Abstract
Peripheral nerve injury (PNI) often leads to retrograde cell death in the spinal cord and dorsal root ganglia (DRG), hindering nerve regeneration and functional recovery. Repetitive magnetic stimulation (rMS) promotes nerve regeneration following PNI. Therefore, this study aimed to investigate the effects of rMS on post-injury neuronal death and nerve regeneration. Seventy-two rats underwent autologous sciatic nerve grafting and were divided into two groups: the rMS group, which received rMS and the control (CON) group, which received no treatment. Motor neuron, DRG neuron, and caspase-3 positive DRG neuron counts, as well as DRG mRNA expression analyses, were conducted at 1-, 4-, and 8-weeks post-injury. Functional and axon regeneration analyses were performed at 8-weeks post-injury. The CON group demonstrated a decreased DRG neuron count starting from 1 week post-injury, whereas the rMS group exhibited significantly higher DRG neuron counts at 1- and 4-weeks post-injury. At 8-weeks post-injury, the rMS group demonstrated a significantly greater myelinated nerve fiber density in autografted nerves. Furthermore, functional analysis showed significant improvements in latency and toe angle in the rMS group. Overall, these results suggest that rMS can prevent DRG neuron death and enhance nerve regeneration and motor function recovery after PNI.
Similar content being viewed by others
Introduction
Peripheral nerve injury (PNI) can lead to impairments in both motor and sensory functions, significantly affecting patients’ quality of life1. Furthermore, severe PNI is often associated with retrograde cell death in the spinal cord and dorsal root ganglion (DRG)2,3. A reduction in the number of neurons following injury hinders nerve regeneration, subsequently triggering functional deficits4. Although nerve autografts are considered the gold standard surgical treatment for PNI, neuronal cell death remains a significant challenge for subsequent nerve regeneration and functional recovery1,4,5. This phenomenon delays the rehabilitation process of patients with PNI, significantly affecting their return to normal work and daily life. Therefore, suppressing post-injury cell death could potentially promotes functional recovery, thereby helping patients with PNI improve their quality of life and achieve better rehabilitation outcomes.
Magnetic stimulation is a promising physical therapeutic approach for promoting nerve regeneration and functional recovery following nerve injury6,7. Its therapeutic effect may be attributed to the electromagnetic field's influence on cell membranes and action potentials, which increases Ca2+ influx and activates signaling pathways such as cyclic adenosine monophosphate-protein kinase A (cAMP-PKA) and dual leucine zipper kinase (DLK), which are known to promote nerve regeneration following PNI8,9. Repetitive magnetic stimulation (rMS) is noninvasive, influences the microenvironment for nerve regeneration, and induces neuroplastic changes10. In animal experiments, its application to peripheral nerves promoted axonal regeneration11. While previous studies have suggested that rMS in the spinal cord can enhance synaptic regeneration following PNI12, its effect on neuronal cell bodies within the spinal cord and DRG remains unclear. Here, we hypothesize that rMS can prevent neuronal death following PNI and promote nerve regeneration and functional recovery.
The selection of an appropriate PNI model is important to investigate the effects of rMS on neuronal death. Our earlier study using a sciatic nerve crush injury rat model did not observe a reduction in the number of DRG neurons13. Therefore, in the present study, we used a more rigorous PNI animal model, specifically a sciatic nerve autograft model, though which we observed a reduction in the number of spinal cord anterior horns and DRG neurons.
The present study aimed to advance this field by applying non-invasive rMS directly to neurons to investigate its effects on post-injury neuronal cell death and nerve regeneration.
Results
No difference in motor neuron count was found at any time point
Beginning the day after the sciatic nerve autograft, the rats in the rMS groups were treated with rMS until euthanasia (Fig. 1). Representative images of the motor neurons (MNs) are shown in Fig. 2a, b. Quantitative analysis revealed a significant decrease in the total MN and α-MN (choline acetyltransferase [ChAT]+, neuronal nuclei [NeuN]+) counts in both the rMS and control (CON) groups starting from 1 week post-injury (total MNs: all rMS groups, 4-week CON group, and 8-week CON group, p < 0.0001; 1-week CON group, p = 0.0012) (α-MNs: all rMS groups, 4-week CON group, and 8-week CON group, p < 0.0001; 1-week CON group, p = 0.0035); however, no decrease was observed in γ-MNs (ChAT+, NeuN-) (Fig. 2c). Additionally, the mean number of total MNs, α-MNs, and γ-MNs showed no significant difference between the rMS and CON groups at any time point (Fig. 2c).
Spinal cord anterior horn motor neurons. (a) Representative images of spinal cord anterior horn motor neurons (MNs) stained with choline acetyltransferase (ChAT) and neuronal nuclei (NeuN) antibodies (red, ChAT; green, NeuN; α-MNs, ChAT+ and NeuN+; γ-MNs, ChAT+ and NeuN-). Scale bar: 20 μm. (b) Representative images of spinal cord anterior horn MNs in the rMS, CON, and intact groups. Scale bar: 50 μm. (c) Mean number of total MNs, α-MNs, and γ-MNs at 1, 4, and 8 weeks post-injury. All data are shown as means ± standard deviations (##p ˂ 0.01 vs. intact group; n.s.: not significant; n = 6).
rMS prevented the decrease in DRG neurons post-injury
A representative image of DRG neurons is shown in Fig. 3a. Quantitative analysis showed that the DRG neuron counts in the CON group significantly decreased from 1 week post-injury (CON groups: 1-week, p = 0.0175; 4-week, p = 0.0071; 8-week, p = 0.0060) (Fig. 3b). DRG neuron counts in the rMS groups were significantly higher than those in the CON group at the 1- and 4-week time points (1-week, p = 0.0241; 4-week, p = 0.0071) (Fig. 3b).
Dorsal root ganglion neurons. (a) Representative images of dorsal root ganglion (DRG) neurons with hematoxylin and eosin (HE) staining. Scale bar: 10 μm. (b) Mean number of DRG neurons at 1, 4, and 8 weeks post-injury. All data are shown as means ± standard deviations (*p ˂ 0.05, **p ˂ 0.01 vs. CON group; #p ˂ 0.05, ##p ˂ 0.01 vs. intact group; n = 6).
