Abstract
Although exercise is beneficial for chronic musculoskeletal pain (CMP), the optimal type and amount of exercise are unclear. This study aimed to determine the impact of circuit training that combines aerobic and resistance exercises on adult women with CMP. A total of 139 women with CMP underwent circuit training for 3 months and were asked to complete the following questionnaires at baseline and 3 months later: Numeric Rating Scale (NRS), Pain Catastrophizing Scale (PCS), Roland-Morris Disability Questionnaire (RDQ), Shoulder36, and Knee injury and Osteoarthritis Outcome Score (KOOS). Significant improvements were observed in NRS, PCS, RDQ, and KOOS activities of daily living (ADL) scores after the intervention relative to baseline (p < 0.0001, p = 0.0013, 0.0004, and 0.0295, respectively), whereas shoulder function did not improve. When considering the impact of exercise frequency, NRS scores improved regardless of exercise frequency. Furthermore, PCS, RDQ, and KOOS scores improved in participants who exercised at least twice a week (24 sessions over the course of 3 months). In conclusion, CMP, pain catastrophizing, and physical function in adult female fitness club participants with CMP of NRS 4 or higher improved after 3 months of aerobic-resistance circuit training.
Similar content being viewed by others
Introduction
Chronic musculoskeletal pain (CMP) is a multifactorial condition that negatively impacts not only physical function, but also mental functioning and quality of life1. The National Livelihood Survey in Japan reported that low back pain, shoulder stiffness, and joint pain are the most common symptoms experienced by the general Japanese population2. Approximately 20–30% of the adult population has chronic pain3,4 and the socio-demographic factors associated with chronic pain include female sex and older age5.
The pathology of CMP involves intricately related biological and psychosocial factors because it has been linked to numerous physical and mental conditions4. Changes in these factors resulting from CMP include muscle weakness associated with reduced daily activity, somnipathy, malnutrition, drug dependence, dependence on family, isolation from family or society, decline in job performance, and economic burden6,7. Pain conditions are reportedly responsible for 21% of years lived with disability (YLDs)8. CMP frequently occurs as a result of a disease or injury. However, it is not merely an accompanying symptom, but rather a separate condition in its own right, with its own medical definition and taxonomy9. In addition, pain catastrophizing is an important psychosocial predictor of the course and experience of chronic pain10, and it has been found to be inversely related to muscular endurance11. This tendency has been proven to negatively impact the neuromuscular, cardiovascular, immune, and neuroendocrine systems12. Therefore, research on CMP treatments, which not only relieve pain but also improve physical and psychosocial factors, is important13.
Exercise therapy, encompassing a wide range of interventions such as general (aerobic) exercise, specific body region exercises for strengthening and flexibility, continuing normal physical activities, and increasing general physical activity levels, is a core treatment option for patients with CMP1. Exercise therapy is particularly important given that existing pharmacological options for chronic pain are often limited by side effects, abuse potential, and overall efficacy14. There is little evidence supporting one particular type and amount of exercise for CMP15. Aerobic exercise has been shown to decrease pain sensitivity in patients with CMP16. However, a systematic review found that unlike in resistance training, aerobic exercise programs showed no effect in reducing chronic low back pain17. Previous studies have demonstrated that combination exercise training, which involves aerobic and strength exercise training, is likely to provide the individual effects unique to aerobic exercise and resistance training, respectively18. Combined aerobic and resistance training can improve lean body mass, muscular strength, body composition, and glycemic control in older adults19,20,21. Moreover, a meta-analysis showed that combination training has a greater effect on cognitive function in older adults than aerobic exercise training alone22. Circuit training is defined as the performance of 6–12 exercises in sequential order with little to no break between them23. A novel type of circuit training program involves a combination of the two aforementioned training modalities, namely, a resistance training set followed immediately by an aerobic exercise interval (a simultaneous aerobic-resistance training method). The effects of circuit training on several chronic disorders have been reported, and positive effects have been demonstrated on body composition, including reductions in body fat and body mass index (BMI)24. The aerobic-resistance circuit training program can elicit a greater cardiorespiratory response and similar muscular strength gains with less time commitment compared with a traditional resistance training program combined with aerobic exercise25. Moreover, this type of circuit training program was found to be feasible and safe in men with post-myocardial infarction26. The nature of circuit training may provide an effective, well-rounded exercise program to improve the overall fitness of older adults21. There have only been few reports on the effects of aerobic-resistance circuit training on pain. Circuit training has been reported to decrease postoperative pain after total knee arthroplasty27 and pain perception in women with fibromyalgia28. Although these studies focused on postoperative pain and pain perception, the effect of aerobic-resistance circuit training for reducing CMP is still unknown.
Recent evidence also suggests that older women are more likely to live with chronic pain than older men9,29. In addition to a female preponderance for chronic pain, women consistently report lower pain thresholds, lower pain tolerance, and greater unpleasantness with pain with different analgesic sensitivity30. Previous reports have indicated that there might be sex-specific mediators affecting the association of demographic variables with pain intensity and physical function, suggesting the need for a sex-specific approach when treating chronic pain31. This highlights that it is beneficial to focus on one sex only when examining the effects of exercise therapy, and since CMP is more common in women, there is a greater clinical need for treatment among women.
We hypothesized that aerobic-resistance circuit training would have positive effects on pain, pain catastrophizing, and physical function in women with CMP. To investigate this, the present questionnaire-based cohort study aimed to evaluate the effects of aerobic-resistance circuit training for 3 months in women with CMP who became new members of fitness facilities.
Results
Participant characteristics
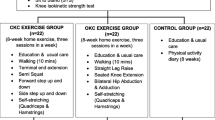
Participants were adult women who became new members of fitness facilities and performed circuit training for 3 months (“the intervention”) without any restrictions on exercise frequency. A total of 139 women with CMP who completed a set of questionnaires, including the numeric rating scale (NRS) for CMP, pain catastrophizing scale (PCS), Roland-Morris disability questionnaire (RDQ), Shoulder36, and Knee injury and Osteoarthritis Outcome Score (KOOS), before and 3 months after the intervention (Fig. 1). The baseline characteristics of the participants are presented in Table 1. The mean age was 63.1 years (SD = 10.8), and the mean NRS score was 5.3 (SD = 1.5).
