Abstract
The objectives of this study were to investigate the variable factors associated with cognitive function and cortical atrophy and estimated variable importance of those factors in affecting cognitive function and cortical atrophy in patients with EOAD and LOAD. Patients with EOAD (n = 40), LOAD (n = 34), and healthy volunteers with normal cognition were included (n = 65). All of them performed 3T MRI, [18F]THK5351 PET (THK), [18F]flutemetamol PET (FLUTE), and detailed neuropsychological tests. To investigate factors associated with neuropsychological test results and cortical thickness in each group, we conducted multivariable linear regression models, including amyloid, tau, cerebral small vessel disease markers on MRI, and vascular risk factors. Then, we estimated variable importance in associating cognitive functions and cortical thickness, using relative importance analysis. In patients with EOAD, global THK retention was the most important contributor to the model variances for most neuropsychological tests, except for memory. However, in patients with LOAD, multiple contributors beyond tau were important in explaining variance of neuropsychological tests. In analyses with mean cortical thickness, global THK retention was the main contributor in patients with EOAD, while in LOAD patients, multiple factors contributed equally to mean cortical thickness. Therefore, EOAD and LOAD may have different pathomechanistic courses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Alzheimer’s disease (AD) is the most common type of dementia, marked by the presence of amyloid-beta (Aβ) and tau pathologies1. The risk of AD increases with age, and AD mainly affects people over age 65; the development of AD in individuals 65 or older is called late-onset AD (LOAD). However, up to 5% of AD patients are early-onset AD (EOAD) patients who develop dementia symptoms prior to age 652. Depending on the age of onset, there are significant differences in the neurodegenerative and clinical patterns exhibited by AD patients. Even in early stages of disease, EOAD patients tend to show more widespread and greater cortical atrophy, while LOAD patients tend to show cortical atrophy relatively confined to medial temporal regions3,4. Compared to LOAD, which predominantly presents with amnestic deficits, EOAD patients show greater deficits in non-amnestic domains and have a more rapidly deteriorating course5,6.
Although Aβ and tau underlie both types of AD, existing evidence suggests that the distribution or burden of Aβ and tau are quite different between EOAD and LOAD7,8,9. In addition, there might be a difference between EOAD and LOAD in the relative contribution of Aβ and tau to patients’ neurodegeneration and cognitive decline. Our previous study showed that only [18F]-THK 5351 (THK) retention, which reflects tau pathology and related astrogliosis, had a significant effect on white matter (WM) connectivity disruption10. This tau-related disruption was strongly correlated with cognitive dysfunction in EOAD, but such a dominant effect of tau-related disruption was not observed in LOAD10. Compared to EOAD, LOAD is considered to be influenced by more diverse factors including the aging process and vascular pathology11. Several previous studies have also shown the role of vascular risk factors in the development or progression of LOAD12,13,14. However, to our knowledge, no study has compared the relative contribution of AD pathology, vascular pathology, and vascular risk factors between EOAD and LOAD. Therefore, we investigated and compared the effects and relative importance of AD pathology (Aβ and tau), vascular pathologies and vascular risk factors on cortical thickness and cognitive impairment in EOAD and LOAD to identify the different pathomechanisms between EOAD and LOAD in more depth.
Methods
Participants
We recruited a total number of 177 participants including 103 patients with AD, and 74 cognitively unimpaired (CU) participants. Participants underwent THK and [18F]-flutemetamol (FLUTE) PET scans, 3.0-Tesla MRI, and detailed neuropsychological tests at the Memory Clinic at Gachon University Gil Medical Center. Of the 177 participants screened for this study, 12 participants with unsuitable data due to motion artifact were excluded. We additionally excluded 26 participants who did not complete the full neuropsychological battery. We thus included in analyses 139 participants (n = 40 EOAD; n = 34 LOAD, n = 65 CU). All patients with AD dementia had been diagnosed with the probable AD according to the National Institute of Neurological and Communicative Disorders and Stroke and the AD and Related Disorders Association15, and diagnoses were confirmed by follow-up for more than 1 year at the outpatient clinics. EOAD was defined as AD patients whose onset age was younger than 65 years old, while LOAD was defined as age of onset older than 65 years old. We excluded patients with severe white matter hyperintensities (WMH) on MRI, defined as a cap or a band > = 10 mm wide, as well as deep WMH > = 25 mm in length, as modified from the Fazekas ischemia criteria16,17. Patients with other structural lesions on brain MRI such as territorial infarction, intracranial hemorrhage, traumatic brain injury, hydrocephalus, severe WMH or WMH associated with radiation, multiple sclerosis, or vasculitis were excluded from this study. All participants completed a clinical interview and underwent a standardized neuropsychological examination.