No differences in apoptotic DRG neuron counts were found at any time point
Previous studies have shown that caspase-3 is a reliable marker of apoptosis14. Here, we used antibodies against caspase-3 to label apoptotic DRG neurons. Representative images of apoptotic DRG neurons are shown in Fig. 4a. Apoptotic DRG neuron counts revealed no significant difference between the rMS and CON groups at any time point (Fig. 4b).
rMS modulates the mRNA expression of neuroregeneration-, inflammation-, and apoptosis-related genes post-injury in the DRG
Compared with that of the intact group, the mRNA expression of nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF), growth-associated protein 43 (GAP-43), and interleukin 6 (IL-6) in the DRG of rats in the rMS and CON groups, as well as that of Bcl2-associated X protein (Bax) in the CON group only, were significantly upregulated 1-week post-injury (1-week rMS group: NGF, p = 0.0388; BDNF, p < 0.0001; GAP-43, p < 0.0001; IL-6, p < 0.0001) (1-week CON group: NGF, p = 0.0092; BDNF, p < 0.0001; GAP-43, p < 0.0001; IL-6, p < 0.0001; Bax, p = 0.0002) (Fig. 5a, b, d, e, g). Additionally, at 4-weeks post-injury, NGF, GAP-43, IL-6, Bax, and B-cell CLL/lymphoma 2 (Bcl-2) were significantly upregulated in the rMS group, whereas BDNF, GAP-43, and IL-6 were significantly upregulated in the CON group (4-week rMS group: NGF, p < 0.0001; GAP-43, p < 0.0001; IL-6, p < 0.0001; Bax, p < 0.0001; Bcl-2, p < 0.0001) (4-week CON group: BDNF, p < 0.0001; GAP-43, p < 0.0001; IL-6, p < 0.0001) (Fig. 5a, b, d, e, g, h). Furthermore, at 8-weeks post-injury, BDNF expression was significantly increased in the rMS group, whereas GAP-43 and Bcl-2 expression was significantly elevated in the CON group (8-week rMS group: BDNF, p < 0.0001) (8-week CON group: GAP-43, p < 0.0001; Bcl-2, p = 0.0280) (Fig. 5b, d, h). Research has shown that the ratio of Bax to Bcl-2 expression determines the apoptotic potential of an individual cell15. In the present study, the mRNA expression of Bax/Bcl-2 was utilized to investigate apoptosis in DRG neurons. Our results found that the Bax/Bcl-2 ratio was significantly decreased in the CON group at 4- and 8-weeks post-injury (CON groups: 4-week, p = 0.0206; 8-week, p = 0.0100) (Fig. 5i).
Results of reverse transcription-quantitative polymerase chain reaction. Gene expression of (a) NGF, (b) BDNF, (c) NT-3, (d) GAP-43, (e) IL-6, (f) TNF, (g) Bax, (h) Bcl-2, and (i) the ratio of Bax/Bcl-2 in the rMS, CON, and intact groups at 1, 4, and 8 weeks post-injury. All data are shown as means ± standard deviations. The mean value of the calibration samples (intact group, n = 6) was set to 1 (*p < 0.05, **p < 0.01, vs. CON group; #p < 0.05, ##p < 0.01, vs. intact group; n = 6).
Compared with that of the CON group, neurotrophin-3 (NT-3), GAP-43, IL-6, tumor necrosis factor (TNF), and Bax mRNA expression in the DRG of the rMS groups was significantly downregulated at 1-week post-injury (1-week: NT-3, p = 0.0460; GAP-43, p < 0.0001; IL-6, p = 0.0136; TNF, p = 0.0397; Bax, p = 0.0075) (Fig. 5c–g). Moreover, 4-weeks post-injury, NGF, NT-3, GAP-43, IL-6, Bax, and Bcl-2 were significantly upregulated in the rMS group (4-week: NGF, p = 0.0030; NT-3, p = 0.0039; GAP-43, p < 0.0001; IL-6, p = 0.0038; Bax, p < 0.0001; Bcl-2, p = 0.0004), whereas BDNF was significantly upregulated in the CON group (4-week: BDNF, p = 0.0011) (Fig. 5a–e, g, h). Additionally, at 8-weeks post-injury, BDNF expression was significantly increased in the rMS group (8-week: BDNF, p = 0.0001), whereas GAP-43 expression was significantly elevated in the CON group (8-week: GAP-43, p = 0.0073) (Fig. 5b, d). The Bax/Bcl-2 ratio significantly decreased in the rMS group at 1-week post-injury (1-week: p = 0.0288) and in the CON group at 4-weeks post-injury (4-week: p = 0.0296) (Fig. 5g).
rMS promotes electrophysiological improvements at 8-weeks post-injury
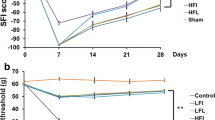
Wet muscle weight and compound muscle action potentials (CMAPs) of the gastrocnemius muscle were assessed to confirm reinnervation. Both wet muscle weight and CMAP amplitudes of the gastrocnemius muscle showed no differences between the rMS and CON groups at 8-weeks post-injury (Fig. 6a, b). However, the CMAP latency in the rMS group was significantly improved at 8-weeks post-injury (p = 0.0440) (Fig. 6b).