Effects of exercise on pain and associated factors
We analyzed the change in pain after the intervention, as well as psychological and physical assessments (Table 2). Significant improvements were noted in the mean NRS score and number of pain sites after the intervention relative to baseline (p < 0.0001 and p = 0.0024, respectively). The prevalence of pain in the lower back and shoulder were significantly decreased (p = 0.0196 and 0.0280, respectively). With regard to pain catastrophizing, rumination, magnification, helplessness, and total PCS score were significantly improved after the intervention relative to baseline (p = 0.0017, 0.0047, 0.0387, and 0.0013, respectively). Physical function also improved after circuit training, as reflected in the RDQ and KOOS activities of daily living (ADL) scores (p = 0.0004 and 0.0295, respectively). In contrast, Shoulder36 scores did not change significantly after the intervention relative to the baseline. The achievement rates of minimal clinically important difference (MCID) were analyzed in the features with significant improvements such as NRS, PCS Total, RDQ, and KOOS ADL, each of which was based on past reports of satisfactory outcomes, as follows: NRS reduction of 1 point32, PCS reduction of 38%33 RDQ reduction of 2 points34, and KOOS ADL increase of more than 835. Meanwhile, the MCID for NRS was achieved in 60.4% of the participants, and those for PCS, RDQ, and KOOS ADL were achieved in 35.3%, 30.9%, and 18.0% of the participants, respectively.
Effect of exercise dose on NRS, PCS, RDQ, Shoulder36, and KOOS scores
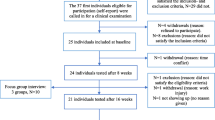
We further divided the participants into three groups according to exercise frequency: the bottom 33% of participants exercised ≤ 23 times for 3 months and were assigned to the low-dose group (n = 48); the middle 33% of participants exercised 24–33 times for 3 months and were assigned to the moderate-dose group (n = 46); and the top 33% of participants exercised ≥ 34 times for 3 months and were assigned to the high-dose group (n = 45) according to the previously reported studies36,37 with modification. We evaluated the effects of exercise on pain and its associated functions according to dose. The results are summarized in Table 3. NRS scores were significantly improved in all three groups after the intervention relative to baseline (p = 0.0008, 0.0005, and 0.0002, respectively). The total score, as well as rumination and magnification domain scores, of PCS were significantly lower in the high-dose group after the intervention (p = 0.0091, 0.0300, and 0.0196, respectively). The total score and rumination domain score also improved in the moderate-dose group (p = 0.0190 and p = 0.0258, respectively). However, no improvement was observed in the low-dose group. Significant improvements were observed in RDQ scores for the moderate-and high-dose groups after the intervention relative to baseline (p = 0.0123 and 0.0009, respectively), but no significant change was observed in the low-dose group. Next, we evaluated the change in the Shoulder36 and KOOS scores depending on exercise frequency. None of the Shoulder36 domain scores differed significantly between the groups. With regard to KOOS scores, symptoms, sports, and QOL domain scores were significantly improved in the moderate-dose group (p = 0.0159, 0.0061, and 0.0423, respectively), and pain and ADL domain scores were significantly improved in the high-dose group (p = 0.0236 and 0.0046, respectively), whereas significant changes were not observed in the low-dose group.
Collectively, these results suggest that NRS scores were significantly improved regardless of exercise frequency, and PCS, RDQ, and KOOS domain scores were significantly improved in the moderate- and high-dose groups, but not in the low-dose group.
We also investigated intergroup differences in the achievement rates of the MCID. In all groups, more than half of the participants achieved MCID for the NRS, especially in the high-dose group who had an achievement rate of 71.1%. However, there was no significant difference compared to the other two groups. Regarding the other MCIDs, the achievement rate of the low-dose group tended to be low in each MCID; however, no significant difference was observed.
Odds ratios (ORs) for withdrawal from the fitness facilities after the 3-month follow-up
The results obtained thus far suggest that continuous exercise is important for improving CMP and associated functions; therefore, we further investigated the predictors of dropout. Within 3 months of the study period, 20 people withdrew from the fitness facilities. Table 4 shows the multivariable logistic regression model for dropout after the 3-month follow-up, and the exercise frequency was associated with reduced odds of dropout (OR: 0.94 [95% CI 0.90–0.99], p = 0.0127). We further evaluated the threshold levels associated with dropout using the receiver operating characteristic (ROC) method. The appropriate cut-off point for the exercise frequency was 25 sessions over the course of 3 months, with a specificity of 62.2% and a sensitivity of 70.0% (Fig. 2). The area under the ROC curve (AUC) was 0.68. This suggests that exercising at least 25 times in 3 months, which was equivalent to exercise twice a week, was a predictor of preventing dropout of the circuit training.
Discussion
To the best of our knowledge, this study is the first to assess the effects of an aerobic-resistance circuit training regimen on pain, pain catastrophizing, and physical function in adult women with CMP. The main findings of this study indicate that CMP, psychological vulnerability, and physical function improved after 3 months of circuit training in Japanese women.
