The outcome of the world, the gates of the future, and the entry into the super-human – these are not thrown open to a few of the privileged nor to one chosen people to the exclusion of all others. They will open only to an advance of all together, in a direction in which all together can join and find completion in a spiritual renovation of the earth….
Pierre Teilhard de Chardin, The Phenomenon of Man, 1955.
Abstract
Imagine a world in which every human being is healthy until the last breath. Thanks to the fast penetration of digital technologies in every region of the planet, this seemingly utopian scenario is not only feasible but also potentially viable. Now that digital technologies have provided almost full interconnectivity among all humans, they should be used to meet key challenges to ensure that health is created and that it spreads to reach every person on earth. The objective of this article is to describe and trigger a serious discussion of such challenges, which include: adopting a new concept of health; positioning self-rated health as the main outcome of the system; creating a health-oriented model to guide service provision; facilitating the identification, scaling up, and sustaining of innovations that can create and spread health; promoting a culture of health promotion; and encouraging the emergence of Precision Health. Once these challenges are met, and health becomes pandemic, public health would have fulfilled its vision, a healthy life for all, at last.
Similar content being viewed by others
Imagine a world in which every human being is healthy until the last breath…
This sentence might evoke a utopian scenario. In reality, however, it describes what would happen if public health could reach its full potential and realize its vision: health for all as part of a flourishing planet.1,2
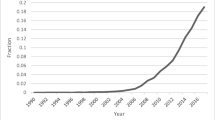
Thanks to the fast penetration of digital technologies in every region of the planet, 95 per cent of people in the world had access to a mobile phone by the end of 2015,3 and within a few years, everyone on earth will have access to the Internet.4 This level of interconnectivity, which has transformed practically all humans into nodes (“humanodes”) of a global superorganism,5 makes a pandemic of health, perhaps for the first time in history, not only feasible but also potentially viable.
At first glance, the use of the word “pandemic” might seem out of place. After all, it is almost always used in relation to the spread of diseases throughout the world. Etymologically, however, the word pandemic comes from the Greek terms pan and demos, which mean all, and people, respectively.6
Building on the unprecedented level of interconnectivity that they have created among humans, digital technologies must now be used to meet a few major challenges to ensure that every person on earth could experience good health.
Challenge #1: To Adopt a New Concept of Health
For a pandemic of health to occur, it will be necessary to conceptualize the term “health” in such a way that it would create the conditions for every person to be healthy, even in the presence of disease. This is now possible.
In 2008, with support from the entire online toolkit of the British Medical Journal (BMJ), a global conversation was ignited7 to challenge the definition of health used by the World Health Organization since its birth in 1948. The motivation behind the conversation was the recognition that such a definition, which remains unmodified in 60 years, condemned humans to be “not healthy”,8 as it is practically impossible for anyone to be in “a state of complete physical, mental and social well-being”.9 Even a person who is tired, wears glasses, or has dental caries could not be regarded as healthy.10
Three years later, following a dedicated meeting in The Hague, the BMJ published the proposal for a conceptualization that resulted from the conversation. This conceptualization considers health to be the “ability to adapt and self-manage” when individuals or communities face physical, mental, or social challenges.11 This approach helps explain how most people who live with multiple chronic diseases, or even with terminal diseases could still consider themselves to be healthy.12 The question now is how digital technologies could be used to mobilize the assets individuals and communities have at their disposal13 to elevate the status for those who do not feel healthy, while protecting those who already consider their health to be good or better.