Wet muscle weight, electrophysiological analysis of gastrocnemius muscle, and kinematic analysis. (a) The wet muscle weight of the gastrocnemius muscle, expressed as the ratio of the injured side to the non-injured side at 8 weeks post-injury is presented. All data are shown as means ± standard deviations (n = 6). (b) The amplitudes and latencies of compound muscle action potentials of the gastrocnemius muscle expressed as the ratio of the injured side to the non-injured side at 8 weeks post-injury. All data are shown as means ± standard deviations (*p ˂ 0.05 vs. CON group; n = 6). (c). A representative image of the ankle angle (angle delineated by the two red lines) and toe angle (angle delineated by the yellow line and dashed line) in the toe-off phase. (d) The joint angle in the toe-off phase at 8 weeks post-injury. All data are shown as means ± standard deviations (*p ˂ 0.05 vs. CON group; ##p ˂ 0.01 vs. intact group; n = 6).
rMS promotes motor function recovery
A representative image of the ankle and toe angles during the toe-off phase is shown in Fig. 6c. The ankle angle is indicated by two red lines, whereas the toe angle is indicated by the yellow dashed lines (Fig. 6c). At 8-weeks post-injury, kinematic analysis revealed that both the ankle and toe angles in the toe-off phase were significantly decreased in both the rMS and CON groups, compared with those in the intact group (ankle angles: rMS group, p < 0.0001; CON group, p < 0.0001) (toe angles: rMS group, p < 0.0001; CON group, p < 0.0001) (Fig. 6d). However, the toe angle was significantly greater in the rMS group than that in the CON group (p = 0.0352) (Fig. 6d). No significant difference was observed in the ankle angles between the rMS and CON groups (Fig. 6d).
rMS promotes sciatic nerve regeneration
Representative images of the transected sciatic nerve sections observed under transmission electron microscopy are shown in Fig. 7a. Quantitative analysis revealed that the myelinated nerve diameter, axon diameter, and myelin sheath thickness did not differ significantly between the rMS and CON groups at 8-weeks post-injury (Fig. 7b).
Axon regeneration evaluation. (a) Representative transmission electron micrographs of transected sciatic nerves in the rMS and CON groups at 8 weeks post-injury. Scale bar: 2 μm. (b) Mean myelinated nerve diameter, mean axon diameter, and mean myelin sheath thickness of autografted sciatic nerves. All data are shown as means ± standard deviations (n = 6). (c) Representative images of the autografted sciatic nerve with toluidine blue staining. Scale bar: 100 μm. (d) Mean myelinated fiber density at 8 weeks post-injury. All data are shown as means ± standard deviations (*p ˂ 0.05 vs. CON group; n = 6).
Representative images of nerve fibers processed with toluidine blue staining are displayed in Fig. 7c. Quantitative analysis indicated that myelinated nerve fiber density was significantly higher in the rMS group than that in the CON group at 8-weeks post-injury (p = 0.0233) (Fig. 7d).
Discussion
rMS is a promising noninvasive method for treating PNI. However, its optimal use and the mechanisms of regeneration remain unclear. To date, most treatments used to promote nerve regeneration following PNI have focused on the regeneration outcomes of injured nerves, while few studies have focused on the effects on upstream neurons. In the present study, we investigated the effects of rMS on neurons and assessed the promotion of nerve regeneration after PNI.
First, we investigated changes in the spinal cord anterior horn MNs and DRG neurons at different time points following PNI. Similar to the findings of previous studies2,3, we confirmed that the sciatic nerve autograft model, an established model of PNI, reduced the numbers of MNs and DRG neurons (Figs. 2 and 3). Previous studies have suggested that electrical stimulation may prevent neuronal death following PNI16,17. However, as an invasive treatment, electrical stimulation poses risks such as the need for invasive procedures and the potential for infection, making it challenging for clinical use. In contrast, noninvasive rMS does not present such issues. As confirmed through histological analysis, rMS prevented a decrease in the number of DRG neurons. However, similar effects were not observed in the MNs. We speculate that this discrepancy may be attributed to the application of rMS from the dorsal side, which may not affectively reach the anterior horn neurons. Although we verified the spinal stimulation intensity capable of eliciting electromyographic (EMG) responses in the gastrocnemius muscle before conducting the experiments, whether this response was caused by magnetic-field-induced motor potentials that were transmitted from the spinal anterior roots to the muscle was not ascertained. Due to the transverse placement of the stimulation coil over the lumbar spinal cord area, the observed EMG response may be attributed to the stimulation of the adjacent sciatic nerve by rMS. Therefore, to prevent a reduction in MNs after PNI, the intervention parameters of rMS should be reconsidered to effectively reach the spinal cord anterior horn.
To validate the effect of rMS on apoptosis in DRG neurons, the expression of the apoptosis marker, caspase-3, was examined in DRG neurons at 1-, 4- and 8-week time points. However, no significant effect of rMS on DRG neuronal apoptosis, compared with that of the CON group, was observed at each time point (Fig. 4). Considering the number of DRG neurons (Fig. 3), this outcome might be attributed to the apoptosis of most neurons having already occurred at the earliest observed time point. Moreover, a previous study showed that the percentage of DRG neuronal loss was the highest within 1 week of PNI18. Therefore, future investigations should observe time points before 1-week post-injury to confirm the effect of rMS on apoptosis.
Neurotrophic factors play an important role in promoting nerve regeneration19,20. Our previous studies showed that mRNA expression levels of NGF and BDNF in the DRG are upregulated in response to sciatic nerve injury13. In the present study, we observed a more sustained upregulation of NGF and BDNF in the rMS group compared to that observed in the CON group (Fig. 5) after 4- and 8-weeks, respectively. Given the association of neurotrophic factors with axonal growth and remyelination21,22, we believe that rMS promotes sustained upregulation of NGF and BDNF, thereby promoting nerve regeneration.
GAP-43 is a membrane protein associated with axonal growth that is commonly used as a marker of neuronal regeneration23,24. Consistent with previous studies, our study found that the mRNA expression of GAP-43 was significantly increased in both the CON and rMS groups after PNI13,25. In the CON group, GAP-43 expression was significantly higher than that in the rMS group at 1-week post-injury and gradually decreased at subsequent time points; however, it remained at a significantly higher level than normal at 8-weeks. In contrast, GAP-43 expression in the rMS group showed a more moderate increasing trend. It reached its peak at 4-weeks post-injury, with levels significantly higher than those in the CON group, followed by a return to baseline levels at 8-weeks post-injury, with levels significantly lower than those in the CON group. However, the observation fact that GAP-43 levels returned to the baseline more rapidly in the rMS group was not sufficient evidence to conclude complete nerve repair. Complete nerve repair typically involves multiple factors, including myelin sheath integrity and functional recovery. Therefore, we conducted comprehensive evaluations of axon regeneration, electrophysiological measurements, and functional assessments to determine the state of nerve repair. The results of our 8-week evaluation of myelinated fiber density in axon regeneration, along with the toe angle from three-dimensional (3D) motion analysis and the latency of gastrocnemius CMAP, further support the conclusion that rMS promotes nerve regeneration.