To investigate the effect of exercise on pain and its associated factors, we focused on the low back, shoulder, and knee in this study, given the high prevalence of CMP at these sites3,38. We also used MCID as a satisfactory outcome to assess correlations between exercise frequency and improvement in pain-associated factors. MCID was first described by Jaeschle et al.39 as “the smallest difference in score in the domain of interest which patients perceive as beneficial and which would mandate, in the absence of troublesome side effects and excessive cost, a change in the patient’s management.” It is a useful benchmark for determining whether patients show sufficient improvement to notice a real clinical difference. In this study, the participants showed a significant improvement in the mean NRS score beyond the MCID. Some studies have reported that combined exercise improves low back pain and knee function. For instance, in one study, a general rehabilitation program combining strength, stretching, endurance, balance, and stabilization exercises in patients with chronic low back pain had significant effects on pain and disability40. A systematic review concluded that combined exercises are effective for improving functional limitations resulting from knee osteoarthritis41. Similar to these reports, a significant reduction in low back pain and improvement in low back and knee function were also observed in the present study. Previous reports on exercise for women with CMP showed that the combined training of neuromuscular exercise and back care counseling was effective for recurrent non-specific low back pain42, and resistance training was also effective for chronic neck pain43. In this study, it was predicted that circuit training would positively affect women with CMP. The prevalence of shoulder pain was also significantly decreased after the intervention relative to baseline, but no significant improvement was observed in shoulder function. This might be explained by the high baseline score for shoulder function, suggesting that many participants in this study had shoulder pain but not shoulder disability. According to Dunn et al.44, shoulder pain is not related to cuff tear severity, but might be correlated with comorbidities, lower education level, and ethnicity. This previous report may explain the high shoulder score of Shoulder36 in this study.
In this study, the effects of the exercise dose on the NRS, PCS, RDQ, Shoulder36, and KOOS scores were also examined. Although scores of PCS, RDQ, and KOOS significantly decreased in the moderate-and high-dose groups, these effects were not observed in the low-dose group. Furthermore, participants who exercised less than twice a week were less likely to achieve MCID for pain and its associated factors. This suggests that circuit training was more effective in participants who exercised more than 24 times in a 3-month period than in those who exercised less. Participating in training 24 times in 3 months is equivalent to exercise twice a week. Our findings collectively indicate that aerobic-resistance circuit training in adult women with CMP had a significant association with reducing pain, and continuous exercise for at least twice a week is required to improve psychological vulnerability and physical disability. Interestingly, there was no significant change in the shoulder function. There is a lack of studies in the literature on the impact of exercise dose on pain14, and the American College of Sports Medicine (ACSM) does not have a specific exercise recommendation to address pain. The ACSM’s Position Stand recommends 30 min of moderate-intensity walking exercise for 5 days per week (or 150 MET minutes) to sufficiently sustain adequate cardiorespiratory, musculoskeletal, and neuromotor fitness for healthy adults45. Although long-term adherence to this regimen would be ideal, it is likely too high of a starting point for individuals with chronic pain, especially for those suffering from movement-induced pain and movement-associated fear avoidance behavior46. Therefore, it is important to carefully examine the optimal exercise doses to reduce pain. Given that previous studies reported that pain can be reduced by exercising twice47 or 3 times per week48, we divided participants into three groups based on exercise frequency. The participants were divided into two groups: less than twice (low-dose group), more than twice and slightly less than 3 times (moderate-dose group), and more than 3 times per week (high-dose group). Circuit training was more effective in the moderate-and high-dose groups than in the low-dose group, and 30 min of continuous exercise for at least twice a week was found to be associated with improvement in both CMP and physical function.
In the results of OR for withdrawal from the fitness facilities after the 3-month follow-up, exercise frequency was significantly associated with dropout from the fitness facilities. Furthermore, the cutoff point was 25 times greater in the 3-month period, equivalent to twice a week. In a randomized comparative trial of combined training for adults with chronic nonspecific low back pain, participants exercised twice a week for 1.5 h49. This contrasts with the present study, in which a sufficient effect was obtained even with 30-min exercise sessions twice a week. This result suggested the time efficiency of the circuit program, as shown in the comparison with the combined program in a previous report25. In addition, as reported previously, people with CMP appear responsive to lower exercise dosage. These are important indications, given that “lack of time’ is the primary reason people do not exercise50. Since adherence to circuit training was the key predictor of improved CMP and prevention of dropout in the results of this study, future efforts should focus on strategies to improve adherence. Exercise programs that integrate both resistance exercise and aerobic training have increased in demand because of their ability to meet exercise guidelines in a time-efficient manner51. Moreover, circuit training allows numerous people to participate in the same training session because of the low total duration of the exercises24,25, which promotes high retention and adherence52. Exercising with others has also been reported to be useful for preventing depression in older adults53. In addition, the safety of aerobic-resistance circuit training has been demonstrated in men with post-myocardial infarction26. Taken together, circuit training is sufficiently safe and may reduce the dropout rate by promoting exercise with other participants without requiring major time commitment.
Patients with CMP complain of widespread negative consequences, such as significant pain intensity, depressive symptoms, weakness, sleep-related problems, sick leave, loss of enjoyment of life in general, and decreased emotional well-being54. Physiological pain with organic insults can have negative effects on emotions and cognitive function, and conversely, a negative emotional state can lead to increased pain through the central pain pathway55. Several theoretical frameworks on pain catastrophizing and pain-related outcomes have been proposed56,57. A multidisciplinary approach that included exercise therapy, psychotherapy, and patient education reportedly improved pain, PCS, and physical function in patients with CMP7. Though the result was similar to the current study, the difference is whether the place of treatment was a hospital or a fitness club. A multidisciplinary approach requires a large number of medical staff, including orthopedic surgeons, psychiatrists, nurses, physical therapists, clinical psychologists, pharmacists, and nutritionists, and it was effective for patients who visited the hospital for pain treatment. For subjects motivated to exercise, such as fitness club members, circuit training seems to be effective and has an advantage in terms of medical costs, compared with a multidisciplinary approach. CMP is a substantial medical health issue, and the financial costs to society are enormous, with current estimates running at more than €200 billion per annum in Europe and $150 billion per annum in the United States58. According to research performed by the American Chamber of Commerce in Japan (ACCJ) in 2011, estimated economic losses due to pain were ¥35 million (approximately $340 thousand) a year, excluding treatment costs2. Therefore, exercise is important not only for improving CMP and associated functions, but also for improving quality of life and healthcare costs. In the present study, 35.3% of all patients with CMP with NRS scores ≥ 4 used oral analgesics. Although the proportion of oral analgesic use did not significantly differ by exercise frequency, there was a tendency for higher oral analgesic use with lower exercise frequency (data not shown). Continuous exercise may help reduce medical expenses, and fitness programs that incorporate both aerobic fitness and strength training would cost little to implement in terms of equipment and facilities59.