For digital technologies to enable the adoption of a true concept of health, other powerful interventions, particularly in the economic and political domains, would need to be implemented first, to reverse the heavy level of medicalization (or “pathologization”) of our modern society. Such interventions, perhaps aided by digital technologies, would need to create new incentives for practically every group of stakeholders except for patients and staunch proponents of health promotion, to propel society towards salutogenesis.14 This will not be easy, given the extent to which most activities and careers are currently rewarded, while feeding a veritable, almighty medical-industrial complex.15
Challenge #2: To Make Health the Top Indicator
Most of the established so-called health indicators in use today do not really focus on health itself. Of the 100 “core health indicators” proposed by the WHO, for instance, 27 are included in the “health status” category. Of these, 25 relate to mortality or morbidity, and two to fertility. The remaining 73 indicators address risk factors for diseases (n = 21), healthcare service coverage (n = 27), or health system (n = 27) issues that focus on mortality, morbidity, access to services, workforce, information management, or financing.16
The pandemic of health requires a different approach, one that is guided by what could be called “salutometrics” (from Latin salus, meaning “health”), or indicators that focus on the true assessment of health. These could complement, enrich, or even replace many of the traditional disease-related variables.
In fact, self-rated health assessments could easily be placed at the top of the list, as they are easy to obtain, have shown great validity and predictive power, and align well with the new conceptualization of health. This indicator is at the core of a large population-based body of research showing that most humans who have been involved in national-level surveys report their health to be good or better than good.17 The corollary is that anyone could aspire to be healthy, making a pandemic of health possible.
Thanks to the widespread availability of mobile telephones, it would be relatively easy now to enable people to gather data by themselves, allowing them to express how they actually feel about their own health, anywhere and at any time, while matching any level of privacy, confidentiality, or anonymity they choose to have. The liberating power of mobile technologies would thus open new avenues for the generation and analysis of continuous streams of data in “real-enough-time”, yielding highly dynamic pictures of people’s health, individually and collectively, from the hyper-local to the global level.
Challenge #3: To Create a New Model of Health-Focused Service Provision
Just as the meaning of health and its assessment have been dominated by a disease-centric approach, most health services are provided within the context of “disease care systems”. Calling them “systems” is a misnomer, as they work more like a disjointed franchise of inefficient repair shops, offering services to the public along dysfunctional production lines operated by people who are increasingly at risk of behaving like robots. As a result, most of the resources available are consumed by activities designed to diagnose and fix problems that are largely unfixable, given that most of the workload relates to the management of chronic conditions, which by definition are incurable.
A new, genuine, health-focused model for service provision should incorporate a comprehensive menu of services designed to allow any person in the community to feel healthy. Such services would be supported by health-oriented insurance, management, financing, and evaluation modules, and would aim at preventing the preventable, curing the curable, relieving the relievable, controlling the controllable, and transcending the inevitable, while always accompanying people.
For the model to achieve these goals, existing electronic health records would need to morph into platforms able to capture and monitor data on self-reported health at all points of interactions with the public, and to guide service providers and recipients to the services that are best suited to meet their needs, regardless of where or who they are. Such platforms should also be connected and feed reward systems designed to reinforce behaviours that lead to the creation or maintenance of good health.
Challenge #4: To Identify and Exchange Knowledge About Effective Innovations That Promote the Creation and Spread of Health
Most successful efforts showing that it is possible to create and spread health remain like islands in a global archipelago of innovation, often unknown beyond the limited geographic area in which they have been developed and implemented.
Digital technologies—particularly in the form of an ecosystem of global open source knowledge management resources—could enable the innovators behind such breakthroughs to make their work visible to interested people from around the world, and to engage in collaborative efforts, efficiently, across geographic and institutional boundaries. Such ecosystems should include, as a minimum, a powerful database to store the information about the innovations; an accounts system and validated service fields that innovators could use to update their information directly and autonomously; tools to allow system administrators to vet, approve, or blacklist services; multiple search capabilities; easy-to-share content, free of cost; and a strong set of easy-to-deploy measures to punish or deter those who misuse sensitive personal data.
Challenge #5: To Scale and Sustain Successful Initiatives
Today, adopting or adapting proven innovations in settings other than those in which they were developed originally is extraordinarily time-consuming. Even if and when it occurs, scaling up any effort to a global level, and sustaining it over time, is practically impossible. One of the main impediments is the lack of organizations within the traditional health system with the mandate to promote, support, or fund the global implementation of disruptive health-creating initiatives. There is even less support, of any kind, to sustain such efforts over long periods of time. As a result, most innovations have very limited impact, both in time and space.