Detailed test items of the neuropsychological examinations and aphasia battery are presented in Supplementary Text-1. Secondary causes of dementia were ruled out through laboratory tests assessing complete blood counts, vitamin B12, folate levels, thyroid function, metabolic profile, and syphilis serology. APOE genotyping was also performed. The CU control group was comprised of 65 healthy volunteers with no neurological or psychiatric illnesses, and no abnormalities detected on neurologic examination. The CU group had a Clinical Dementia Rating (CDR) score of 0, and normal cognitive function determined using neuropsychological tests (defined as within 1.5 standard deviations of the age- and education-corrected normative mean). CU participants did not have any structural lesions on brain MRI such as cerebral infarction, intracranial hemorrhage, traumatic brain injury, hydrocephalus, or severe WMH. They were either family members of the patients at the Memory Disorder Clinic of Gil Medical Center or volunteers from the community. For the comparison with the EOAD or LOAD groups, CU subjects were divided into age-matched control groups comprising 33 young controls (YC) (mean age: 57.6 years old) and 32 old controls (OC) (mean age: 74.4 years old).
Written informed consent was obtained from all participants and the study was approved by the Institutional Review Board of Gachon University Gil Medical Center. Research was conducted in accordance with the Declaration of Helsinki.
MR image acquisition and parcellation
MR images of all subjects were obtained using 3.0 Tesla MR scanner (Verio, Siemens, Erlangen, Germany) at Gil medical Center. 3D T1-MPRAGE was acquired using the following parameters: repetition time = 1900 ms, echo time = 2.93 ms, flip angle = 8°, pixel bandwidth = 170 Hz/pixel, matrix size = 256 × 208, field of view = 256 mm, NEX = 1, total acquisition time = 4 min 10 s, and 0.5 × 0.5 × 1.0 mm3 voxels. The FLAIR imaging parameters used were as follows: repetition time = 9000 ms, echo time = 122 ms, flip angle = 150°, pixel bandwidth = 287 Hz/pixel, matrix size = 256 × 224, field of view = 256 mm, NEX = 1, slice thickness = 2 mm, total acquisition time = 2 min 44 s. The SWI imaging parameters used were as follows: repetition time = 27 ms, echo time = 20 ms, flip angle = 15°, pixel bandwidth = 120 Hz/pixel, matrix size = 256 × 224, field of view = 256 mm, NEX = 1, slice thickness = 2 mm, total acquisition time = 4 min 27 s. T2-weighted imaging parameters used were as follows: repetition time = 9650 ms, echo time = 88 ms, flip angle = 120°, pixel bandwidth = 174 Hz/pixel, matrix size = 256 × 224, field of view = 256 mm, NEX = 1, slice thickness = 4 mm, total acquisition time = 3 min 03 s. Assessment of lacunes and cerebral microbleeds (CMBs) on MRI are described in Supplementary Text-2. WMH volume was calculated using FLAIR images. Images were analyzed using FreeSurfer 6.0 (www.surfer.nmr.mgh.harvard.edu), with ROIs for regional cortical thickness determined using the Desikan-Killiany Atlas (supplementary table 1).
To calculate surface-based cortical thickness, we first constructed the outer and inner cortical surface meshes from the MR volume of each subject. The two meshes are isomorphic with the same vertices and connectivity because the outer surface is constructed by deforming the inner surface. In order to establish correspondence between subjects, we resampled each subject’s cortical surface to 40,962 vertices for each hemisphere. The vertex-wise cortical thickness at each vertex was defined as the distance between the two surfaces at the vertex. We used a cortical thickness w-score in order to standardize cortical thickness values on the distribution of normal values. W-score was calculated using each age-matched CU group by the method previously described18.