The present study has several limitations. First, our sample population consisted of only adult females and was mostly Japanese. Future studies should examine whether our results are generalizable to men and people of other ages and races. The average age of the participants in the current study was 63.1 years. In this regard, older age has been reported as a predictor of poor outcomes in patients with neck pain treated by physical therapy60. Furthermore, African-Americans with chronic pain reportedly have different rehabilitation outcomes than Caucasians, and Asians have higher pain catastrophizing and pain severity than European Canadians61. Second, a limitation of the present study was the variation in exercise frequency in each group. In the low-dose group, exercise frequency varied from 3 to 23 times. In addition, due to the nature of the observational study, it was not possible to include a control group (e.g., without intervention). Third, all outcomes were based on subjective evaluations from questionnaires and were not objectively evaluated. As such, evaluations of muscle strength, physical performance, and pressure pain threshold are necessary in the future. Fourth, our inclusion and exclusion criteria and screening methods may have impacted the external validity of our findings. Some potentially important demographic variables (i.e., education, income, and employment status) were not surveyed. Population-based studies of chronic pain have consistently shown that chronic pain occurrence is inversely related to the socioeconomic status, with evidence that people living in adverse socioeconomic circumstances experience more chronic pain and greater pain severity, independent of other demographic and clinical factors5. In this study, all the participants were fitness club members and were presumed to have a favorable socio-economic status. Finally, the follow-up period was relatively short. More studies with longer follow-up periods are needed to evaluate long-term outcomes.
In conclusion, CMP, pain catastrophizing, and physical function in adult female fitness club participants with a CMP of NRS 4 or higher improved after 3 months of aerobic-resistance circuit training. The subjects included 139 out of 2600 new fitness club members, with an average age of 63.1 years. It was suggested that circuit training has the potential for immediate and high clinical impact as a low-cost, non-pharmacological, and non-invasive treatment.
Methods
Participants
The structured combined exercise training facilities (Curves Japan Co., Ltd.), to which the participants of the study belonged, were fitness facilities that held 30-min circuit training sessions for women in Japan. Participants of the present cohort study were women who became members of the above-mentioned facilities. The first self-administered questionnaire regarding medical history and pain-associated functions was distributed at the time of enrollment to 2600 members of 132 facilities in Japan, and responders were 1347 people.
The inclusion criteria were participants who have CMP with an NRS score of 4 or higher. The question related to the presence of CMP was “Please show all parts of the body that have experienced persistent or recurrent pain over the last 3 months or more on the image below.” Regarding the answers, participants were asked to “check the painful parts of the body” or indicate “no pain,” based on the health condition at the time of answering the questionnaire. The Michigan Body Map62, a self-report measure to assess areas of the body with chronic pain, was used to assess the location of pain and number. Multiple answers were allowed for the location of pain. Chronic pain was defined as pain that persisted for more than 3 months, based on a previous report6. Participants were asked the NRS score of the single most painful site. The exclusion criteria were as follows: missing data for height, weight, age, CMP, NRS, exercise frequency, errors in these measurements, or clear entry errors (n = 232), withdrawal from the fitness facilities (n = 58), absence of CMP on enrollment based on responses to the self-administered questionnaire (n = 238); and CMP with NRS score < 4 (n = 626). The second self-administered questionnaire was administered to 193 members 3 months after admission. Consequently, 165 people responded to the second self-administered questionnaires, and 139 members, excluding those with missing data, were included in the present study. Pain with an NRS score ≥ 4 is subject to drug treatment63 and categorized as moderate or severe pain64. Accordingly, we defined participants with an NRS score of ≥ 4 as having CMP in need of treatment (Fig. 1).
Study design
This was a multicenter cohort study that examined the effects of aerobic-resistance circuit training for 3 months in women with CMP. All procedures were approved by the ethics committee of Osaka University. Written informed consent was obtained from all the participants prior to their participation. All primary and secondary pre-specified efficacy outcomes are reported in the present manuscript, and all methods were performed in accordance with the relevant guidelines and regulations.
Exercise regimen
The number of admissions to fitness facilities was examined for the first 3 months after joining using an electronic admission management system. Since the number of admissions corresponds to the number of training sessions attended, the former was defined as the exercise frequency. To perform the aerobic-resistance circuit training, 12 individual exercise stations designed to work on all major muscle groups and 12 step boards were arranged alternatively in a circular manner. The circuit exercise alternated between 30 s of resistance exercise and 30 s of aerobic training, leading to a duration of 24 min. Combined with the 6-min stretching period, the training lasted for 30 min. The exercise involved stepping on a step board for the aerobic training while executing resistance training using 12 different hydraulic devices (chest press/seated row, squat, shoulder press/lateral pull, leg extension/leg curl, abdominal crunch/back extension, lateral lift, elbow flexion/extension, horizontal leg press, pectoral deck, oblique, hip abductor/adductor, gluteus), and was developed for women to increase their muscle strength. All participants performed both aerobic and resistance training in the same manner, allowing numerous people to participate in the same training session because of the short total duration of the exercises.
Outcomes
All participants completed validated questionnaires pertaining to their general health, physical activity levels, and physical function, which included 34 items (medical history, pain site, pain intensity, pain duration, pain frequency, current treatment of pain, smoking, reason for joining the fitness club, etc.) other than PCS, RDQ, Shoulder36, and KOOS. The participants took approximately 30 min to complete the questionnaire. Outcomes included changes in pain and associated factors, as follows: intensity of pain as assessed by NRS (0: no pain, 10: unbearable pain), number of pain sites, prevalence of chronic pain, pain catastrophizing as assessed by PCS (0: low level of catastrophic thinking, 52: high level of catastrophic thinking), low back pain-specific disability as assessed by RDQ (0: no limitation, 24: maximal limitation), shoulder function as assessed by Shoulder36 (0: maximal limitation, 4: no limitation), and knee function as assessed by KOOS (0: maximal limitation, 100: no limitation).