As this picture is unlikely to change in the foreseeable future, perhaps the only available way to multiply and sustain effective health-creating innovations is in the hands of existing large global digital data organizations, particularly those with an apparently altruistic nature, such as Wikipedia. More realistically, scaling and sustaining successful innovations might only happen through the creation of entirely new social business models that do not require the end users to pay for their services, which are immune to the chronic financial woes plaguing healthcare systems the world over, and which are designed, deliberately, to activate and unleash millions of human and technological vectors to fuel the pandemic of health.
Challenge #6: To Promote a Culture of Health Promotion
In 1986, the Ottawa Health Charter called for international efforts to achieve “health for all” by the year 2000, through health promotion activities that were meant to enable people to gain control over their lives and to improve their health.18 Sadly, the Charter had little impact. Instead, the pace of medicalization (or “pathologization”) of society has accelerated relentlessly all over the world, to the point that now almost every physical, mental, or social challenge faced by humans could easily be considered as a condition to be corrected through medical means.19
The time may have come for the health promotion community to step up their efforts and unleash the large-scale transformative movement that was meant to follow the launch of the Ottawa Health Charter. Digital technologies, and particularly online public engagement platforms,20 could play a major role in mobilizing and motivating people to pay more attention to what causes health, as opposed to what causes disease.21 Thanks to such powerful tools, it would be relatively easy to bring to reality the large-scale movement that was expected to follow the launch of the Ottawa Health Charter and to redress the power structures feeding most of the inequities in health status.22
Challenge #7: To Foster Precision Health
Precision Medicine promises to revolutionize healthcare through the recognition that each patient is unique from a biological perspective. This notion, which goes back thousands of years, now relies on breakthroughs from research on genomics, proteomics, metabolomics, and microbiomics to identify and correct the unique abnormalities affecting each individual patient.23 Analogously, there is an opportunity for the emergence of what could be called Precision Health. Such an approach would involve an explicit acknowledgement of the uniqueness of each person in terms of the capacity to adapt and self-manage when facing physical, mental, or social challenges, and effective means to mobilize the best available resources in the world to boost it.
For Precision Health to work, as it is the case with Precision Medicine, digital technologies will be essential to fuel the massive individualization required to make it part of day-to-day reality. Social networking tools, such as those offered by applications designed to help people access services to meet their needs (e.g. book a table at a restaurant, make a flight reservation, and find a date), could be easily adapted to allow people to make explicit their unique characteristics in terms of self-reported health, as well as their values, preferences, circumstances, incentives, and goals. Once individual profiles are created, they could be matched with the most compatible assets in their communities with which they could maintain or achieve good levels of health.
Many people might feel that these challenges are insurmountable. However, just a few decades ago it was thought landing safely on the moon or decoding the human genome was impossible. With relatively primitive tools, but with leadership, clear vision, conviction, and painstaking work, we proved ourselves wrong. Now, armed with digital tools of unimaginable and ever increasing power, we must believe that we can have a health system that allows us all to feel healthy until our last breath, and with a strong sense of urgency, prove ourselves right.
Editors' Note
This article is one of eight commissioned articles in a Special Sponsored Issue of the Journal of Public Health Policy in 2016, The Use and Impact of Digital Technologies on Population Health and Health Equity Gains .
References
Jadad, A.R. (2014) Let’s create a pandemic of health, together. Women’s College Research Institute Development Rounds. http://www.womensresearch.ca/publications/news/alex-jadad-wcri-research-development-rounds, accessed 14 February 2014.
Kotha, R. Jadad, A.R. and Hu, H. (2014) Creating a pandemic of health: Opportunities and lessons for a university initiative at the intersection of health, equity and innovation. Harvard Public Health Review 5. http://harvardpublichealthreview.org/wp-content/uploads/2015/04/HPHRv5-Kotha-Jadad-Hu-Creating-a-Pandemic.pdf.
