Abstract
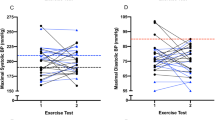
It has been established that blacks have higher overall incidence and prevalence of hypertension compared to their white counterparts. However, the maximum blood pressure (BP) response of blacks to exercise has not been characterized. A total of 5996 apparently healthy men from the Fitness Registry and Importance of Exercise: A National Database (FRIEND) who underwent maximum cardiopulmonary exercise tests on a cycle ergometer were included in this analysis. Of these participants, 1245 (21%) self-identified as black while the remaining 4751 (79%) identified as white. All subjects had a respiratory exchange ratio (RER) of ≥1.0 and had no reports of cardiovascular or pulmonary disease. Systolic BP (BP) response to exercise was indexed according to increase in workload (SBP/MET-slope). Both racial groups were subdivided into age groups by decade. Black men had higher peak SBP and higher SBP/MET-slopes compared to white men across all age groups (p < 0.001). Resting SBP was not different between blacks and whites except within the 18–29-year age group. The differences in peak SBP and SBP/MET-slope between age and race groups indicate that black men have an exaggerated BP response to exercise irrespective of resting BP values. Further investigation is warranted to determine the underlying mechanisms responsible and clinical implications for this exaggerated BP response to exercise.


Similar content being viewed by others
References
Guazzi M, Arena R, Halle M, Piepoli MF, Myers J, Lavie CJ. 2016 focused update: clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2016;133:e694–711.
Guazzi M, Adams V, Conraads V, Halle M, Mezzani A, Vanhees L, et al. EACPR/AHA Scientific Statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2012;126:2261–74. http://circ.ahajournals.org/content/126/18/2261%5Cnhttp://circ.ahajournals.org//subscriptions/%5Cnhttp://circ.ahajournals.org/.
Kokkinos P, Myers J. Exercise and physical activity: clinical outcomes and applications. Circulation. 2010;122:1637–48.
Schultz MG, La Gerche A, Sharman JE. Blood pressure response to exercise and cardiovascular disease. Curr Hypertens Rep. 2017;19:89. http://link.springer.com/10.1007/s11906-017-0787-1.
Currie KD, Floras JS, La Gerche A, Goodman JM. Exercise blood pressure guidelines: time to re-evaluate what is normal and exaggerated? Sport Med. 2018;48:1763–71. http://link.springer.com/10.1007/s40279-018-0900-x.
Hedman K, Cauwenberghs N, Christle JW, Kuznetsova T, Haddad F, Myers J. Workload-indexed blood pressure response is superior to peak systolic blood pressure in predicting all-cause mortality. Eur J Prev Cardiol [Internet]. 2019 Sep 30;2047487319877268. https://doi.org/10.1177/2047487319877268.
Jae SY, Kurl S, Kunutsor SK, Franklin BA, Laukkanen JA. Relation of maximal systolic blood pressure during exercise testing to the risk of sudden cardiac death in men with and without cardiovascular disease. Eur J Prev Cardiol. 2019;2047487319880031. https://pubmed.ncbi.nlm.nih.gov/31604381/. [Epub ahead of print].
Sabbahi A, Arena R, Kaminsky LA, Myers J, Phillips SA. Peak blood pressure responses during maximum cardiopulmonary exercise testing. Hypertension. 2018;71:229–36. http://hyper.ahajournals.org/lookup/doi/10.1161/HYPERTENSIONAHA.117.10116.
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–492. 20 http://www.ncbi.nlm.nih.gov/pubmed/29386200.
Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136:e393–423.
Thomas SJ, Booth JN, Dai C, Li X, Allen N, Calhoun D, et al. Cumulative incidence of hypertension by 55 years of age in blacks and whites: the CARDIA Study. J Am Heart Assoc. 2018;7:e007988. http://www.ncbi.nlm.nih.gov/pubmed/29997132.