Following PNI, inflammatory cytokines rapidly respond to nerve damage by recruiting macrophages and regulating the expression of regeneration-associated genes, thus exerting both neuroprotective and axonal regeneration-promoting effects26,27. However, evidence suggests that an excessive inflammatory response may hinder early stage recovery after PNI28. In this study, we examined the mRNA expression of IL-6 and TNF. Consistent with our previous findings, IL-6 expression increased rapidly after injury, whereas TNF expression showed no significant change13. At the 1-week time point post-injury, IL-6 expression was significantly higher in the CON group than that in the rMS group. However, at the 4-week time point, IL-6 expression in the CON group decreased rapidly and was significantly lower than that in the rMS group, with both groups returning to normal levels after 8 weeks. Although TNF expression showed no significant change at each time point in the rMS group, compared with that in the intact group, TNF expression in the rMS group was significantly lower than that in the CON group at 1-week post-injury. These results suggest that following PNI, rMS may prevent DRG neuronal loss by reducing the expression of inflammatory cytokines. This reduction could decrease excessive inflammation and subsequently slow the decline in IL-6 expression compared with that in the CON group, thereby continuously promoting nerve regeneration.
Bax and Bcl-2 both belong to the Bcl-2 protein family and play important roles in the process of cell apoptosis29,30. Bax is a pro-apoptotic protein that promotes mitochondrial permeabilization, leading to the release of apoptotic inducers such as cytochrome C from the mitochondria into the cytoplasm and ultimately triggering cell apoptosis29,31. In contrast, Bcl-2 acts as an anti-apoptotic protein primarily by maintaining the integrity and stability of the mitochondrial membrane to counteract the effects of Bax and prevent apoptosis29,31. Therefore, the balance between Bax and Bcl-2 expression is a critical determinant of cell survival and apoptosis. An increase in the activity of Bax or a decrease in the activity of Bcl-2 leads to an increase in the propensity for apoptosis, and vice versa15. We found that at 1-week post-injury, the expression of Bax in the CON group was significantly increased, reaching levels higher than those in the rMS group, whereas no significant increase was observed in the rMS group. Additionally, the Bax/Bcl-2 ratio in the rMS group was significantly lower than that in the CON group at the 1-week time point. We speculated that rMS may prevent an increase in early Bax expression post-injury, thereby preventing a DRG neuronal loss. Furthermore, 4-weeks post-injury, the expression of both Bax and Bcl-2 increased in the rMS group, maintaining a stable Bax/Bcl-2 ratio. However, in the CON group, Bcl-2 expression was significantly upregulated at 8-weeks, with a significant downregulation of the Bax/Bcl-2 ratio at 4- and 8-weeks. Further research is required to elucidate the relationship between these results and neuronal death.
Our previous studies have reported that the toe angles in the toe-off phase gradually recover with nerve regeneration32. In this study, we found a significant improvement in the toe angle in the rMS group at 8-weeks post-injury (Fig. 6d). Additionally, the latency of the gastrocnemius innervated by the sciatic nerve showed significant improvement (Fig. 6b). CMAP latency represents a delay in nerve impulse conduction (the time interval between stimulation and response)33, indicating that rMS promotes the speed of nerve response and recovery of motor function in PNI rats. Furthermore, in the axonal regeneration evaluation, we observed that the myelinated fiber density in the rMS group was significantly higher than that in the CON group (Fig. 7). Collectively, these results suggested that rMS targeting the spinal cord promots nerve regeneration following PNI.
This study had a few limitations. First, we observed no protective effect of rMS on the spinal cord anterior horn MNs, in contrast to its protective effect on DRG neurons. This discrepancy may be attributed to the rMS parameters used, which may not effectively transmit stimulation to the anterior horn of the spinal cord. Thus, the effect on MNs after PNI must be explored by appropriately adjusting parameters, such as intensity. Second, though this study demonstrated the beneficial effects of rMS, the underlying mechanisms, particularly at the molecular level, remain unclear. Future research should explore the molecular pathways involved in rMS-induced neuroprotection and nerve regeneration, such as the modulation of inflammatory cytokines, to gain a more comprehensive understanding of the mechanisms by which rMS exerts its effects. Moreover, the counts of DRG neurons and caspase-3-positive cells support the notion that the significant reduction in DRG neurons in the CON group primarily occurred within the first week after injury, consistent with previous research findings18. Future studies should focus on the early stages, within the first week post-injury, to further investigate the mechanism by which rMS prevents a reduction in DRG neurons. Additionally, while we observed that rMS improved the toe angle after PNI using 3D motion analysis, which partially reflects the recovery of motor function, further analysis is required to validate the effectiveness of rMS in promoting motor function recovery. To gain a more comprehensive understanding of the long-term benefits of rMS, the observation period should be further extended in future studies. Finally, DRG neurons are sensory neurons. Since sensory function and motor performance are closely interrelated, whether the observed improvement in motor function in this study is attributable to the recovery of sensory input remains unclear. Studies have shown that magnetic field therapy can help improve hyperalgesia after PNI34,35; thus, the alleviation of pain may contribute to the mechanism underlying this relationship. Since we did not assess sensory functions in this study, further research is required to investigate the effects of rMS on sensory-related molecules and functions.
In conclusion, this study confirmed that rMS prevents DRG neuronal death after PNI. Additionally, we demonstrated that rMS promotes nerve regeneration and motor function recovery following PNI at 8-weeks post-injury. These outcomes may be attributed to the modulation of mRNA expression of neurotrophic factors, growth-associated proteins, inflammatory cytokines, and apoptotic factors. These findings provide a foundation that may further contribute to the development of treatments aimed at preventing neuronal cell death following severe PNI and the associated impediments to nerve regeneration and functional recovery. Additional research is needed to elucidate the specific mechanisms by which rMS prevents neuronal death at an early stage and to determine optimal stimulation parameters.