The NRS measures pain severity by asking the patient to select a number, and is considered one of the best single-item methods available to estimate pain intensity65.
Several assessment tools have been developed to quantify pain catastrophizing, the most commonly used of which is the PCS66. The PCS includes 13 items rated on a 5-point scale ranging from 0 (not at all true) to 4 (very true).” The items are divided across three subdomains: rumination (4 items, e.g., “When I have pain, I can’t keep it out of my mind”), magnification (3 items, e.g., “When I have pain, I keep thinking of other painful events”), and helplessness (6 items, e.g., “When I have pain, I feel like I can’t go on”).Items are summed across subdomains to derive a total score ranging from 0 to 52, with higher scores reflecting higher levels of catastrophic thinking67. Pain catastrophizing is the tendency to focus on and amplify pain sensations and feel helpless when pain occurs59.
The RDQ was designed in 198368 for use in primary care research to assess physical disability due to low back pain, and it is sensitive to changes in patients with mild to moderate disability69. The Japan Orthopaedic Association and the Japanese Shoulder Society jointly developed an original patient-reported outcome measure, Shoulder36, version 1.3, in 201070. Shoulder36 is a self-reported shoulder-specific instrument that evaluates shoulder function and consists of 36 questions that represent six domains: pain, range of motion (ROM), muscle strength, general health, activities of daily living (ADL), and ability of sports (Sports). Scores range from 0 to 4 in each domain, and summing the scores to obtain a total score is not permitted because the domains are not independent71. A strong association has been reported between the Simple Shoulder test and each domain in Shoulder36 in patients with rotator cuff tears, suggesting the usefulness of Shoulder36 as a patient-based scoring system in these patients72.
The KOOS is a 42-item joint-specific measure that was developed to assess short- and long-term outcomes in patients with knee injuries, as they are often at risk of developing knee osteoarthritis73. It consists of five domains that are scored separately from 0 (extreme problems) to 100 (no problems): symptoms, pain, activities of daily living (ADL), sport and recreation function (Sports), and knee-related quality of life (QOL).
Statistical analysis
All recorded data were entered into the electronic storage. Statistical analyses were performed using the JMP Pro 15 software (SAS Institute Inc., NC, USA). Normality of the data was assessed, and statistical significance was set at p < 0.05.
Categorical variables are presented as frequencies and percentages. Quantitative variables are presented as mean (SD). Outcomes were defined as changes between 3 months after intervention and baseline for NRS, number of pain sites, prevalence of CMP, PCS, RDQ, Shoulder36, and KOOS. Comparisons were performed between the baseline and 3 months after the intervention. Because most parameters were not normally distributed, continuous data were analyzed using the Wilcoxon signed-rank test. The McNemar test was used to analyze categorical variables. Fisher’s exact test was used to evaluate intergroup differences in MCID achievement.
Multivariable logistic regression analysis was performed to calculate the ORs for dropout of fitness facilities. The dependent variable was dropout (0 = no dropout, 1 = dropout) at 3 months after the 3-month follow-up period. The selection of potential predictor variables for that particular regression model was based on previous literature, including age and BMI as the cause of dropout74. The variables that showed a significant univariate association with dropping out (p < 0.1), such as exercise frequency and NRS at follow-up, were also selected as potential predictor variables. The inclusion of appropriate predictor variables in the final multivariate regression model was based on multicollinearity assessment and the strength of their univariate association with the primary outcome measure. In the final multivariate logistic regression model for dropout status, statistical significance was set at p < 0.05. The ROC method was used to determine the threshold levels associated with dropout. This method has the advantage of synthesizing information on the sensitivity and specificity for detecting improvement using an external criterion75. From the ROC curves, we computed the optimal cut-off point, corresponding to the maximum sum of sensitivity and specificity.
References
Jordan, J. L., Holden, M. A., Mason, E. E. & Foster, N. E. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD005956.pub2 (2010).
Sugai, K., Tsuji, O., Matsumoto, M., Nishiwaki, Y. & Nakamura, M. Chronic musculoskeletal pain in Japan (the final report of the 3-year longitudinal study): Association with a future decline in activities of daily living. J. Orthop. Surg. 25, 2309499017727945. https://doi.org/10.1177/2309499017727945 (2017).
Breivik, H., Collett, B., Ventafridda, V., Cohen, R. & Gallacher, D. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur. J. Pain 10, 287–333. https://doi.org/10.1016/j.ejpain.2005.06.009 (2006).
Dahlhamer, J. et al. Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 67, 1001–1006. https://doi.org/10.15585/mmwr.mm6736a2 (2018).
van Hecke, O., Torrance, N. & Smith, B. H. Chronic pain epidemiology and its clinical relevance. Br. J. Anaesth. 111, 13–18. https://doi.org/10.1093/bja/aet123 (2013).
Treede, R. D. et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 160, 19–27. https://doi.org/10.1097/j.pain.0000000000001384 (2019).
Takahashi, N., Takatsuki, K., Kasahara, S. & Yabuki, S. Multidisciplinary pain management program for patients with chronic musculoskeletal pain in Japan: A cohort study. J. Pain Res. 12, 2563–2576. https://doi.org/10.2147/jpr.S212205 (2019).
Vos, T. et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2163–2196. https://doi.org/10.1016/s0140-6736(12)61729-2 (2012).
Mills, S. E. E., Nicolson, K. P. & Smith, B. H. Chronic pain: A review of its epidemiology and associated factors in population-based studies. Br. J. Anaesth. 123, e273–e283. https://doi.org/10.1016/j.bja.2019.03.023 (2019).