Keller K, Stelzer K, Ostad MA, Post F. Impact of exaggerated blood pressure response in normotensive individuals on future hypertension and prognosis: systematic review according to PRISMA guideline. Adv Med Sci. 2017;62:317–29. http://ac.els-cdn.com.proxy.cc.uic.edu/S1896112617300159/1-s2.0-S1896112617300159-main.pdf?_tid=21dd363e-3c44-11e7-a5f5-00000aab0f27&acdnat=1495165078_fe250c8926dd4ccbe225bf9c00feadc5.
Kaminsky LA, Arena R, Beckie TM, Brubaker PH, Church TS, Forman DE, et al. The importance of cardiorespiratory fitness in the United States: the need for a national registry: a policy statement from the american heart association. Circulation. 2013;127:652–62.
Kaminsky LA, Arena R, Myers J. Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing data from the fitness registry and the importance of exercise national database. Mayo Clin Proc. 2015;90:1515–23. https://doi.org/10.1016/j.mayocp.2015.07.026.
Kaminsky LA, Imboden MT, Arena R, Myers J. Reference Standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing using cycle ergometry: Data From the Fitness Registry and the Importance of Exercise National Database (FRIEND) Registry. Mayo Clin Proc. 2017;92:228–33.
Myers J, Arena R, Franklin B, Pina I, Kraus WE, McInnis K, et al. Recommendations for clinical exercise laboratories: a scientific statement from the american heart association. Circulation. 2009;119:3144–61.
Myers J, Forman DE, Balady GJ, Franklin BA, Nelson-Worel J, Martin B-JJ, et al. Supervision of exercise testing by nonphysicians: a scientific statement from the American Heart Association. Circulation. 2014;130:1014–27.
Arena R, Myers J, Kaminsky LA. Revisiting age-predicted maximal heart rate: can it be used as a valid measure of effort? Am Heart J. 2016;173:49–56. https://doi.org/10.1016/j.ahj.2015.12.006.
Sharman JE, LaGerche A. Exercise blood pressure: clinical relevance and correct measurement. J Hum Hypertens. 2015;29:351–8. http://www.nature.com/articles/jhh201484.
Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, et al. Exercise standards for testing and training: a scientific statement from the American heart association. Circulation. 2013;128:873–934.
Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366:321–9. http://www.nejm.org/doi/pdf/10.1056/NEJMoa1012848.
Abate NI, Mansour YH, Tuncel M, Arbique D, Chavoshan B, Kizilbash A, et al. Overweight and sympathetic overactivity in black Americans. Hypertension. 2001;38:379–83. http://hyper.ahajournals.org/lookup/doi/10.1161/01.HYP.38.3.379.
Bombelli M, Facchetti R, Sega R, Carugo S, Fodri D, Brambilla G, et al. Impact of body mass index and waist circumference on the long-term risk of diabetes mellitus, hypertension, and cardiac organ damage. Hypertension. 2011;58:1029–35.
Feairheller DL, Park J-Y, Sturgeon KM, Williamson ST, Diaz KM, Veerabhadrappa P, et al. Racial differences in oxidative stress and inflammation: in vitro and in vivo. Clin Transl Sci. 2011;4:32–7.
Kim K, Hurr C, Patik JC, Matthew Brothers R. Attenuated cutaneous microvascular function in healthy young African Americans: role of intradermal l-arginine supplementation. Microvasc Res. 2018;118:1–6. https://www-sciencedirect-com.proxy.cc.uic.edu/science/article/pii/S0026286217302339.
Melikian N, Wheatcroft SB, Ogah OS, Murphy C, Chowienczyk PJ, Wierzbicki AS, et al. Asymmetric Dimethylarginine and reduced nitric oxide bioavailability in young black African men. Hypertension. 2007;49:873–7. http://hyper.ahajournals.org/cgi/doi/10.1161/01.HYP.0000258405.25330.80.
