outcome groups were used within these models.
Alternatively, non-physical queues occur when patients may wait in any location away from the service such as their place of residence-e.g. when care is scheduled (Deo et al, 2013) or a patients wait is potentially long and unknown (Zenios & Wein, 2000). Non-physical queues represent unconstrained demand which begins from the point when a patient is referred to a service. A patient’s wait is therefore typically of an order larger than their expected service time. Such models are commonly used to model the demand and access at a system level.
The most common analysis of non-physical queues related to waiting lists and multiple uses of a single or multiple services. Studies of these scenarios were carried out using steady-state analysis or time-dependent methods. Due to the long-run nature of steady-state models these models were appropriate for such situations, especially when variability and differences within the patient population were negligible. In scenarios of scarce appointment or resource allocation, time variable methods were increasingly used. Within these models, variable health/outcome was widely considered due to the longer time frames of care, possible multiple interactions and the benefits stated previously.
It should be noted that this work is limited due to the difficulty of systematically reviewing this literature. In particular, we found two main difficulties. Firstly, these papers are published within a wide range of journals, some within healthcare journals, others in operational research (OR) journals, whilst a proportion was found within journals that were neither health-specific nor OR specific. Secondly, we found that patient flow is described and referred to in myriad ways within literature. No clear standards were found; thus, locating these papers was particularly difficult.
Due to the complexity of finding literature, we cannot claim our findings to be exhaustive. However, by following an iterative process of literature searching our findings are representative of this literature, allowing us to draw meaningful conclusions in the next section.
As a final observation, the reporting of implementation and collaboration varied greatly within each group of analytical method.
Conclusions and directions for future work
Community healthcare consists of a diverse range of geographically disparate services, each providing treatment to patients with specific health needs. As a result, the factors that are considered to influence patient flow are often markedly different to acute services and vary from one service to another. Considering the characteristics discussed in this review, it is common for a mixture of complex dynamics to be modelled within community care applications. Modelling these services can thus become complicated, requiring innovative methods to include all or some of these dynamics. This is highlighted by the range of different methods presented in this review.
Future directions for patient flow modelling within community care are now explored motivated by known challenges for community care, gaps found within the literature and any transferable knowledge between the two sets of literature.
Few models considered patient flow within systems of differing community services with most studies focussing on single services. Likewise, few also considered the mix of patients within these services. Consider, however, a diabetes pathway where patients may require treatment for comorbidities from multiple services based in the community. Each of these services will also provide care to a range of patients, not just those with diabetes. This example highlights a significant challenge in the management of community services. Namely, how to co-ordinate and deliver care within physically distributed, co-dependent services considering increasing episodic use by patients with differing needs. With a shift of focus towards care for the increasing number of patients with multiple long-term illnesses (NHS England, 2014), the patient mix within each service further exacerbates this challenge. Therefore, it would be beneficial to develop methods for modelling patient flow through multiple services to investigate these scenarios.
Considering the above, another useful direction would be to develop time-dependent analytical methods and simulation models for these scenarios. Whilst often analytically difficult, there are important benefits in using these methods as shown by the wide range of applications within this review. Given the characteristics of community services previously discussed, a helpful addition to the research landscape would be models of systems for which steady-state assumptions do not hold or where capacity, demand and timing of patient use vary. This would be helpful in community care where – due to the decentralisation – it can be hard to measure and interpret the impact that changes to one part of the system have on the whole system over short-term and long-term time periods. In considering flow in a system of inter-related services, or situations where patients may re-use the same service over a time period, the development of system level, time-dependent methods would be beneficial in analysing the time variable impact of changes in the immediate, short term and long term for the whole system.
Finally, 13 papers used variable health/outcomes, of which 5 applied to multiple care interactions. Again considering the purpose and nature of community care, we suggest that methods which use multiple health states to model the improvement and decline of patient health throughout a course of care would be a useful direction for future study. A good example of these methods is presented by Deo et al (2013, 2015). Having otherwise not been widely explored, methods that quantify and evaluate the quality of care and include an interaction between patient outcomes, care pathways and flow within the system would be valuable and appropriate for community care modelling.