Materials and methods
Animals
The experimental setup is illustrated in Fig. 1a. In total, 84 12-week-old male Lewis rats weighing between 250 and 300 g (Shimizu Laboratory Supplies Co., Ltd., Kyoto, Japan) were purchased and used for this experiment. The rats were housed in groups of three per cage, provided with ample food and water, and subjected to a 12-h light–dark cycle to mimic natural day and night conditions. Among the 84 rats, 72 were randomly divided into the rMS and CON groups (36 rats per group) using a computer-based random-order generator. Samples from both the rMS and CON groups (18 rats per group) underwent reverse transcription-quantitative polymerase chain reaction (RT-qPCR) at 1, 4, and 8 weeks postoperatively (n = 6 for each group at each time point).
Tissue samples from 36 rats in the rMS and CON groups (n = 18 per group) were subjected to immunohistochemistry and hematoxylin and eosin (HE) staining at various postoperative time points (1, 4, and 8 weeks) (n = 6 for each group at each time point). At the 8-week time point, 6 rats from each group underwent electrophysiological and motor function assessments prior to euthanasia. Euthanasia was performed by overdosing the rats with 2% isoflurane inhalation anesthesia, followed by exsanguination through a cardiac incision. Wet muscle weight measurements and axon regeneration evaluations were also performed at the 8-week time point. Furthermore, 6 rats were designated as intact calibration samples for RT-qPCR, and an additional 6 rats were used as intact samples for immunohistochemistry and HE staining analyses. The sample size in this study was determined based on previous studies13,36,37. Histological evaluations were performed by author ZZ, who was blinded to the treatment. This study was approved by the Animal Experiment Committee of Kyoto University (approval no. MedKyo23073), and all procedures were performed in accordance with the Regulations on Animal Experimentation at Kyoto University and the ARRIVE guidelines.
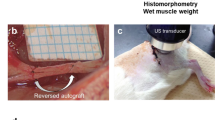
Surgery
A rat model of sciatic nerve autograft injury was used in this study37. Rats were anesthetized through intraperitoneal injection of a mixed anesthetic (0.15 mg/kg medetomidine, 2 mg/kg midazolam, and 2.5 mg/kg butorphanol)37. The left sciatic nerve was exposed through a longitudinal lateral incision along the thigh. An 8-mm-long sciatic nerve was excised at the mid-thigh, 85–90 mm from the tip of the third toe, and grafted using 9-0 nylon sutures (T06A09N20-25, Bear Medic Corporation, Tokyo, Japan). The muscles and skin were closed using 4-0 nylon sutures (S15G04N-45; Bear Medic Corporation, Tokyo, Japan). Additionally, the presence of autografted nerves was confirmed upon euthanizing the rats, ensuring the exclusion of animals with unsuccessful autografting during the data collection process.
rMS protocol
The rMS protocol’s settings are depicted in Fig. 1b. rMS was delivered using a coil connected to a commercially available magnetic stimulator (Pathleader, IFG Corporation, Sendai, Japan). The stimulation area of the rMS coil was 45 mm long and 25 mm wide. The coil was placed transversely over the lumbar spinal cord of the animal for intervention. During stimulation, the rats were anesthetized with 2% isoflurane inhalation and secured in the prone position on the table to prevent struggling during the procedure. To determine the appropriate stimulation intensity to ensure that rMS could be delivered to the spinal cord, we performed EMG of the gastrocnemius muscles in intact rats. Stable EMG responses of the gastrocnemius muscle were observed at an intensity of 50% of the maximum output. Previous studies have shown that a stimulation frequency of 20 Hz has a promoting effect on nerve regeneration11. Therefore, the stimulation parameters used in this study were set at a frequency of 20 Hz, a stimulation intensity of 50%, a 2-s train duration, and an inter-train interval of 13 s, with 40 trains per session. Each session of rMS comprised 1,600 pulses/day delivered within 10 min, five times per week, from the first postoperative day until sacrifice. The CON group did not undergo rMS.
Immunohistochemistry
After the rats were euthanized, the L4–L6 spinal cord and ipsilateral L4 and L5 DRGs were dissected. The dissected tissues were fixed with 4% paraformaldehyde for 24 h, followed by incubation in 30% sucrose for 48 h at 4 °C. All tissues were embedded in the optimal cutting temperature compound, and stored at − 80 °C after freezing in liquid nitrogen. Subsequently, 10-μm-thick cryostat cross-sections of the spinal cord and longitudinal sections of the DRGs were prepared.
Three random sections of each spinal cord specimen were stained. Spinal cord slides were washed with phosphate-buffered saline (PBS) and treated with a blocking buffer containing 5% bovine serum albumin (Roche Holding AG) at room temperature (approximately 25 °C) for 30 min. Primary antibodies, including goat anti-ChAT (1:100; AB144P, Merck Millipore, Burlington, MA, USA) and mouse anti-NeuN (1:100; MAB377, Merck Millipore, Burlington, MA, USA), were added, and the slides were incubated overnight at 4 °C. Following PBS washes, the slides were incubated with Alexa Fluor 594 donkey anti‐goat IgG (1:200; A-11058, Life Technologies, Carlsbad, CA, USA) and Alexa Fluor 488 donkey anti-mouse IgG (1:200; A-21202, Life Technologies, Carlsbad, CA, USA) secondary antibodies at room temperature for 2 h. After washing with PBS, the coverslips were mounted on all slides using an aqueous mounting medium. In accordance with previous research, anterior horn α-MNs were identified as those exhibiting ChAT and NeuN immunoreactivity in a region > 300 μm2, while γ-MNs were defined as those exhibiting only ChAT immunoreactivity38,39,40. This protocol was used to label and quantify the two types of MNs. Three random cross sections of each sample were examined using a confocal laser scanning microscope (FV10i; Olympus, Tokyo, Japan). The number of ipsilateral anterior horn MNs in each image was manually counted using the ImageJ software (National Institutes of Health, Bethesda, MD, USA). The number of MNs per rat was calculated as the mean of the three images.