Junghaenel, D. U., Schneider, S. & Broderick, J. E. Linguistic indicators of pain catastrophizing in patients with chronic musculoskeletal pain. J. Pain 18, 597–604. https://doi.org/10.1016/j.jpain.2017.01.001 (2017).
Larivière, C., Bilodeau, M., Forget, R., Vadeboncoeur, R. & Mecheri, H. Poor back muscle endurance is related to pain catastrophizing in patients with chronic low back pain. Spine 35, E1178-1186. https://doi.org/10.1097/BRS.0b013e3181e53334 (2010).
Campbell, C. M. & Edwards, R. R. Mind-body interactions in pain: The neurophysiology of anxious and catastrophic pain-related thoughts. Transl. Res. 153, 97–101. https://doi.org/10.1016/j.trsl.2008.12.002 (2009).
Turk, D. C. & Okifuji, A. Psychological factors in chronic pain: Evolution and revolution. J. Consult. Clin. Psychol. 70, 678–690. https://doi.org/10.1037//0022-006x.70.3.678 (2002).
Polaski, A. M. et al. The dosing of aerobic exercise therapy on experimentally-induced pain in healthy female participants. Sci. Rep. 9, 14842. https://doi.org/10.1038/s41598-019-51247-0 (2019).
Booth, J. et al. Exercise for chronic musculoskeletal pain: A biopsychosocial approach. Musculoskelet. Care 15, 413–421. https://doi.org/10.1002/msc.1191 (2017).
Öte Karaca, Ş, Demirsoy, N. & Günendi, Z. Effects of aerobic exercise on pain sensitivity, heart rate recovery, and health-related quality of life in patients with chronic musculoskeletal pain. Int. J. Rehabil. Res. 40, 164–170. https://doi.org/10.1097/mrr.0000000000000212 (2017).
Searle, A., Spink, M., Ho, A. & Chuter, V. Exercise interventions for the treatment of chronic low back pain: A systematic review and meta-analysis of randomised controlled trials. Clin. Rehabil. 29, 1155–1167. https://doi.org/10.1177/0269215515570379 (2015).
Sawada, S. S. et al. Combined aerobic and resistance training, and incidence of diabetes: A retrospective cohort study in Japanese older women. J. Diabetes Investig. 10, 997–1003. https://doi.org/10.1111/jdi.12973 (2019).
Villareal, D. T. et al. Aerobic or resistance exercise, or both, in dieting obese older adults. N. Engl. J. Med. 376, 1943–1955. https://doi.org/10.1056/NEJMoa1616338 (2017).
Maiorana, A., O’Driscoll, G., Goodman, C., Taylor, R. & Green, D. Combined aerobic and resistance exercise improves glycemic control and fitness in type 2 diabetes. Diabetes Res. Clin. Pract. 56, 115–123. https://doi.org/10.1016/s0168-8227(01)00368-0 (2002).
Takeshima, N. et al. Effect of concurrent aerobic and resistance circuit exercise training on fitness in older adults. Eur. J. Appl. Physiol. 93, 173–182. https://doi.org/10.1007/s00421-004-1193-3 (2004).
Colcombe, S. & Kramer, A. F. Fitness effects on the cognitive function of older adults: A meta-analytic study. Psychol. Sci. 14, 125–130. https://doi.org/10.1111/1467-9280.t01-1-01430 (2003).
Nunez, T. P. et al. Metabolic effects of two high-intensity circuit training protocols: Does sequence matter?. J. Exerc. Sci. Fit. 18, 14–20. https://doi.org/10.1016/j.jesf.2019.08.001 (2020).
Bocalini, D. S. et al. Effects of circuit-based exercise programs on the body composition of elderly obese women. Clin. Interv. Aging 7, 551–556. https://doi.org/10.2147/cia.S33893 (2012).
Myers, T. R., Schneider, M. G., Schmale, M. S. & Hazell, T. J. Whole-body aerobic resistance training circuit improves aerobic fitness and muscle strength in sedentary young females. J. Strength Cond. Res. 29, 1592–1600. https://doi.org/10.1519/jsc.0000000000000790 (2015).
Dor-Haim, H. et al. Improvement in cardiac dysfunction with a novel circuit training method combining simultaneous aerobic-resistance exercises. A randomized trial. PLoS ONE 13, e0188551. https://doi.org/10.1371/journal.pone.0188551 (2018).
Hsu, W. H. et al. Circuit training enhances function in patients undergoing total knee arthroplasty: A retrospective cohort study. J. Orthop. Surg. Res. 12, 156. https://doi.org/10.1186/s13018-017-0654-4 (2017).
Izquierdo-Alventosa, R. et al. Low-intensity physical exercise improves pain catastrophizing and other psychological and physical aspects in women with fibromyalgia: A randomized controlled trial. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph17103634 (2020).
Kennedy, J., Roll, J. M., Schraudner, T., Murphy, S. & McPherson, S. Prevalence of persistent pain in the U.S. adult population: New data from the 2010 national health interview survey. J. Pain 15, 979–984. https://doi.org/10.1016/j.jpain.2014.05.009 (2014).
Wiesenfeld-Hallin, Z. Sex differences in pain perception. Gend. Med. 2, 137–145. https://doi.org/10.1016/s1550-8579(05)80042-7 (2005).
Danielsson, L., Kvarstein, G. & Bergvik, S. Mediators of pain and physical function in female and male patients with chronic pain. J. Pain Res. 13, 1059–1071. https://doi.org/10.2147/jpr.S233501 (2020).
Salaffi, F., Stancati, A., Silvestri, C. A., Ciapetti, A. & Grassi, W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur. J. Pain 8, 283–291. https://doi.org/10.1016/j.ejpain.2003.09.004 (2004).
Scott, W., Wideman, T. H. & Sullivan, M. J. Clinically meaningful scores on pain catastrophizing before and after multidisciplinary rehabilitation: A prospective study of individuals with subacute pain after whiplash injury. Clin. J. Pain 30, 183–190. https://doi.org/10.1097/AJP.0b013e31828eee6c (2014).