PET data acquisition
All PET scans were acquired with a Siemens Biograph 6 Truepoint PET/computed tomography (CT) scanner (Siemens, Erlangen, Germany) with a list-mode emission acquisition. THK was synthesized and radiolabeled at Gachon University Neuroscience Research Institute. All participants underwent a 20-min emission scan starting 50 min after 185 MBq of THK was injected intravenously (50–70 min) and a 20-min emission scan starting 90 min after the intravenous injection of 185 MBq of FLUTE (90–110 min), which was purchased from Carecamp Inc. and radiolabeled at the Gachon University Neuroscience Research Institute. A low-dose CT was performed for attenuation correction prior to all scans. In participants who underwent THK and FLUTE PET scans, the mean intervals between THK PET and FLUTE PET scans was 10 days. FLUTE PET and MRI scans were acquired on the same day. Individual static images were reconstructed onto a 256 × 256 × 109 matrix with a voxel size of 1.3 × 1.3 × 1.5 mm3 using a 2D ordered subset expectation maximization algorithm (8 iterations and 16 subsets), with corrections for physical effects.
PET imaging quantification
Each THK or FLUTE PET image was co-registered with the corresponding T1 image using FreeSurfer. Regional mean values of PET images were then extracted after region-based partial volume correction (PVC) using the PETSurfer tool in FreeSurfer19,20 and were weighted-averaged for pre-defined ROIs. ROIs include the prefrontal (frontal pole, pars orbitalis, lateral orbital frontal, pars triagularis, pars opercularis, rostral middle frontal, superior frontal, caudal middle frontal, and medial orbital frontal regions), orbitofrontal (lateral orbital frontal and medial orbital frontal regions), sensorimotor (pre-central, post-central, and paracentral regions), anterior cingulate (accumbens-area, caudal anterior cingulate, and rostral anterior cingulate regions), superior parietal, inferior parietal (inferior parietal and supramarginal regions), precuneus, posterior cingulate, occipital cortex (cuneus, pericalcarine, and lateral occipital regions), superior temporal, middle temporal, inferior temporal, mesial temporal (hippocampus, amygdala, parahippocampal and entorhinal cortices), entorhinal cortices, parahippocampus, hippocampus, amygdala, fusiform gyrus, lingual gyrus, striatum, and global retention. Global retention ratio of THK was calculated based on AD-related regions including the prefrontal, superior parietal, lateral temporal, inferior parietal, occipital, anterior cingulate, mesial temporal, precuneus, and posterior cingulate cortices. Regional standardized uptake value ratios (SUVRs) were calculated using cerebellar gray matter as the reference region for THK images21,22 and the pons for FLUTE images23. SUVR images were also generated from the MRI co-registered PET images with voxel-based PVC19,20. The global retention ratio of FLUTE was calculated based on AD-related regions including the frontal, parietal, lateral temporal, anterior and posterior cingulate cortices23. Patients were classified as amyloid positive based on visual reads in the frontal, temporal, parietal cortices, striatum, and precuneus.
Statistical analysis
Differences in characteristics, neuropsychological battery z-scores, and cortical thickness w-scores between patients with EOAD and LOAD were assessed using independent t-tests (for continuous variables) and chi-squared tests (for categorical variables). To investigate factors associated with neuropsychological test results (z-score) and cortical thickness in each group, we conducted multivariable linear regression models, including THK global retention, FLUTE global cortical retention, WMH volume, the numbers of CMBs and lacunes, and history of hypertension (HTN), diabetes mellitus (DM), coronary artery disease, dyslipidemia, and stroke. Age, gender, and educational year were additionally adjusted for in the MMSE and CDR-Sum of Boxes (SOB) analyses. Then, we estimated variable importance in associating neuropsychological battery z-scores and cortical thickness w-score, using relative importance analysis. Relative importance weight was depicted with histograms representing R2 of each variable contributing to total amount of variance explained (total R2). All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA) and R version 3.2.4 with relaimpo package24. In predicting cortical thickness using relative importance analysis, cortical thickness data was converted to w-score adjusting age, gender, and education years18. Relative importance of factors associated with regional cortical thickness in EOAD and LOAD was estimated by regional THK regional retention, FLUTE regional cortical retention, WMH volume, the numbers of CMBs and lacunes, and history of HTN, DM, coronary artery disease, dyslipidemia, and stroke in each ROIs.
Results
Characteristics of study subjects
A total of 40 individuals with EOAD and 34 with LOAD were included (Table 1). The mean ages were 59.7 (standard deviation [SD], 5.3) and 76.9 (6.0) years in the EOAD and LOAD groups, respectively. Women accounted for 32.5% (n = 13) in the EOAD group and 26.5% (n = 9) in the LOAD group. The proportions of those with HTN were 15.0% in the EOAD group and 41.2% in the LOAD group. All EOAD and LOAD patients were amyloid positive. The means of WMH volume were 3733.5 mL (SD, 2475.5) and 7848.7 mL (7045.4) in the EOAD and LOAD groups, respectively. Comparisons of clinical characteristics, neuropsychological test results and regional SUVR of THK PET between AD patients and each age-matched CU are presented in supplementary table 2–4.