In considering OR methods for community services which combine patient flow modelling and patient outcomes, there may be some transferable knowledge from transplant models. For situations where non-physical are modelled, transplant list models may provide a useful basis as they share some distinct similarities to community care services – such as reneging, time-varying demand, limited resources and in some cases re-entrant patients. Transplant models may be informative for both scheduled care and unscheduled care.
References
Alagoz O, Maillart LM, Schaefer AJ and Roberts MS (2004) The optimal timing of living-donor liver transplantation. Management Science 50(10), 1420–1430.
Bayer S, Petsoulas C, Cox B, Honeyman A and Barlow J (2010) Facilitating stroke care planning through simulation modelling. Health Informatics Journal 16(2), 129–143.
Bhattacharjee P and Ray PK (2014) Patient flow modelling and performance analysis of healthcare delivery processes in hospitals: a review and reflections. Computers & Industrial Engineering 78, 299–312.
Bretthauer KM and Côté MJ (1998) A model for planning resource requirements in health care organizations. Decision Sciences 29(1), 243–270.
Cardoso T, Oliveira MD and Barbosa-póvoa A (2012) Modeling the demand for long-term care services under uncertain information. Health Care Management Science 15(4), 385–412.
Cayirli T, Veral E and Rosen H (2006) Designing appointment scheduling systems for ambulatory care services. Health Care Management Science 9(1), 47–58.
Chan CW, Farias VF, Bambos N and Escobar GJ (2012) Optimizing intensive care unit discharge decisions with patient readmissions. Operations Research 60(6), 1323–1341.
Chand S, Moskowitz H, Norris JB, Shade S and Willis DR (2009) Improving patient flow at an outpatient clinic: study of sources of variability and improvement factors. Health Care Management Science 12(3), 325–340.
Chao J et al (2014) The long-term effect of community-based health management on the elderly with type 2 diabetes by the Markov modeling. Archives of Gerontology and Geriatrics 59(2), 353–359.
Clague JE, Reed PG, Barlow J, Rada R, Clarke,M and Edwards RHT (1997) Improving outpatient clinic efficiency using computer simulation. International Journal of Health Care Quality Assurance 10(5), 197–201.
Cochran JK and Roche KT (2009) A multi-class queuing network analysis methodology for improving hospital emergency department performance. Computers & Operations Research 36(5), 1497–1512.
Côté MJ (2000) Understanding patient flow. Decision Line 31(2), 8–10.
Deo S, Iravani S, Jiang T, Smilowitz K and Samuelson S (2013) Improving health outcomes through better capacity allocation in a community-based chronic care model. Operations Research 61(6), 1277–1294.
Deo S, Rajaram K, Rath S, Karmarkar US and Goetz MB (2015) Planning for HIV screening, testing, and care at the Veterans Health Administration. Operations Research 63(2), 287–304.
Derienzo CM, Shaw RJ, Meanor P, Lada E, Ferranti J and Tanaka D (2016) A discrete event simulation tool to support and predict hospital and clinic staffing. Health Informatics Journal, 1460458216628314.
Diaz R, Behr J, Kumar S and Britton B (2015) Modeling chronic disease patient flows diverted from emergency departments to patient-centered medical homes. IIE Transactions on Healthcare Systems Engineering 5(4), 268–285.
Drekic S, Stanford DA, Woolford DG and Mcalister VC (2015) A model for deceased-donor transplant queue waiting times. Queueing Systems 79(1), 87–115.
England NHS (2014) Five Year Forward View. London: HM Government.
Fialho AS, Oliveira MD and Sa AB (2011) Using discrete event simulation to compare the performance of family health unit and primary health care centre organizational models in Portugal. BMC Health Services Research 11, 274.
Garg L, McClean S, Barton M, Meenan BJ and Fullerton BJ (2012) Intelligent patient management and resource planning for complex, heterogeneous, and stochastic healthcare systems. IEEE Transactions on Systems, Man, and Cybernetics Part A: Systems and Humans 42(6), 1332–1345.
Goddard J and Tavakoli M (2008) Efficiency and welfare implications of managed public sector hospital waiting lists. European Journal of Operational Research 184(2), 778–792.
Gough D, Thomas J and Oliver S (2012) Clarifying differences between review designs and methods. Systematic Reviews 1, 28.
Gupta D et al (2007) Capacity planning for cardiac catheterization: a case study. Health Policy 82(1), 1–11.
