Abstract
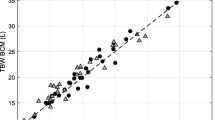
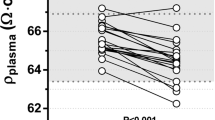
Measuring intercompartmental, blood and urinarybiochemical parameters during acute bed rest(ABR) and rigorous bed rest (RBR) the aim ofthis work was to disclose if ABR or RBR couldinfluence significantly more and significantlyfaster the body hydration level in normal subjects.Studies conducted during pre-bed rest (BR)period of 3-days and during 7-days period of ABRand RBR. Thirty normal male individuals24.6 ± 5.7 years of age were chosen assubjects. They were divided into three groups:unrestricted active control subjects (UACS),acute bed rested subjects (ABRS) and rigorousbed rested subjects (RBRS). Acute bed restedsubjects confined abruptly to RBR, while theydid not have any prior knowledge of the exactdate and time when they would be subjected toRBR. RBRS were submitted to RBR in apredetermined date and time known to them rightfrom the start of the study. UACS were notsubjected to any form of BR.Fluid loss, urinary and plasma sodium (Na+) andpotassium (K+), plasma osmolality, whole bloodhematocrit (Hct) and hemoglobin (Hb), and totalplasma protein level increased significantly(p < 0.05), while urinary osmolality,extracellular volume (ECV), plasma volume (PV),red cell volume (RCV), blood volume (BV),interstitial volume (IV) and fluid consumptiondecreased significantly (p < 0.05) in ABRS andRBRS compared with their pre-BR values andtheir control (UACS). However, the measuredvariables changed significantly (p < 0.05) moreand significantly faster in ABRS than RBRS.Conversely, whole blood Hct and Hb levels,fluid consumption and fluid loss, urinary andplasma osmolality, urinary and plasmaelectrolytes, plasma protein, ECV, PV, RCV, BVand IV levels were not change in UACS comparedwith their pre-BR values.Significantly greater and significantly fasterintercompartmental, blood and urinarybiochemical changes were observed in ABRS thanRBRS. Body hydration was affected significantlymore and significantly faster in ABR than RBR. It wasconcluded, the more abruptly normal activity isrestricted the smaller the body hydration inbed rested subject is, and probably in patientswho are abruptly confined to RBR.
Similar content being viewed by others
References
Zorbas YG, Federenko YF, Naexu KA. Fluid-electrolyte excretion and plasma hormonal changes in trained subjects during acute bed rest and chronic hyperhydration. Eurorehab 1995; 2: 107–114.
Zorbas YG, Federenko YF, Yaroshenko YY. Urinary and plasma calcium in endurance trained volunteers during exposure to acute and rigorous bed rest conditions. Biol Trace Element Res 1986; 54: 75–86.
Zorbas YG, Yaroshenko YY, Federenko YF. Serum urate and cholesterol levels in endurance trained volunteers during acute and rigorous bed rest conditions. Panminerva Med 1996; 38: 223–228.
Yaroshenko YY, Zorbas YG, Kuznetsov NK, Kakurin AG, Popov VK. Changes in thyroid hormones and lipids in endurance trained volunteers during acute and rigorous bed rest conditions. Wiener Klinische Wochenschrift 1998; 110: 225–231.
Greenleaf JE, Bernauer EM, Juhos LT, Young HL, Morse JT, Staley RW. Effects of exercise on fluid exchange and body composition in man during 14-day bed rest. J Appl Physiol: Respirat Environm Exercise Physiol 1977; 43: 126–132.
Greenleaf JE, Bernauer EM, Young HL, Morse JT, Staley RW, Juhos LT, Van Beaumont W. Fluid and electrolyte shifts during bed rest with isometric and isotonic exercise. J Appl Physiol: Respirat Environm Exercise Physiol 1977; 42: 59–66.
Balke B, Grillo CP, Konecci WB, Luft UC. Work capacity after blood donation. J Appl Physiol 1954; 7: 231–238.
Epstein M. Renal effects of head-out water immersion in man: implications for an understanding of volume homeostasis. Physiol Rev 1978; 58: 529–581.
Gauer OH, Henry JP. Neurohormonal control of plasma volume. Inter Rev Physiol Cardiovasc Physiol II 1976; 9: 145–190.
Epstein M, Saruta T. Effect of water immersion on reninaldosterone and renal handling in normal man. J Appl Physiol 1971; 31: 368–374.
Epstein M, Bricker NS, Bourgoignie JJ. Presence of a natriuretic factor in urine of normal men undergoing water immersion. Kidney Inter 1978; 13: 152–158.
Spears CP, Hyatt KH, Vogel JM, Langfitt SB. Unified method for a serial study of body fluid compartments. Aerospace Med 1974; 45: 274–278.
Grigor'yev AI. Regulation of fluid-electrolyte metabolism and renal functions in man during kosmic flights, PhD Thesis, “Interkosmos” Council, Academy of Sciences USSR and Directorate of Kosmic Biology and Medicine, Ministry of Health USSR, Moscow, Russia, 1980.
Kakurin LI, Arzamazov GS, Grigor'yev AI. Kaliuretic renal function in man as related to different degrees of exercise during bed rest. Kosmicheskaya Biol 1978; 12: 13–17.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Zorbas, Y.G., Yarullin, V.L., Denogratov, S.D. et al. Fluid volume measurements in normal subjects to disclose body hydration during acute bed rest. Int Urol Nephrol 35, 457–465 (2003). https://doi.org/10.1023/B:UROL.0000025636.41034.83
Issue Date:
DOI: https://doi.org/10.1023/B:UROL.0000025636.41034.83