Factors associated with neuropsychological test results
As shown in Table 2, in individuals with EOAD, the level of global THK retention was significantly associated with scores of MMSE (β = − 6.71, standard error [SE] = 1.61, p < 0.001), CDR-SOB (β = 2.25, SE = 0.67, p < 0.001), digit span forward (β = − 1.27, SE = 0.53, p = 0.02), digit span backward (β = − 1.53, SE = 0.43, p < 0.001), naming K-BNT (β = − 2.78, SE = 0.70, p < 0.001), RCFT copy (β = − 5.91, SE = 2.44, p = 0.02), COWAT animal (β = − 0.96, SE = 0.37, p = 0.01), and TMT-A (β = − 14.91, SE = 4.13, p < 0.001). The increased level of global FLUTE retention was significantly associated with increased CDR-SOB (β = 3.83, SE = 1.30, p = 0.01) and decreased digit span backward (β = − 2.26, SE = 0.78, p = 0.01), SVLT immediate recall (β = − 2.11, SE = 0.86, p = 0.02), RCFT immediate recall (β = − 1.64, SE = 0.64, p = 0.02), RCFT delayed recall (β = − 1.95, SE = 0.76, p = 0.02), COWAT animal (β = − 1.44, SE = 0.67, p = 0.04), and K-CWST color reading (β = − 2.80, SE = 0.96, p = 0.01). There were no significant associations between the other factors and neuropsychological test results except the associations of CMBs and DM with MMSE.
In individuals with LOAD, global FLUTE retention was significantly associated with scores of MMSE (β = − 18.52, SE = 6.24, p = 0.01), CDR-SOB (β = 7.76, SE = 2.99, p = 0.02), digit span forward (β = − 3.30, SE = 1.50, p = 0.04), digit span backward (β = − 6.14, SE = 1.55, p < 0.001), SVLT immediate recall (β = − 2.54, SE = 1.12, p = 0.03), RCFT recognition (β = − 5.22, SE = 2.16, p = 0.02), COWAT animal (β = − 3.42, SE = 1.00, p < 0.001), K-CWST color reading (β = − 3.03, SE = 1.19, p = 0.02), TMT-A (β = − 16.08, SE = 3.90, p < 0.001), and TMT-B (β = − 8.01, SE = 2.86, p = 0.01). Increased WMH volumes were significantly associated with decreased scores of COWAT animal (β = − 0.06, SE = 0.02, p = 0.02) and TMT-A (β = − 0.34, SE = 0.09, p < 0.001). Dyslipidemia was significantly associated with decreased scores of naming K-BNT (β = − 1.29, SE = 0.55, p = 0.03) and TMT-B (β = − 3.59, SE = 0.98, p < 0.001). The other factors were not significantly associated with decreased neuropsychological battery z-scores.
Relative importance of factors associated with neuropsychological test results
In individuals with EOAD, global THK retention was the most important contributor to the model variances in associating scores of MMSE, CDR-SOB, K-BNT, TMT-A, digit span forward, and COWAT-animal. In RCFT copy, digit span backward, and TMT-B, global THK retention and global FLUTE retention showed similar size of importance. Global FLUTE retention was most important in predicting scores of SVLT delayed recall and RCFT delayed recall only (Fig. 1).
Relative importance of factors associated with neuropsychological test results in EOAD and LOAD. In EOAD, global THK retention was the most important factor for MMSE, CDR-SOB, K-BNT, and TMT-A. Global FLUTE retention was crucial for SVLT delayed recall. In LOAD, global FLUTE retention contributed most to MMSE, CDR-SOB, and TMT-A. In the other neuropsychological tests, there were varied contributors which were most important in explaining variances. THK, global SUVR of [18F]THK-5351; FLUTE, global SUVR of [18F]flutemetamol; WMHV, white matter hyperintensities volumes; MB, cerebral microbleeds; HTN, hypertension; DM, diabetes mellitus; CAD, coronary artery disease; Stroke Hx, stroke history.