DRG sections were treated with a 3% hydrogen peroxide solution for 30 min. For antigen retrieval, sections were heated at 65 °C for 30 min in HistoVT One (Nacalai Tesque, Inc., Kyoto, Japan; diluted 1:10) and washed thrice with PBS. Normal goat serum (5%) was used as a blocking solution for 30 min at room temperature. Subsequently, the sections were incubated overnight at 4 °C with a rabbit polyclonal anti-cleaved-caspase-3 primary antibody (1:100; Asp175, Cell Signaling Technology, Danvers, MA, USA). All sections were subsequently rinsed and treated with goat anti-rabbit IgG for 30 min at room temperature. Antigen–antibody complexes were detected using an avidin–biotin complex reagent (ABC kit PK-6100; Vector Laboratories, Burlingame, CA, USA) enhanced with 3,3′-diaminobenzidine (DAB kit SK-4105; Vector Laboratories, Burlingame, CA, USA). The sections were then viewed under a light microscope (Eclipse 80i; Nikon, Tokyo, Japan), and positive cells were counted. The number of positive cells per rat was calculated as the average count of one image of the L4 and L5 DRG from each rat, with values representing the number of cells per 0.1 mm2.
HE staining
Three random sections of each L4 and L5 DRG specimen were selected for HE staining. Sections were examined under a light microscope (DM2500; Leica, Wetzlar, Germany). The number of DRG neurons in each image was manually counted using ImageJ software. The number of DRG neurons per rat was calculated as the sum of the mean numbers of L4 and L5 DRG neurons and represented as the number of neurons per 0.1 mm2.
RT-qPCR
The L4 and L5 DRG of each rat were dissected at 1, 4, and 8 weeks postoperatively; 6 intact rats were dissected as intact controls. Total RNA was extracted from the DRG specimens using the RNeasy Plus Universal Mini Kit (Qiagen, Valencia, CA, USA), and RNA purity was determined using NanoDrop2000 (Thermo Fisher Scientific, Wilmington, DE, USA). The A260/A280 ratios for all specimens were > 1.90. After extraction, 1 μg of total RNA was reverse-transcribed to cDNA, and RT-qPCR was performed using a 7500 Real-Time PCR System (Applied Biosystems, Foster City, CA, USA). TaqMan gene expression assays (Applied Biosystems) were used to detect NGF (assay ID: Rn01533872_m1), BDNF (assay ID: Rn02531967_s1), NT-3 (assay ID: Rn00579280_m1), GAP-43 (assay ID: Rn01474579_m1), IL-6 (assay ID: Rn01410330_m1), TNF (assay ID: Rn99999017_m1), Bcl-2 (assay ID: Rn99999125_m1), and Bax (assay ID: Rn01480161_g1).
Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) (assay ID: Rn01775763_g1) was used as an endogenous reference gene13. The data obtained were analyzed using the comparative threshold cycle method, and the target gene expression was normalized to that of GAPDH. The values of the calibration specimens (intact DRG specimens) were set to 1, and the values of the specimens in the rMS and CON groups at each post-injury time point were shown relative to those of the calibration specimens.
Kinematic analysis
Based on our previous study32, we utilized a 3D motion analysis system (Kinema Tracer System; Kissei Comtec, Nagano, Japan) for the kinematic analysis. Following anesthesia induction with 2% isoflurane, colored hemispheric markers were attached to specific bilateral anatomical landmarks on the skin, including the anterior superior iliac spine, greater trochanter, knee joint, lateral malleolus, and fifth metatarsophalangeal joint. The fourth toes were marked with pink ink, and the rats walked on a treadmill at a speed of 12 m/min, while four motion-capture cameras recorded 10 consecutive steps. We analyzed the ankle and toe angles during the toe-off phase, which is the phase in which the foot loses its last contact with the ground. The ankle angle was determined as the angle formed between the lines connecting the knee joint to the lateral malleolus and the lateral malleolus to the fifth metatarsophalangeal joint. The toe angle was defined as the angle formed between the line extending from the lateral malleolus to the fifth metatarsophalangeal joint and the line connecting the fifth metatarsophalangeal joint to the tip of the fourth toe. Subsequently, a data processing software was used to calculate the mean values of the ankle and toe angles.
Electrophysiological analysis
After kinematic analysis at 8 weeks, the rats were anesthetized with mixed anesthetics, and electrophysiological assessments were performed using an electromyogram measuring system (Neuropack S1 MEB-9404; Nihon Kohden, Tokyo, Japan). Sciatic nerves were then stimulated proximal to the injury site, and CMAPs were recorded in the gastrocnemius muscle, which is innervated by the tibial nerve. The amplitude and latency of CMAPs were expressed as the ratio of the injured side to the non-injured side.
Axon regeneration evaluation
An autografted sciatic nerve specimen was dissected 8 weeks after surgery. The specimens were initially immersed overnight in 1.44% paraformaldehyde and 1% glutaraldehyde in 0.036 M phosphate buffer (pH = 6.8) at a temperature of 4 °C. Subsequently, samples were fixed with 1% osmium tetroxide in 0.1 M phosphate buffer for 120 min. Specimens were dehydrated using graded ethanol and embedded in EPON (Luveak, Nacalai Tesque, Kyoto, Japan). Transverse sections (thickness of 1 μm) taken from the middle of the autografted nerve were stained with toluidine blue solution and viewed under a light microscope (Eclipse 80i; Nikon, Tokyo, Japan). Subsequently, the density of myelinated fibers was assessed in randomly selected areas covering 80,000 mm2 within one cross-section per rat using the ImageJ software, ensuring that these areas represented ≥ 30% of the total image area32. The results were presented as myelinated fiber densities (fibers/mm2).