Sanou, M. (2015) The World in 2015: ICT Facts and Figures. International Telecommunication Union. https://www.itu.int/en/ITU-D/Statistics/Documents/facts/ICTFactsFigures2015.pdf.
Jadad, A,R. and Enkin, M.W. (2007) Computers: Transcending our limits. In Medical Milestones: Celebrating Key Advances since 1840. BMJ 334(suppl): s8. http://ocw.tudelft.nl/fileadmin/ocw/courses/PublicHygieneandEpidemiology/res00025/!303420424d4a323030375f4d65646963616c4d696c6573746f6e6573.pdf.
Pandemic. Online Etymological Dictionary. http://www.etymonline.com/index.php?term=pandemic.
Jadad, A.R. and O’Grady, L. (2008) How should health be defined? BMJ. http://www.bmj.com/cgi/content/full/337/dec10_1/a2900.
Jadad, A.R. and O’Grady, L. (2008) A global conversation on defining health. BMJ Group Blogs. http://blogs.bmj.com/bmj/2008/12/10/alex-jadad-on-defining-health/#comments.
United Nations. Constitution of the World Health Organization. www.who.int/governance/eb/who_constitution_en.pdf.
Gurnani, M.V. and Agarwal, A. (2015) Healthy lives for all, until the last breath: An interview with Dr. Alex Jadad. University of Toronto Medical Journal 92: 20–24.
Huber, M., Knottnerus, J.A., Green, L., Horst, H., Jadad, A.R., Kromhout, D., Leonard, B., Lorig, K., Loureiro, M.I., Meer, J.W., Schnabel, P., Smith, R., Weel, C. and Smid, H. (2011) How should we define health? BMJ 343: d4163.
Vögele, C. (2013) On living a long, healthy, and happy life, full of love, and with no regrets, until our last breath: An interview with Alejandro R Jadad. Verhaltenstherapie 23: 287–289.
McLean, J. (2011) Asset based approaches for health improvement: Redressing the balance. Glasgow Centre for Population Health. Briefing paper 9. www.gcph.co.uk/assets/0000/2627/GCPH_Briefing_Paper_CS9web.pdf.
McLean J. (2011) Asset based approaches for health improvement: redressing the balance. Glasgow Centre for Population Health. Briefing paper 9. www.gcph.co.uk/assets/0000/2627/GCPH_Briefing_Paper_CS9web.pdf.
Relman, A.S. (1980) The new medical-industrial complex. New England Journal of Medicine 303: 963–970.
World Health Organization. (2015) Global Reference List of 100 Core Health Indicators. http://www.who.int/healthinfo/indicators/2015/en/.
World Health Survey. (2003) Geneva: World Health Organization (WHO).
World Health Organization. (1986) The Ottawa Charter for Health Promotion. http://www.who.int/healthpromotion/conferences/previous/ottawa/en/.
Conrad, P. (2007) The Medicalization of Society: On the Transformation of Human Conditions into Treatable Disorders. Baltimore: Johns Hopkins University Press.
Horose C. (2015) Let’s get digital! 50 tools for onine public engagement. Community Matters. http://www.communitymatters.org/blog/let%E2%80%99s-get-digital-50-tools-online-public-engagement.
Antonovsky, A. (1996) The salutogenic model as a theory to guide health promotion. Health Promotion International 11: 11–18.
Taylor, C., O’Hara, L. and Barnes, M. (2014) Health promotion: A critical salutogenic science. International Journal of Social Work and Human Services Practice 2: 283–290.
Collins, F.S. and Varmus, H. (2015) A new initiative on precision medicine. New England Journal of Medicine 372: 793–795.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is licensed under a Creative Commons Attribution 3.0 Unported License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/3.0/
The online version of this article is available Open Access
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jadad, A.R. Creating a pandemic of health: What is the role of digital technologies?. J Public Health Pol 37 (Suppl 2), 260–268 (2016). https://doi.org/10.1057/s41271-016-0016-1
Published:
Issue Date:
DOI: https://doi.org/10.1057/s41271-016-0016-1