Hare WL, Alimadad A, Dodd H, Ferguson R, Rutherford A (2009) A deterministic model of home and community care client counts in British Columbia. Health Care Management Science 12(1), 80–98.
Hensher M (1997) Improving general practitioner access to physiotherapy: a review of the economic evidence. Health Services Management Research 10(4), 225–230.
Hulshof PJH, Kortbeek N, Boucherie RJ, Hans EW and Bakker PJM (2012) Taxonomic classification of planning decisions in health care: a structured review of the state of the art in OR/MS. Health Systems 1, 129–175.
Izady N (2015) Appointment capacity planning in specialty clinics: a queueing approach. Operations Research 63(4), 916–930.
Kim S and Kim S (2015) Differentiated waiting time management according to patient class in an emergency care center using an open Jackson network integrated with pooling and prioritizing. Annals of Operations Research 230(1), 35–55.
Koizumi N, Kuno E and Smith TE (2005) Modeling patient flows using a queuing network with blocking. Health Care Management Science 8(1), 49–60.
Kucukyazici B, Verter V and Mayo NE (2011) An analytical framework for designing community-based care for chronic diseases. Production and Operations Management 20(3), 474–488.
Li S, Geng N and Xie X (2015) Radiation queue: meeting patient waiting time targets. IEEE Robotics and Automation Magazine 22(2), 51–63.
Liquet B, Timsit JF and Rondeau V (2012) Investigating hospital heterogeneity with a multi-state frailty model: application to nosocomial pneumonia disease in intensive care units. BMC Medical Research Methodology 12(1), 1.
Matta ME and Patterson SS (2007) Evaluating multiple performance measures across several dimensions at a multi-facility outpatient center. Health Care Management Science 10(2), 173–194.
McLean DR and Jardine AG (2005) A simulation model to investigate the impact of cardiovascular risk in renal transplantation. Transplantation Proceedings 37(5), 2135–2143.
Moher D, Liberati A, Tetzlaff J and Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine 151(4), 264–269.
Munton T, Martin A, Marrero I, Llewellyn A, Gibson K and Gomersall A (2011) Evidence: getting out of hospital? The Health Foundation.
Pagel C, Richards DA and Utley M (2012) A mathematical modelling approach for systems where the servers are almost always busy. Computational and Mathematical Methods in Medicine.
Pan C, Zhang D, Kon AWM, Wai SL and Ang WB (2015) Patient flow improvement for an ophthalmic specialist outpatient clinic with aid of discrete event simulation and design of experiment. Health Care Management Science 18(2), 137–155.
Panayiotopoulos JC and Vassilacopoulos G (1984) Simulating hospital emergency departments queuing systems: \((GI/G/m(t)) :(IHFF/N/\infty )\). European Journal of Operational Research 18(2), 250–258.
Patrick J, Nelson K and Lane D (2015) A simulation model for capacity planning in community care. Journal of Simulation 9(2), 111–120.
Ponis ST, Delis A, Gayialis SP, Kasimatis P and Tan J (2013). Applying discrete event simulation (DES) in healthcare: the case for outpatient facility capacity planning. International Journal of Healthcare Information Systems and Informatics 8(3), 58–79.
Powell J (2002) Systematic review of outreach clinics to primary care in the UK. Journal of Health Services Research and Policy 7(3), 177–183.
Qiu Y, Song J and Liu Z (2016) A simulation optimisation on the hierarchical health care delivery system patient flow based on multi-fidelity models. International Journal of Production Research 54(21), 6478–6493.
Santibáñez P, Chow VS, French J, Puterman ML. and Tyldesley S (2009) Reducing patient wait times and improving resource utilization at British Columbia Cancer Agency’s ambulatory care unit through simulation. Health Care Management Science 12(4), 392–407.
Shechter S M, et al (2005) A clinically based discrete-event simulation of end-stage liver disease and the organ allocation process. Medical Decision Making 25(2), 199–209.
Shi J, Peng Y and Erdem E (2014) Simulation analysis on patient visit efficiency of a typical VA primary care clinic with complex characteristics. Simulation Modelling Practice and Theory 47, 165–181.