Ultrathin cross-sectional slices of the same tissues stained with uranyl acetate and lead citrate were observed under a transmission electron microscope (Model H-7000; Hitachi High-Technologies, Tokyo, Japan). According to a previous study36, 10 random microphotographs of each cross-section were taken at a magnification of 2000×, and the shortest diameter of myelinated nerve fibers (a) and axons diameter (b) were measured using ImageJ. The myelin sheath thickness (c) of each myelinated nerve fiber was determined using the following formula: (a−b)/2. The means of the myelinated nerve diameter, axon diameter, and myelin sheath thickness were calculated by averaging three parameters (a, b, and c) for each cross-section.
Wet muscle weight
After removing the regenerated nerve, the bilateral gastrocnemii were dissected, detached from the bone at their origin and insertion points, and immediately weighed using a digital scale. The wet muscle weight was expressed as the ratio of the injured side to the non-injured side.
Statistical analysis
All statistical analyses were conducted using JMP Pro 15 software (SAS Institute, Cary, NC, USA). The data are presented as means ± standard deviations. Model assumptions were checked using the Shapiro–Wilk normality test and Levene’s test for homogeneity of variance. All data were normally distributed and showed homogeneity of variance. Differences between the rMS and CON groups were assessed using Student’s t-test, while comparisons with the intact groups were assessed using Dunnett’s test. Statistical significance was set at p < 0.05.
Data availability
The datasets used and/or analyzed in this study are available upon request from the corresponding author.
Abbreviations
- 3D:
-
Three-dimensional
- Bax:
-
Bcl2-associated X protein
- Bcl-2:
-
B-cell CLL/lymphoma 2
- BDNF:
-
Brain-derived neurotrophic factor
- ChAT:
-
Choline acetyltransferase
- CMAP:
-
Compound muscle action potential
- CON:
-
Control
- DRG:
-
Dorsal root ganglion
- EMG:
-
Electromyography
- GAP-43:
-
Growth-associated protein 43
- GAPDH:
-
Glyceraldehyde 3-phosphate dehydrogenase
- HE:
-
Hematoxylin and eosin
- IL-6:
-
Interleukin 6
- MN:
-
Motor neuron
- NeuN:
-
Neuronal nuclei
- NGF:
-
Nerve growth factor
- NT-3:
-
Neurotrophin-3
- PBS:
-
Phosphate-buffered saline
- PNI:
-
Peripheral nerve injury
- rMS:
-
Repetitive magnetic stimulation
- RT-qPCR:
-
Reverse transcription-quantitative polymerase chain reaction
- TNF:
-
Tumor necrosis factor
References
Wang, M. L., Rivlin, M., Graham, J. G. & Beredjiklian, P. K. Peripheral nerve injury, scarring, and recovery. Connect Tissue Res. 60, 3–9 (2019).
Agthong, S., Kaewsema, A. & Chentanez, V. Inhibition of p38 MAPK reduces loss of primary sensory neurons after nerve transection. Neurol. Res. 34, 714–720 (2012).
Lin, J. et al. The GDF11 promotes nerve regeneration after sciatic nerve injury in adult rats by promoting axon growth and inhibiting neuronal apoptosis. Front. Bioeng. Biotechnol. 9, 803052 (2022).
Hart, A. M., Terenghi, G. & Wiberg, M. Neuronal death after peripheral nerve injury and experimental strategies for neuroprotection. Neurol. Res. 30, 999–1011 (2008).
Palispis, W. A. & Gupta, R. Surgical repair in humans after traumatic nerve injury provides limited functional neural regeneration in adults. Exp. Neurol. 290, 106–114 (2017).
Qian, Y. et al. Advances in electrical and magnetic stimulation on nerve regeneration. Regen. Med. 14, 969–979 (2019).
Xu, S. & Ito, A. Expanding the targets of therapeutic electrophysical stimulation—for the advancement of peripheral nerve regenerative rehabilitation. Curr. Opin. Biomed. Eng. 28, 100515 (2023).
Grassi, C. et al. Effects of 50 Hz electromagnetic fields on voltage-gated Ca2+ channels and their role in modulation of neuroendocrine cell proliferation and death. Cell Calcium 35, 307–315 (2004).
Ghosh-Roy, A., Wu, Z., Goncharov, A., Jin, Y. & Chisholm, A. D. Calcium and cyclic AMP promote axonal regeneration in Caenorhabditis elegans and require DLK-1 kinase. J. Neurosci. 30, 3175–3183 (2010).
Jiang, J.-L., Guo, X.-D., Zhang, S.-Q., Wang, X.-G. & Wu, S.-F. Repetitive magnetic stimulation affects the microenvironment of nerve regeneration and evoked potentials after spinal cord injury. Neural Regen. Res. 11, 816–822 (2016).
Chen, J., Zhou, X.-J. & Sun, R.-B. Effect of the combination of high-frequency repetitive magnetic stimulation and neurotropin on injured sciatic nerve regeneration in rats. Neural Regen. Res. 15, 145–151 (2020).
Zhivolupov, S. A. et al. Impulse magnetic stimulation facilitates synaptic regeneration in rats following sciatic nerve injury. Neural Regen. Res. 7, 1299–1303 (2012).
Xu, S. et al. Ultrasound therapy of injury site modulates gene and protein expressions in the dorsal root ganglion in a sciatic nerve crush injury rat model. Ultrasound Med. Biol. 48, 2502–2511 (2022).
Stadelman, C. et al. Expression of cell death-associated proteins in neuronal apoptosis associated with pontosubicular neuron necrosis. Brain Pathol. 11, 273–281 (2001).
Perlman, H., Zhang, X., Chen, M. W., Walsh, K. & Buttyan, R. An elevated bax/bcl-2 ratio corresponds with the onset of prostate epithelial cell apoptosis. Cell Death Differ. 6, 48–54 (1999).
Pei, B.-A., Zi, J.-H., Wu, L.-S., Zhang, C.-H. & Chen, Y.-Z. Pulsed electrical stimulation protects neurons in the dorsal root and anterior horn of the spinal cord after peripheral nerve injury. Neural Regen. Res. 10, 1650–1655 (2015).