In individuals with LOAD, global FLUTE retention contributed most to the model variances in associating scores of digit span forward, digit span backward, COWAT animal, TMT-A, MMSE, and CDR-SOB. In the other neuropsychological tests, there were varied contributors which were most important in explaining variances (HTN in naming K-BNT, CMBs in RCFT copy, HTN in RCFT delayed recall, and dyslipidemia in TMT-B).
Relative importance of factors associated with cortical thickness
In individuals with EOAD, global THK retention was the most important contributor to the model variances in associating mean cortical thickness (Fig. 2A). FLUTE global cortical retention was second most important. Total R-squared was 65.26% in the EOAD group, and relative importance was 26.62% and 18.55% for THK global retention and FLUTE global cortical retention, respectively.
Relative importance of factors associated with mean cortical thickness in EOAD (A) and LOAD (B). In EOAD, global retention of THK was the key factors associated with mean cortical thickness followed by FLUTE retention. In LOAD, THK had minimal impact; lacune count was most important, along with CMBs, FLUTE retention, DM, and stroke history. THK, global SUVR of [18F]THK-5351; FLUTE, global SUVR of [18F]flutemetamol; WMHV, white matter hyperintensities volumes; HTN, hypertension; DM, diabetes mellitus; CAD, coronary artery disease; Stroke Hx, stroke history.
In individuals with LOAD, THK global region retention rarely contributed to the model variances in predicting mean cortical thickness; the number of lacunes had the largest relative importance (Fig. 2B). Heterogenous factors including number of CMBs, FLUTE retention, DM, and stroke history had similar relative importance. Total R-squared was 30.53%, with relative importance of the number of lacunes of 11.82%.
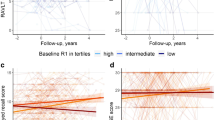
In regional analysis, the overall trend was similar to global analysis results (Fig. 3 and supplementary table 1). In the analysis of regional cortical thickness, regional THK retention was the variable with the most significant effect on cortical thickness in EOAD. The areas where the models had a lesser exploratory power and THK retention had a relatively smaller effect were mainly the primary motor, sensory, and visual cortices, as well as the anterior cingulate. On the other hand, the regions where the influence of THK retention was dominant were the AD signature areas. In contrast, in LOAD, various factors influenced regional cortical thickness.
Relative importance of factors associated with regional cortical thickness in EOAD (A) and LOAD (B). In EOAD, global retention of THK was the key factors associated with regional cortical thickness In LOAD, heterogenous factors were associated with regional cortical thickness. ROIs were described in supplementary table 1. THK, global SUVR of [18F]THK-5351; FLUTE, global SUVR of [18F]flutemetamol; WMHV, white matter hyperintensities volumes; HTN, hypertension; DM, diabetes mellitus; CAD, coronary artery disease; Stroke Hx, stroke history.
Discussion
In this study, we investigated and compared the effects and relative importance of AD pathology, vascular pathologies and vascular risk factors on cortical atrophy and cognitive impairment in EOAD and LOAD. We found that factors related to cortical thickness and cognitive function differed between EOAD and LOAD. In EOAD, tau (as measured by THK uptake) was a major factor related o cortical thickness and cognition. It is already well known that tau pathology is more closely related to neuronal loss and clinical symptoms compared to amyloid25. Aβ is known to be upstream of tau in AD pathology; Aβ triggers the formation of toxic tau, and the toxic form of tau causes neuronal death26. It is also reflected in the A/T/N classification system for AD biomarkers as well; amyloid (A) precedes tau (T) and neurodegeneration (N), which correlate with clinical symptoms27. In a previous tau PET study, EOAD patients showed tau pathology in more widespread neocortical regions than LOAD patients7. This distinct pattern of tau pathology has been considered a key factor of the atrophy pattern and clinical features of EOAD. The results of our study are also in line with previous data and support the fact that tau is a major contributor in EOAD. Tau pathology may lead to cognitive deficits through multiple mechanisms, not just cortical thinning. For example, in our previous study, tau was related to WM connectivity disruption in EOAD and this tau-related WM disruption showed a significant association with cognitive impairment except for memory10. Similarly, in this analysis, tau was a major contributor in most cognitive function measures in EOAD. However, the explanatory power for the cognitive items most affected by memory, such as SVLT delayed recall or RCFT delayed recall, was markedly lower than that for other cognitive measures, and the influence of amyloid was greater than that of tau. This may be because EOAD patients do not always follow the traditional Braak staging when tau pathology spreads and the medial temporal lobe, a region critical to memory function, is less affected and relatively spared by tau pathology in the early stage of EOAD28. For this reason, it is possible that Aβ pathology, which precedes tau pathology, appeared to have a greater effect than tau on memory function in this analysis. In our study, a significant number of EOAD patients were non-amnestic (7 out of 40 patients) or, even if they had memory decline, other cognitive functions deteriorated earlier (12 out of 40 patients).