Roland, M. & Fairbank, J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine 25, 3115–3124. https://doi.org/10.1097/00007632-200012150-00006 (2000).
Devji, T. et al. Application of minimal important differences in degenerative knee disease outcomes: A systematic review and case study to inform BMJ Rapid Recommendations. BMJ Open 7, e015587. https://doi.org/10.1136/bmjopen-2016-015587 (2017).
Woodlief, T. L. et al. Dose response of exercise training following roux-en-Y gastric bypass surgery: A randomized trial. Obesity 23, 2454–2461 (2015).
MacDonald, C. S. et al. Dose-response effects of exercise on glucose-lowering medications for type 2 diabetes: A secondary analysis of a randomized clinical trial. Mayo Clin. Proc. 95, 488–503 (2020).
Nakamura, M., Nishiwaki, Y., Ushida, T. & Toyama, Y. Prevalence and characteristics of chronic musculoskeletal pain in Japan. J. Orthop. Sci. 16, 424–432. https://doi.org/10.1007/s00776-011-0102-y (2011).
Jaeschke, R., Singer, J. & Guyatt, G. H. Measurement of health status. Ascertaining the minimal clinically important difference. Control. Clin. Trials 10, 407–415. https://doi.org/10.1016/0197-2456(89)90005-6 (1989).
Wendt, M., Cieślik, K., Lewandowski, J. & Waszak, M. Effectiveness of combined general rehabilitation gymnastics and muscle energy techniques in older women with chronic low back pain. Biomed. Res. Int. 2019, 2060987. https://doi.org/10.1155/2019/2060987 (2019).
Uthman, O. A. et al. Exercise for lower limb osteoarthritis: Systematic review incorporating trial sequential analysis and network meta-analysis. BMJ 347, f5555. https://doi.org/10.1136/bmj.f5555 (2013).
Suni, J. H. et al. Effectiveness and cost-effectiveness of neuromuscular exercise and back care counseling in female healthcare workers with recurrent non-specific low back pain: A blinded four-arm randomized controlled trial. BMC Public Health 18, 1376. https://doi.org/10.1186/s12889-018-6293-9 (2018).
Ylinen, J. et al. Active neck muscle training in the treatment of chronic neck pain in women: A randomized controlled trial. JAMA 289, 2509–2516. https://doi.org/10.1001/jama.289.19.2509 (2003).
Dunn, W. R. et al. Symptoms of pain do not correlate with rotator cuff tear severity: A cross-sectional study of 393 patients with a symptomatic atraumatic full-thickness rotator cuff tear. J. Bone Joint Surg. Am. 96, 793–800. https://doi.org/10.2106/jbjs.L.01304 (2014).
Garber, C. E. et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 43, 1334–1359. https://doi.org/10.1249/MSS.0b013e318213fefb (2011).
Larsson, C., Ekvall Hansson, E., Sundquist, K. & Jakobsson, U. Impact of pain characteristics and fear-avoidance beliefs on physical activity levels among older adults with chronic pain: A population-based, longitudinal study. BMC Geriatr. 16, 50. https://doi.org/10.1186/s12877-016-0224-3 (2016).
França, F. R., Burke, T. N., Hanada, E. S. & Marques, A. P. Segmental stabilization and muscular strengthening in chronic low back pain: A comparative study. Clinics 65, 1013–1017. https://doi.org/10.1590/s1807-59322010001000015 (2010).
Kanas, M. et al. Home-based exercise therapy for treating non-specific chronic low back pain. Rev. Assoc. Med. Bras. 1992(64), 824–831. https://doi.org/10.1590/1806-9282.64.09.824 (2018).
Verbrugghe, J. et al. High intensity training to treat chronic nonspecific low back pain: Effectiveness of various exercise modes. J. Clin. Med. https://doi.org/10.3390/jcm9082401 (2020).
Sciamanna, C. N. et al. Feasibility and impact of a 1-minute daily functional exercise regimen prescribed to older adults by their primary care physician. Prev. Med. Rep. 21, 101307. https://doi.org/10.1016/j.pmedr.2020.101307 (2021).
Paton, C. D. & Hopkins, W. G. Combining explosive and high-resistance training improves performance in competitive cyclists. J. Strength Cond. Res. 19, 826–830. https://doi.org/10.1519/r-16334.1 (2005).
Nordgren, B. et al. An outsourced health-enhancing physical activity programme for people with rheumatoid arthritis: Exploration of adherence and response. Rheumatology 54, 1065–1073. https://doi.org/10.1093/rheumatology/keu444 (2015).
Kanamori, S. et al. Frequency and pattern of exercise and depression after two years in older Japanese adults: The JAGES longitudinal study. Sci. Rep. 8, 11224. https://doi.org/10.1038/s41598-018-29053-x (2018).
Gerdle, B., Ghafouri, B., Ernberg, M. & Larsson, B. Chronic musculoskeletal pain: Review of mechanisms and biochemical biomarkers as assessed by the microdialysis technique. J. Pain Res. 7, 313–326. https://doi.org/10.2147/JPR.S59144 (2014).
Ikemoto, T., Miki, K., Matsubara, T. & Wakao, N. Psychological treatment strategy for chronic low back pain. Spine Surg. Relat. Res. 3, 199–206. https://doi.org/10.22603/ssrr.2018-0050 (2019).
Quartana, P. J., Campbell, C. M. & Edwards, R. R. Pain catastrophizing: A critical review. Expert Rev. Neurother. 9, 745–758. https://doi.org/10.1586/ern.09.34 (2009).
Sullivan, M. J. et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin. J. Pain 17, 52–64. https://doi.org/10.1097/00002508-200103000-00008 (2001).
Tracey, I. & Bushnell, M. C. How neuroimaging studies have challenged us to rethink: Is chronic pain a disease?. J. Pain 10, 1113–1120. https://doi.org/10.1016/j.jpain.2009.09.001 (2009).