Han, S., Kim, D., Kim, H., Park, J. W. & Youn, I. Electrical stimulation inhibits cytosine arabinoside-induced neuronal death by preventing apoptosis in dorsal root ganglion neurons. Neuroreport 27, 1217–1224 (2016).
McKay-Hart, A., Brannstrom, T., Wiberg, M. & Terenghi, G. Primary sensory neurons and satellite cells after peripheral axotomy in the adult rat: Timecourse of cell death and elimination. Exp. Brain Res. 142, 308–318 (2002).
Menorca, R. M. G., Fussell, T. S. & Elfar, J. C. Nerve physiology: Mechanisms of injury and recovery. Hand Clin. 29, 317–330 (2013).
Skaper, S. D. Neurotrophic factors: An overview. Methods Mol. Biol. 1727, 1–17 (2018).
Menorca, R. M. G., Fussell, T. S. & Elfar, J. C. Peripheral nerve trauma: Mechanisms of injury and recovery. Hand Clin. 29, 317–330 (2013).
Chen, Z.-L., Yu, W.-M. & Strickland, S. Peripheral regeneration. Annu. Rev. Neurosci. 30, 209–233 (2007).
Verge, V. M., Tetzlaff, W., Richardson, P. M. & Bisby, M. A. Correlation between GAP43 and nerve growth factor receptors in rat sensory neurons. J. Neurosci. 10, 926–934 (1990).
Benowitz, L. I. & Routtenberg, A. GAP-43: An intrinsic determinant of neuronal development and plasticity. Trends Neurosci. 20, 84–91 (1997).
Anderson, K. D., Merhege, M. A., Morin, M., Bolognani, F. & Perrone-Bizzozero, N. I. Increased expression and localization of the RNA-binding protein HuD and GAP-43 mRNA to cytoplasmic granules in DRG neurons during nerve regeneration. Exp. Neurol. 183, 100–108 (2003).
Zhang, J.-M. & An, J. Cytokines, inflammation and pain. Int. Anesthesiol. Clin. 45, 27–37 (2007).
Fregnan, F., Muratori, L., Simões, A. R., Giacobini-Robecchi, M. G. & Raimondo, S. Role of inflammatory cytokines in peripheral nerve injury. Neural Regen. Res. 7, 2259–2266 (2012).
Tang, G. et al. Reduced inflammatory factor expression facilitates recovery after sciatic nerve injury in TLR4 mutant mice. Int. Immunopharmacol. 55, 77–85 (2018).
Gross, A., McDonnell, J. M. & Korsmeyer, S. J. BCL-2 family members and the mitochondria in apoptosis. Genes Dev. 13, 1899–1911 (1999).
Adams, J. M. & Cory, S. The Bcl-2 protein family: Arbiters of cell survival. Science 281, 1322–1326 (1998).
Strasser, A., O’Connor, L. & Dixit, V. M. Apoptosis signaling. Annu. Rev. Biochem. 69, 217–245 (2000).
Wang, T. et al. Functional evaluation outcomes correlate with histomorphometric changes in the rat sciatic nerve crush injury model: A comparison between sciatic functional index and kinematic analysis. PLoS One 13, e0208985 (2018).
Tavee, J. Nerve conduction studies: Basic concepts. Handb. Clin. Neurol. 160, 217–224 (2019).
Mert, T., Metin, T. O., Sahin, E., Yaman, S. & Sahin, M. Neuroprotective and anti-neuropathic actions of pulsed magnetic fields with low frequencies in rats with chronic peripheral neuropathic pain. Brain Res. Bull. 177, 273–281 (2021).
Kohno, T. et al. Neuromodulation through magnetic fields irradiation with AT-04 improves hyperalgesia in a rat model of neuropathic pain via descending pain modulatory systems and opioid analgesia. Cell. Mol. Neurobiol. 43, 4345 (2023).
Wang, T. et al. Low-intensity pulsed ultrasound prompts both functional and histologic improvements while upregulating the brain-derived neurotrophic factor expression after sciatic crush injury in rats. Ultrasound Med. Biol. 47, 1586–1595 (2021).
Kawai, H. et al. Ultrasound therapy for a week promotes regeneration and reduces pro-inflammatory macrophages in a rat sciatic nerve autograft model. Sci. Rep. 13, 11494 (2023).
Friese, A. et al. Gamma and alpha motor neurons distinguished by expression of transcription factor Err3. Proc. Natl. Acad. Sci. U. S. A. 106, 13588–13593 (2009).
Shneider, N. A., Brown, M. N., Smith, C. A., Pickel, J. & Alvarez, F. J. Gamma motor neurons express distinct genetic markers at birth and require muscle spindle-derived GDNF for postnatal survival. Neural Dev. 4, 42 (2009).
Keiner, D., Kühn, J. P., Huber, A. & Oertel, J. Antiapoptotic effect of granulocyte-colony stimulating factor after peripheral nerve trauma. World Neurosurg. 129, e6–e15 (2019).
Acknowledgements
This study was supported by JSPS KAKENHI grants (JP21K19709 and JP24K02797). We would like to thank Keiko Okamoto-Furuta and Haruyasu Kohda (Division of Electron Microscopic Study, Center for Anatomical Studies, Graduate School of Medicine, Kyoto University) for their technical assistance with the electron microscopy, and Editage (www.editage.jp) for English language editing. In addition, SX would like to thank the Otsuka Toshimi Scholarship Foundation for providing financial support through a scholarship during this study.
Author information
Authors and Affiliations
Contributions
AI designed the study and secured funding. SX performed the experiments, analyzed the data, and wrote the manuscript. ZZ performed the experiments and analyzed the data. SX, AI, ZZ, RN, CT, FM, HK, and TA read, edited and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, S., Ito, A., Zhao, Z. et al. Repetitive magnetic stimulation prevents dorsal root ganglion neuron death and enhances nerve regeneration in a sciatic nerve injury rat model. Sci Rep 14, 19016 (2024). https://doi.org/10.1038/s41598-024-69251-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69251-4
- Springer Nature Limited