In LOAD, there was no specific variable with predominance, and the model had lower explanatory power in the analysis of cortical thickness. This suggests that in LOAD, unlike EOAD where tau is a major contributor, more diverse degenerative and vascular factors beyond amyloid, tau, and cerebral small vessel disease included in our analysis may contribute to brain atrophy. Compared to EOAD, which occurs at a relatively young age, LOAD occurs at an advanced age and is likely to be influenced by the aging process. The incidence of vascular risk factors or vascular pathologies increases with age. It is well known that vascular risk factors influence the development or progression of AD12,13,14. One study showed that elevated vascular risk might influence tau burden when coupled with high Aβ burden, especially in temporal neocortical regions known to be affected early in LOAD29. Intra-brain vascular dysregulation has been suggested as an early pathological event in LOAD11. As several previous neuropathological studies have shown, vascular pathology frequently co-exists with AD pathology in the elderly30,31. Vascular pathology is known to lower the threshold of cognitive decline in a given AD pathology32 and interact with AD pathology33. Vascular dysfunction affects amyloid deposition by reducing amyloid clearance34, and amyloid also has a toxic effect on the cerebrovasculature35. Even without tau pathology, amyloid can cause neuronal dysfunction or cell death26,36 and vascular pathology itself also can cause cortical thinning37 or cognitive impairment38. In sum, cortical thinning and cognitive decline in LOAD are thought to be influenced by multiple, diverse factors rather than being predominantly determined by tau pathology.
Our results showed that the clinical significance of each AD biomarker may be different in the two AD subtypes and that a different approach may be required in each condition. In addition, this difference in pathomechanism also suggests that treatment effects may differ between the two AD subtypes depending on which pathology is targeted. For example, a subgroup analyses of a monoclonal antibody therapy targeting Aβ found the treatment was more effective for LOAD than EOAD39. It is necessary to consider the difference between EOAD and LOAD when targeting and testing the effectiveness of AD therapies. Also, it is important to reduce and control vascular risk in patients with LOAD, and vascular pathology should be considered one of the therapeutic targets in LOAD.
The limitations of our study should be noted. The main limitation is that THK PET is confounded by MAO-B availability across the entire brain, so interpretation needs caution40. THK PET image may reflect neurodegenerative changes caused by reactive astrogliosis as well as tau pathology. Further studies using next generation tau-selective radiotracers will be helpful. Secondly, since we conducted a cross-sectional study, it was not possible to establish temporal relationships. Further study with longitudinal and pathologic data is needed to validate our results. Lastly, this study has the limitation of not analyzing genes other than the APOE4 gene. Previous studies have shown that there is a genetic influence not only in Mendelian EOAD, but also in LOAD and non-Mendelian EOAD41,42,43,44. These genetic influences are believed to have a significant impact on cognitive function and cortical atrophy. Future large-scale studies including genetic analysis are required.
In conclusion, our data suggested the possibility that EOAD and LOAD may have different pathomechanism. The strength of this study lies in its quantitative demonstration of how 10 different variables, including in vivo Alzheimer's pathology, vascular risk factors, and cerebral small vessel disease, affect cognitive function and cortical atrophy in both EOAD and LOAD. Generally, tau pathology had a dominant influence on cognitive functions and cortical atrophy in EOAD, but it is noteworthy that amyloid had a greater impact on memory. In LOAD, not only tau but also several other factors included in the analysis had an influence and it appeared that various other factors not included in the analysis might also be involved in cortical atrophy.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Blennow, K., de Leon, M. J. & Zetterberg, H. Alzheimer’s disease. The Lancet 368, 387–403 (2006).
Zhu, X.-C. et al. Rate of early onset Alzheimer’s disease: a systematic review and meta-analysis. Ann. Transl. Med. 3 (2015).
Migliaccio, R. et al. Mapping the progression of atrophy in early-and late-onset Alzheimer’s disease. J. Alzheimer’s Dis. 46, 351–364 (2015).
Cho, H. et al. Longitudinal changes of cortical thickness in early-versus late-onset Alzheimer’s disease. Neurobiol. Aging 34, e1929–e1921 (2013).
