Abstract
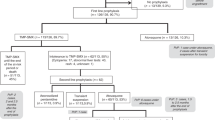
Pneumonia due to Pneumocystis carinii is an infrequent complication following autologous stem cell transplantation (ASCT) which is associated with a high mortality. Although administration of trimethoprim/sulfa- methoxazole (TMP/SMX) is an effective prophylactic strategy for Pneumocystis carinii pneumonia (PCP), treatment-associated toxicity frequently results in discontinuation of therapy. We have conducted a prospective randomized trial comparing atovaquone, a new anti-Pneumocystis agent, with TMP/SMX for PCP prophylaxis following autologous peripheral blood stem cell (PBSC) transplantation. Thirty-nine patients were studied. Twenty patients received atovaquone suspension and 19 patients received TMP/SMX. The median ages were 44 (range 20–68) and 47 (range 32–63) years, respectively. A similar number of patients with solid tumors (14 vs 15) and hematologic malignancies (five vs five) were treated in each group. Either TMP/SMX (160/800 mg) or atovaquone (1500 mg) was administered daily from transplant day −5 until day −1, discontinued from day 0 to engraftment, then resumed 3 days per week until day +100 post-transplant. The median time to engraftment (ANC >0.5 × 109/l) was similar in both groups. Eighty percent of the patients randomized to atovaquone prophylaxis completed the study. Four atovaquone-treated patients were removed from study; two patients (10%) did not receive a transplant and two patients (10%) were removed due to a protocol violation. None of the 16 patients treated with atovaquone experienced treatment-associated adverse effects. Of the 19 patients randomized to receive TMP/SMX, 55% completed the study. Nine TMP/SMX-treated patients were removed from the study; one patient (5%) did not receive a transplant and eight patients (40%) were removed due to drug intolerance (P < 0.003). the rate of intolerance to tmp/smx led to the early discontinuation of this randomized trial. intolerance of tmp/smx included elevated transaminase levels (n = 1), nausea or vomiting (n = 3), thrombocytopenia (n = 2) and neutropenia (n = 2). All episodes of TMP/SMP intolerance occurred following transplantation after a median duration of 17.5 (range 2–48) days and a median of 7 (range 1–20) doses. Resolution of adverse side-effects occurred in all eight patients within a median of 7 (range 2–20) days following discontinuation of therapy. Neither PCP nor bacterial infections were identified in any of the patients treated. This prospective randomized study demonstrated that atovaquone is well-tolerated for anti-Pneumocystis prophylaxis in autologous PBSC transplant patients intolerant of TMP/SMX.
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Colby, C., McAfee, S., Sackstein, R. et al. A prospective randomized trial comparing the toxicity and safety of atovaquone with trimethoprim/sulfamethoxazole as Pneumocystis carinii pneumonia prophylaxis following autologous peripheral blood stem cell transplantation. Bone Marrow Transplant 24, 897–902 (1999). https://doi.org/10.1038/sj.bmt.1702004
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1702004
- Springer Nature Limited
Keywords
This article is cited by
-
Feasibility of trimethoprim/sulfamethoxazole desensitization therapy in hematological diseases
Clinical and Experimental Medicine (2022)
-
Comparative effectiveness of trimethoprim-sulfamethoxazole versus atovaquone for the prophylaxis of pneumocystis pneumonia in patients with connective tissue diseases receiving prolonged high-dose glucocorticoids
Rheumatology International (2022)
-
Primary prophylaxis of bacterial infections and Pneumocystis jirovecii pneumonia in patients with hematologic malignancies and solid tumors: 2020 updated guidelines of the Infectious Diseases Working Party of the German Society of Hematology and Medical Oncology (AGIHO/DGHO)
Annals of Hematology (2021)
-
Radiation pneumonitis complicated by Pneumocystis carinii in patients with thoracic neoplasia: a clinical analysis of 7 cases
Cancer Communications (2019)
-
Management of infection and febrile neutropenia in patients with solid cancer
Clinical and Translational Oncology (2016)