Kalinowski L, Dobrucki IT, Malinski T. Race-specific differences in endothelial function predisposition of African Americans to vascular diseases. Circulation. 2004;109:2511–7. http://www.circulationaha.org.
Ozkor MA, Rahman AM, Murrow JR, Kavtaradze N, Lin J, Manatunga A, et al. Differences in vascular nitric oxide and endothelium-derived hyperpolarizing factor bioavailability in blacks and whites. Arterioscler Thromb Vasc Biol. 2014;34:1320–7. http://atvb.ahajournals.org/lookup/suppl/doi:10.1161/ATVBAHA.113.303136/-/DC1.
Vongpatanasin W, Wang Z, Arbique D, Arbique G, Adams‐Huet B, Mitchell JH, et al. Functional sympatholysis is impaired in hypertensive humans. J Physiol. 2011;589:1209–20. https://physoc-onlinelibrary-wiley-com.proxy.cc.uic.edu/doi/abs/10.1113/jphysiol.2010.203026.
Heffernan KS, Jae SY, Wilund KR, Woods JA, Fernhall B. Racial differences in central blood pressure and vascular function in young men. Am J Physiol Circ Physiol. 2008;295:H2380–7. http://www.physiology.org/doi/10.1152/ajpheart.00902.2008.
Bond V, Stephens Q, Adams RG, Vaccaro P, Demeersman R, Williams D, et al. Aerobic exercise attenuates an exaggerated exercise blood pressure response in normotensive young adult African-American men. Blood Press. 2002;11:229–34.
Riebe D, Ehrman JK, Liguori G, Magal M, (eds) ACSM’s guidelines for exercise testing and prescription. 10th ed. Philadelphia, PA: Wolters Kluwer Health; 2018.
Yan H, Ranadive SM, Heffernan KS, Lane AD, Kappus RM, Cook MD, et al. Hemodynamic and arterial stiffness differences between African-Americans and Caucasians after maximal exercise. Am J Physiol Circ Physiol. 2014;306:H60–8. http://www.physiology.org/doi/10.1152/ajpheart.00710.2013.
Barbosa TC, Kaur J, Stephens BY, Akins JD, Keller DM, Brothers RM, et al. Attenuated forearm vascular conductance responses to rhythmic handgrip in young African-American compared with Caucasian-American men. Am J Physiol Circ Physiol. 2018;315:H1316–21. https://www.physiology.org/doi/10.1152/ajpheart.00387.2018.
Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, et al. Clinician’s guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:191–225. http://circ.ahajournals.org/cgi/content/long/122/2/191.
Chant B, Bakali M, Hinton T, Burchell AE, Nightingale AK, Paton JFR, et al. Antihypertensive treatment fails to control blood pressure during exercise. Hypertension. 2018;72:102–9.
Schultz MG, Sharman JE. Exercise hypertension. Pulse. 2013;1:161–76. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4315351&tool=pmcentrez&rendertype=abstract.
Weiss SA, Blumenthal RS, Sharrett AR, Redberg RF, Mora S. Exercise blood pressure and future cardiovascular death in asymptomatic individuals. Circulation.2010;121:2109–16. http://circ.ahajournals.org.
Daida H, Allison TG, Squires RW, Miller TD, Gau GT. Peak exercise blood pressure stratified by age and gender in apparently healthy subjects. Mayo Clin Proc. 1996;71:445–52.
Acknowledgements
FRIEND Consortium Contributors are as follows: Ball State University (Leonard Kaminsky, Matthew Harber), METTEST (Sundeep Chaudhry), Massachusetts General Hospital (Gregory Lewis). This study was supported in part by an NIH training grant to Ahmad Sabbahi (T32-HL-139439).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sabbahi, A., Arena, R., Kaminsky, L.A. et al. Characterization of the blood pressure response during cycle ergometer cardiopulmonary exercise testing in black and white men. J Hum Hypertens 35, 685–695 (2021). https://doi.org/10.1038/s41371-020-00411-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-00411-5
- Springer Nature Limited