Koss, E. et al. Clinical and neuropsychological differences between patients with earlier and later onset of Alzheimer’s disease: A CERAD analysis, Part XII. Neurology 46, 136–141 (1996).
Smits, L. L. et al. Early onset Alzheimer’s disease is associated with a distinct neuropsychological profile. J. Alzheimer’s Dis. 30, 101–108 (2012).
Schöll, M. et al. Distinct 18F-AV-1451 tau PET retention patterns in early-and late-onset Alzheimer’s disease. Brain 140, 2286–2294 (2017).
Cho, H. et al. Amyloid deposition in early onset versus late onset Alzheimer’s disease. J. Alzheimer’s Dis. 35, 813–821 (2013).
Marshall, G. A., Fairbanks, L. A., Tekin, S., Vinters, H. V. & Cummings, J. L. Early-onset Alzheimer’s disease is associated with greater pathologic burden. J. Geriatr. Psychiatry Neurol. 20, 29–33 (2007).
Lee, W. J. et al. Effects of alzheimer’s and vascular pathologies on structural connectivity in early-and late-onset Alzheimer’s disease. Front. Neurosci. 15, 606600 (2021).
Iturria-Medina, Y., Sotero, R. C., Toussaint, P. J., Mateos-Pérez, J. M. & Evans, A. C. Early role of vascular dysregulation on late-onset Alzheimer’s disease based on multifactorial data-driven analysis. Nat. Commun. 7, 11934 (2016).
Luchsinger, J. et al. Aggregation of vascular risk factors and risk of incident Alzheimer disease. Neurology 65, 545–551 (2005).
Helzner, E. P. et al. Contribution of vascular risk factors to the progression in Alzheimer disease. Arch. Neurol. 66, 343–348 (2009).
Deschaintre, Y., Richard, F., Leys, D. & Pasquier, F. Treatment of vascular risk factors is associated with slower decline in Alzheimer disease. Neurology 73, 674–680 (2009).
McKhann, G. et al. Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA Work Group* under the auspices of Department of Health and Human Services Task Force on Alzheimer’s disease. Neurology 34, 939–939 (1984).
Seo, S. W., Cho, S. S., Park, A., Chin, J. & Na, D. L. Subcortical vascular versus amnestic mild cognitive impairment: Comparison of cerebral glucose metabolism. J. Neuroimaging 19, 213–219 (2009).
Fazekas, F., Chawluk, J. B., Alavi, A., Hurtig, H. I. & Zimmerman, R. A. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. Am. J. Neuroradiol. 8, 421–426 (1987).
Chung, J. et al. Normalization of cortical thickness measurements across different T1 magnetic resonance imaging protocols by novel W-Score standardization. Neuroimage 159, 224–235 (2017).
Greve, D. N. et al. Different partial volume correction methods lead to different conclusions: An 18 F-FDG-PET study of aging. Neuroimage 132, 334–343 (2016).
Greve, D. N. et al. Cortical surface-based analysis reduces bias and variance in kinetic modeling of brain PET data. Neuroimage 92, 225–236 (2014).
Okamura, N. et al. Non-invasive assessment of Alzheimer’s disease neurofibrillary pathology using 18F-THK5105 PET. Brain 137, 1762–1771 (2014).
Lockhart, S. N. et al. Dynamic PET measures of tau accumulation in cognitively normal older adults and Alzheimer’s disease patients measured using [18F] THK-5351. PLoS ONE 11, e0158460 (2016).
Thurfjell, L. et al. Automated quantification of 18F-flutemetamol PET activity for categorizing scans as negative or positive for brain amyloid: Concordance with visual image reads. J. Nucl. Med. 55, 1623–1628 (2014).
Grömping, U. Relative importance for linear regression in R: The package relaimpo. J. Stat. Softw. 17, 1–27 (2007).
Bejanin, A. et al. Tau pathology and neurodegeneration contribute to cognitive impairment in Alzheimer’s disease. Brain 140, 3286–3300 (2017).
Bloom, G. S. Amyloid-β and tau: The trigger and bullet in Alzheimer disease pathogenesis. JAMA Neurol. 71, 505–508 (2014).
Jack, C. R. et al. A/T/N: An unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology 87, 539–547 (2016).
Cavedo, E. et al. Medial temporal atrophy in early and late-onset Alzheimer’s disease. Neurobiol. Aging 35, 2004–2012 (2014).
