Abstract
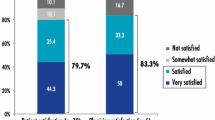
Photodynamic therapy (PDT) is an attractive treatment option for skin diseases such as actinic keratosis, since large skin areas can be treated with high response rates and good cosmetic outcomes. Nevertheless inflammation and pain are still major side effects. The aim of this study was to investigate the extent to which less time-consuming PDT treatment regimens using methyl aminolevulinate (MAL) decrease protoporphyrin IX (PpIX) photobleaching, inflammation and pain. Twenty-four healthy volunteers were treated with 4 different interventions on each forearm. All 8 fields were tape-stripped 10 times. On the right arm MAL was applied for 20, 40, 60 or 180 min, followed by further incubation after wiping off MAL until 180 min after start and then illuminating with red light 180 min after start. On the left arm MAL or vehicle was applied for 30, 60, or 90 min and illuminated immediately after MAL removal. PpIX fluorescence, photobleaching, objective and subjective erythema (as a measure for inflammation), pigmentation and pain were measured. The results showed a significant correlation between incubation time, time until illumination and photobleaching. Furthermore, there was a significant correlation between photobleaching and erythema and also between photobleaching and pain. In conclusion, shorter PDT regimens result in decreased photobleaching and also less inflammation and pain. We hypothesize that a shorter incubation time is important for the optimal specific subcellular distribution of PpIX and to avoid unspecific distribution. We propose a shorter PDT regimen, “Pulse PDT”, comprising, for example 30 min incubation with MAL and illumination after 180 min, and we have planned a study of actinic keratosis and “Pulse PDT”.
Similar content being viewed by others
References
P. Babilas, S. Schreml, M. Landthaler and R. M. Szeimies, Photodynamic therapy in dermatology: state-of-the-art, Photodermatol., Photoimmunol. Photomed., 2010, 26(3), 118–132.
L. R. Braathen, R. M. Szeimies, N. Basset-Seguin, R. Bissonnette, P. Foley, D. Pariser, R. Roelandts, A. M. Wennberg and C. A. Morton, Guidelines on the use of photodynamic therapy for nonmelanoma skin cancer: an international consensus. International Society for Photodynamic Therapy in Dermatology, 2005, J. Am. Acad. Dermatol., 2007, 56(1), 125–143.
L. R. Braathen, B. E. Paredes, O. Saksela, C. Fritsch, K. Gardlo, T. Morken, K. W. Frolich, T. Warloe, A. M. Soler and A. M. Ros, Short incubation with methyl aminolevulinate for photodynamic therapy of actinic keratoses, J. Eur. Acad. Dermatol. Venereol., 2009, 23(5), 550–555.
D. Touma, M. Yaar, S. Whitehead, N. Konnikov and B. A. Gilchrest, A trial of short incubation, broad-area photodynamic therapy for facial actinic keratoses and diffuse photodamage, Arch. Dermatol., 2004, 140(1), 33–40.
S. Smith, D. Piacquadio, V. Morhenn, D. Atkin and R. Fitzpatrick, Short incubation PDT versus 5-FU in treating actinic keratoses, J. Drugs Dermatol., 2003, 2(6), 629–635.
F. Piffaretti, M. Zellweger, B. Kasraee, J. Barge, D. Salomon, H. van den Bergh and G. Wagnieres, Correlation between protoporphyrin IX fluorescence intensity, photobleaching, pain and clinical outcome of actinic keratosis treated by photodynamic therapy, Dermatology, 2013, 227(3), 214–225.
B. Krammer and K. Uberriegler, In vitro investigation of ALA-induced protoporphyrin IX, J. Photochem. Photobiol., B, 1996, 36(2), 121–126.
J. E. Mateus, W. Valdivieso, I. P. Hernandez, F. Martinez, E. Paez and P. Escobar, Cell accumulation and antileishmanial effect of exogenous and endogenous protoporphyrin IX after photodynamic treatment, Biomedica, 2014, 34(4), 589–597.
S. Shahzidi, B. Cunderlikova, A. Wiedlocha, Y. Zhen, V. Vasovic, J. M. Nesland and Q. Peng, Simultaneously targeting mitochondria and endoplasmic reticulum by photodynamic therapy induces apoptosis in human lymphoma cells, Photochem. Photobiol. Sci., 2011, 10(11), 1773–1782.
A. Juzeniene, P. Juzenas, L. W. Ma, V. Iani and J. Moan, Topical application of 5-aminolaevulinic acid, methyl 5-aminolaevulinate and hexyl 5-aminolaevulinate on normal human skin, Br. J. Dermatol., 2006, 155(4), 791–799.
S. Fabricius, C. M. Lerche, P. A. Philipsen and H. C. Wulf, The relation between methyl aminolevulinate concentration and inflammation after photodynamic therapy in healthy volunteers, Photochem. Photobiol. Sci., 2013, 12(1), 117–123.
S. R. Wiegell, I. M. Stender, R. Na and H. C. Wulf, Pain associated with photodynamic therapy using 5-aminolevulinic acid or 5-aminolevulinic acid methylester on tape-stripped normal skin, Arch. Dermatol., 2003, 139(9), 1173–1177.
S. R. Wiegell, B. Petersen and H. C. Wulf, Topical corticosteroid reduces inflammation without compromising the efficacy of photodynamic therapy for actinic keratoses: a randomized clinical trial, Br. J. Dermatol., 2014, 171(6), 1487–1492.
E. Angell-Petersen, R. Sorensen, T. Warloe, A. M. Soler, J. Moan, Q. Peng and K. E. Giercksky, Porphyrin formation in actinic keratosis and basal cell carcinoma after topical application of methyl 5-aminolevulinate, J. Invest. Dermatol., 2006, 126(2), 265–271.
R. Na, I. M. Stender, M. Henriksen and H. C. Wulf, Autofluorescence of human skin is age-related after correction for skin pigmentation and redness, J. Invest. Dermatol., 2001, 116(4), 536–540.
H. C. Wulf, Methods and an apparatus for determining an individual’s ability to stand ultraviolet radiation, US Patent, 4882598,1986.
S. R. Wiegell, J. Skiveren, P. A. Philipsen and H. C. Wulf, Pain during photodynamic therapy is associated with protoporphyrin IX fluorescence and fluence rate, Br. J. Dermatol., 2008, 158(4), 727–733.
S. R. Wiegell, M. Haedersdal and H. C. Wulf, Cold water and pauses in illumination reduces pain during photodynamic therapy: a randomized clinical study, Acta Derm. -Venereol., 2009, 89(2), 145–149.
B. R. Kirkwood, Essentials of medical statistics, Blackwell Science Ltd, 2nd edn,2003.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lerche, C.M., Fabricius, S., Philipsen, P.A. et al. Correlation between treatment time, photobleaching, inflammation and pain after photodynamic therapy with methyl aminolevulinate on tape-stripped skin in healthy volunteers. Photochem Photobiol Sci 14, 875–882 (2015). https://doi.org/10.1039/c5pp00069f
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1039/c5pp00069f