Shmueli A, Sprung CL and Kaplan EH (2003) Optimizing admissions to an intensive care unit. Health Care Management Science 6(3), 131–136.
Sibbald B, McDonald R and Roland M (2007) Shifting care from hospitals to the community: a review of the evidence on quality and efficiency. Journal of Health Services Research and Policy 12(2), 110–117.
Song J, Chen W and Wang L (2012) A block queueing network model for control patients flow congestion in urban healthcare system. International Journal of Services Operations and Informatics 7(2–3), 82–95.
Stanford DA, Lee JM, Chandok N and Mcalister V (2014) A queuing model to address waiting time inconsistency in solid-organ transplantation. Operations Research for Health Care 3(1), 40–45.
Sterman JD (2000) Business Dynamics: Systems Thinking and Modeling for a Complex World. Boston: McGraw-Hill.
Swisher JR and Jacobson SH (2002) Evaluating the design of a family practice healthcare clinic using discrete-event simulation. Health Care Management Science 5(2), 75–88.
Taylor K, Dangerfield B and le Grand J (2005) Simulation analysis of the consequences of shifting the balance of health care: a system dynamics approach. Journal of Health Services Research & Policy 10(4), 196–202.
Thomsen MS and Nørrevang O (2009) A model for managing patient booking in a radiotherapy department with differentiated waiting times. Acta Oncologica 48(2), 251–258.
Utley M, Gallivan S, Pagel C and Richards D (2009) Analytical methods for calculating the distribution of the occupancy of each state within a multi-state flow system. IMA Journal of Management Mathematics 20(4), 345–355.
van Zon AH and Kommer GJ (1999) Patient flows and optimal health-care resource allocation at the macro-level: a dynamic linear programming approach. Health Care Management Science 2(2), 87–96.
Wang Q (2004) Modeling and analysis of high risk patient queues. European Journal of Operational Research 155(2), 502–515.
Whitten PS, Mair FS, Haycox A, May CR, Williams TL and Hellmich S (2002) Systematic review of cost effectiveness studies of telemedicine interventions. British Medical Journal 324, 1434–1437.
Wolstenholme E (1999) A patient flow perspective of UK health services: exploring the case for new” intermediate care” initiatives. System Dynamics Review 15(3), 253–271.
Xie H, Chaussalet TJ and Millard PH (2005) A continuous time Markov model for the length of stay of elderly people in institutional long-term care. Journal of the Royal Statistical Society: Series A (Statistics in Society) 168(1), 51–61.
Xie H, Chaussalet TJ and Millard PH (2006) A model-based approach to the analysis of patterns of length of stay in institutional long-term care. IEEE Transactions on Information Technology in Biomedicine 10(3), 512–518.
Yuan Y, Gafni A, Russell JD and Ludwin D (1994) Development of a central matching system for the allocation of cadaveric kidneys a simulation of clinical effectiveness versus equity. Medical Decision Making 14(2), 124–136.
Zenios SA (1999) Modeling the transplant waiting list: a queueing model with reneging. Queueing Systems 31(3–4), 239–251.
Zenios SA and Wein LM (2000) Dynamic allocation of kidneys to candidates on the transplant waiting list. Operations Research 48(4), 549–569.
Zhang Y, Berman O and Verter V (2009) Incorporating congestion in preventive healthcare facility network design. European Journal of Operational Research 198(3), 922–935.
Zhang Y and Puterman ML (2013) Developing an adaptive policy for long-term care capacity planning. Health Care Management Science 16(3), 271–279.
Zhang Y, Puterman ML, Nelson N and Atkins D (2012) A simulation optimization approach to long-term care capacity planning. Operations Research 60(2), 249–261.
Acknowledgements
This research was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care North Thames at Barts Health NHS Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. The first author was supported by the Health Foundation as part of the Improvement Science PhD programme. The Health Foundation is an independent charity committed to bringing about better health and healthcare for people in the UK.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is licensed under a Creative Commons Attribution-NonCommercial- NoDerivs 3.0 Unported License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/.
The online version of this article is available Open Access.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Palmer, R., Fulop, N.J. & Utley, M. A systematic literature review of operational research methods for modelling patient flow and outcomes within community healthcare and other settings. Health Syst (2017). https://doi.org/10.1057/s41306-017-0024-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41306-017-0024-9