Rabin, J. S. et al. Vascular risk and β-amyloid are synergistically associated with cortical tau. Ann. Neurol. 85, 272–279 (2019).
Korczyn, A. D. Mixed dementia—the most common cause of dementia. Ann. N. Y. Acad. Sci. 977, 129–134 (2002).
Schneider, J. A., Arvanitakis, Z., Bang, W. & Bennett, D. A. Mixed brain pathologies account for most dementia cases in community-dwelling older persons. Neurology 69, 2197–2204 (2007).
Schneider, J. A., Boyle, P. A., Arvanitakis, Z., Bienias, J. L. & Bennett, D. A. Subcortical infarcts, Alzheimer’s disease pathology, and memory function in older persons. Ann. Neurol. 62, 59–66 (2007).
Honjo, K., Black, S. E. & Verhoeff, N. P. Alzheimer’s disease, cerebrovascular disease, and the β-amyloid cascade. Can. J. Neurol. Sci. 39, 712–728 (2012).
Apátiga-Pérez, R. et al. Neurovascular dysfunction and vascular amyloid accumulation as early events in Alzheimer’s disease. Metab. Brain Dis. 37, 39–50 (2022).
Zhang-Nunes, S. X. et al. The cerebral β-amyloid angiopathies: Hereditary and sporadic. Brain Pathol. 16, 30–39 (2006).
Ramser, E. M. et al. Amyloid-β oligomers induce tau-independent disruption of BDNF axonal transport via calcineurin activation in cultured hippocampal neurons. Mol. Biol. Cell 24, 2494–2505 (2013).
Seo, S. W. et al. Cortical thinning related to periventricular and deep white matter hyperintensities. Neurobiol. Aging 33, 1156–1167 (2012).
van der Flier, W. M. et al. Small vessel disease and general cognitive function in nondisabled elderly: The LADIS study. Stroke 36, 2116–2120 (2005).
Van Dyck, C. H. et al. Lecanemab in early Alzheimer’s disease. N. Engl. J. Med. 388, 9–21 (2023).
Ng, K. P. et al. Monoamine oxidase B inhibitor, selegiline, reduces 18F-THK5351 uptake in the human brain. Alzheimer’s Res. Ther. 9, 1–9 (2017).
Andrade-Guerrero, J. et al. Alzheimer’s disease: An updated overview of its genetics. Int. J. Mol. Sci. 24, 3754 (2023).
Andrews, S. J. et al. The complex genetic architecture of Alzheimer’s disease: novel insights and future directions. EBioMed. 90 (2023).
Chen, H.-H. et al. Genetically regulated expression in late-onset Alzheimer’s disease implicates risk genes within known and novel loci. Transl. Psychiatry 11, 618 (2021).
Reitz, C., Rogaeva, E. & Beecham, G. W. Late-onset vs nonmendelian early-onset Alzheimer disease: A distinction without a difference?. Neurol. Genet. 6, e512 (2020).
Acknowledgements
This study was supported by a grant of the Korea Healthcare Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant No: HI14C1135), a grant from the Basic Science Research Program through the National Research Foundation of Korea (NRF) that is funded by the Ministry of Education (Grant No: 2021R1A6A1A03038996), and Gachon University Gil Medical Center (Grant number : FRD2022-16).
Funding
This study was supported by a grant of the Korea Healthcare Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant No: HI14C1135), a Grant from the Basic Science Research Program through the National Research Foundation of Korea (NRF) that is funded by the Ministry of Education (Grant No: 2021R1A6A1A03038996), and Gachon University Gil Medical Center (Grant number : FRD2022-16).
Author information
Authors and Affiliations
Contributions
Design of the study: J.C., Y.N. Supervision: Y.N., J.-K.S., S.N.L., C.K. Acquisition of funding: Y.N. Data acquisition: H.S., W.-R.K., Y.N. Data processing and statistical analyses: J.C., J.-H.S., H.S., W.-R.K., H.K.N., J.B. First draft of the manuscript: C.W.Y., J.C. Revision and final version of manuscript: All authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Written informed consent was obtained from all participants and the study was approved by Institutional Review Board of Gachon University Gil Medical Center (IRB No: GDIRB2015-272).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cho, J., Yoon, C.W., Shin, JH. et al. Heterogeneity of factors associated with cognitive decline and cortical atrophy in early- versus late-onset Alzheimer’s disease. Sci Rep 14, 20429 (2024). https://doi.org/10.1038/s41598-024-71402-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71402-6
- Springer Nature Limited