McMurray, R. G., Harrell, J. S. & Griggs, T. R. A comparison of two fitness programs to reduce the risk of coronary heart disease in public safety officers. J. Occup. Med. 32, 616–620. https://doi.org/10.1097/00043764-199007000-00012 (1990).
Hill, J. C., Lewis, M., Sim, J., Hay, E. M. & Dziedzic, K. Predictors of poor outcome in patients with neck pain treated by physical therapy. Clin. J. Pain 23, 683–690. https://doi.org/10.1097/AJP.0b013e3181468e67 (2007).
Vincent, H. K., George, S. Z., Seay, A. N., Vincent, K. R. & Hurley, R. W. Resistance exercise, disability, and pain catastrophizing in obese adults with back pain. Med. Sci. Sports Exerc. 46, 1693–1701. https://doi.org/10.1249/mss.0000000000000294 (2014).
Brummett, C. M. et al. Preliminary validation of the Michigan Body Map. Pain 157, 1205–1212. https://doi.org/10.1097/j.pain.0000000000000506 (2016).
Lichtman, A. H. et al. Results of a double-blind, randomized, placebo-controlled study of nabiximols oromucosal spray as an adjunctive therapy in advanced cancer patients with chronic uncontrolled pain. J. Pain Symptom Manag. 55, 179-188.e171. https://doi.org/10.1016/j.jpainsymman.2017.09.001 (2018).
Yiangou, A. et al. Therapeutic lumbar puncture for headache in idiopathic intracranial hypertension: Minimal gain, is it worth the pain?. Cephalalgia 39, 245–253. https://doi.org/10.1177/0333102418782192 (2019).
Jensen, M. P., Turner, J. A., Romano, J. M. & Fisher, L. D. Comparative reliability and validity of chronic pain intensity measures. Pain 83, 157–162. https://doi.org/10.1016/s0304-3959(99)00101-3 (1999).
Sullivan, M. J. L., Bishop, S. R. & Pivik, J. The Pain Catastrophizing Scale: Development and validation. Psychol. Assess. 7, 524–532. https://doi.org/10.1037/1040-3590.7.4.524 (1995).
Pielech, M. et al. Pain catastrophizing in children with chronic pain and their parents: Proposed clinical reference points and reexamination of the Pain Catastrophizing Scale measure. Pain 155, 2360–2367. https://doi.org/10.1016/j.pain.2014.08.035 (2014).
Roland, M. & Morris, R. A study of the natural history of back pain. Part I: Development of a reliable and sensitive measure of disability in low-back pain. Spine 8, 141–144. https://doi.org/10.1097/00007632-198303000-00004 (1983).
Smeets, R., Köke, A., Lin, C. W., Ferreira, M. & Demoulin, C. Measures of function in low back pain/disorders: Low Back Pain Rating Scale (LBPRS), Oswestry Disability Index (ODI), Progressive Isoinertial Lifting Evaluation (PILE), Quebec Back Pain Disability Scale (QBPDS), and Roland-Morris Disability Questionnaire (RDQ). Arthritis Care Res. 63(Suppl 11), S158-173. https://doi.org/10.1002/acr.20542 (2011).
Maruyama, K., Kishimoto, J., Hara, M. & Mikasa, M. A characteristic and the direction for uses of self-assessment tool for the shoulder “Shoulder 36 version 1.3”. Nihon Seikeigekagakkai Zasshi J. Jpn. Orthop. Assoc. 87, 249e57 (2013) ((in Japanese)).
Amako, M., Tsuda, Y. & Chiba, K. Comparison of reliability, validity and responsiveness of the Japanese Orthopaedic Association Shoulder 36 Ver. 1.3 among different diagnoses of shoulder lesions. J. Orthop. Sci. https://doi.org/10.1016/j.jos.2020.03.018 (2020).
Kawakami, J. et al. Usefulness of Shoulder36 in rotator cuff tears: Comparison with Simple Shoulder Test. J. Orthop. Surg. 27, 2309499018819060. https://doi.org/10.1177/2309499018819060 (2019).
Roos, E. M., Roos, H. P., Lohmander, L. S., Ekdahl, C. & Beynnon, B. D. Knee Injury and Osteoarthritis Outcome Score (KOOS)–development of a self-administered outcome measure. J. Orthop. Sports Phys. Ther. 28, 88–96. https://doi.org/10.2519/jospt.1998.28.2.88 (1998).
Dennett, R. et al. Adherence and drop-out in randomized controlled trials of exercise interventions in people with multiple sclerosis: A systematic review and meta-analyses. Mult. Scler. Relat. Disord. 43, 102169. https://doi.org/10.1016/j.msard.2020.102169 (2020).
Hanley, J. A. & McNeil, B. J. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148, 839–843. https://doi.org/10.1148/radiology.148.3.6878708 (1983).
Acknowledgements
The authors would like to thank Junya Sado for the study design and development. We would also like to thank the participants who volunteered for this study.
Author information
Authors and Affiliations
Contributions
T.K., N.S., T.H., H.S., and K.N. designed the study. S.U., T.K., H.E., T.S., and S.S. analyzed the data. S.S., S.U., T.K., and K.N. wrote the manuscript. S.S. and S.U. contributed equally to this work.
Corresponding author
Ethics declarations
Competing interests
This research was carried out as a collaborative project among Osaka University, Curves Japan Co., Ltd. and Eli Lilly Japan K.K., and was financially supported by Eli Lilly Japan K.K.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sato, S., Ukimoto, S., Kanamoto, T. et al. Chronic musculoskeletal pain, catastrophizing, and physical function in adult women were improved after 3-month aerobic-resistance circuit training. Sci Rep 11, 14939 (2021). https://doi.org/10.1038/s41598-021-91731-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-91731-0
- Springer Nature Limited
This article is cited by
-
Novel Therapies for Centralized Pain: a Brief Review
Current Pain and Headache Reports (2022)