Abstract
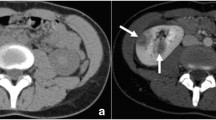
An experimental study has been conducted toevaluate the effects of increasedintra-abdominal pressure (IAP) on the excretionfunction from renal pelvis into the ureter.Methods: Sixteen adult male New Zealandrabbits were randomly allocated in two groupsafter obtaining basal scintigraphies. Group Iconsisted of 8 rabbits which were subjected toan increased IAP for ten day period. In GroupII an other 8 rabbits were subjected to anincreased IAP for 60 day period. At the end ofthe periods of increased IAP the post-pressurescintigraphic evaluations of both groups werecarried out. Time to maximum activity(Tmax), T1/2 and T2/3 values ofthe radiopharmaceutical in the kidneys and downslope parameters (DS1/2, DS2/3)were calculated from the renogram curves ofboth right and left kidneys. Comparison ofbasal and post-pressure scintigrapies and themean difference of the renogram parametersbetween groups were performed.Results: All basal scintigraphies werenormal. Post-pressure scintigraphies revealedan obvious delay in the excretion phase in bothgroups. Both kidneys of a rabbit in group Irevealed a non-obstructive pattern throughresponding well to administration of diuretic.Furthermore both kidneys of a rabbit from groupII have revealed an obstructive pattern.T1/2 and T2/3 values weresignificantly elevated and mean DS1/2,DS2/3 were significantly decreased inpost-pressure scintigraphies of the both groupswithout revealing a statistically significantdifference between groups I and II. The meandifference of Tmax was significantlyincreased in group II.Conclusion: The increases in IAP, throughthe compressive effect upon ureters togetherwith a concomitant increase in intravesicalpressure, may impair the passage of urine fromrenal pelvis into ureter. The impaired passagemay play a role in the development of hydronephrosis which may either reveal anonobstructive and/or obstructive pattern.
Similar content being viewed by others
References
Damask AC. Medical Physics. New York, NY: Academical Press, 1978.
Boix-Ochoa J. Address of honoured guest: the physiologic approach to the management of gastric esophageal reflux. J Pediatr Surg 1986; 21:1032-1033.
Schein M, Wittmann DH, Aprahamian CC, Condon RE. The abdominal compartment syndrome: The physiological and clinical consequences of elevated intraabdominal pressures. J Am Coll Surg 1995; 180: 745-753.
Dmochowski R. Cystometry. Urol Clin North Am 1996; 23: 243-252.
Norris JP, Staskin DR. History physical examination and classification of neurogenic voiding dysfunction. Urol Clin North Am 1996; 23: 337-343.
McGuire EJ, Savastano JA, Morrissey S. Bladder and ureteral pressure relationships in normal human primates. J Urol 1983; 130: 374-376.
Nicolini U, Fisk M, Talbert DG et al. Intrauterine manometry: technique and application to fetal pathology. Prenat Diagn 1989; 9: 243-254.
Tanyel FC. Urinary tract anomalies and dysfunctional voiding: a spectrum dictated by the influence of amniotic pressure upon fetal urodynamics. Medic Hypoth 2000; 54: 140-145.
Housley HT, Harrison MR. Fetal urinary tract abnormalities. Natural history pathophysiology and treatment. Urol Clin North Am 1998; 25: 63-74.
King LR. Hydronephrosis. When is obstruction not obstruction? Urol Clin North Am 1995; 22: 31-42.
Homsy YL, Mehta PH, Hout D, Danais S. Intermittent hydronephrosis: a diagnostic challenge. J Urol 1988; 140: 1222-1226.
Karnak I, Bingol-Kologlu M, Karaagaoglu E et al. Renal pelvic pressure responds with augmented increases to increments in intraabdominal pressure. J Pediatr Surg 2001; 36: 901-904.
Ready PP, Mandell J. Prenatal diagnosis. Therapeutic implications. Urol Clin North Am 1998; 25: 171-186.
Brown SCW. Nuclear medicine in clinical diagnosis and treatment of obstructive uropathy. In: Murray IPC, Ell PJ eds. Nuclear Medicine in Clinical Diagnosis and Treatment, Edinburgh: Churchill Livingstone, 1994: 271-286.
Jones DA, Lupton EW, George NJR. Effect of bladder filling on upper tract dynamics in man. Br J Urol 1990; 65: 492-496.
Zimskind PD, Davis DM, Decaestecker JE. Effects of bladder filling on ureteral filling. J Urol 1969; 102: 693-696.
Koff SA. Pressure volume relationships in human hydronephrosis. Urology 1985; 25: 256-258.
Kimble RM, Harding J, Kolbe A. Additional congenital anomalies occur in babies with a gut atresia or stenosis: When to investigate and which investigation. Pediatr Surg Int 1997; 12: 565.
Lortat-Jacob S, Nihoul-Fekete C, Pellerin D. Urogenital abnormalities associated with anorectal malformations. Acta Urol Belg 1990; 58: 163.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bingol-Kologlu, M., Ergün, E.L., Caner, B. et al. Increased intra-abdominal pressure results in both obstructive and nonobstructive types of impairments of renal pelvic excretion. Int Urol Nephrol 35, 127–133 (2003). https://doi.org/10.1023/B:UROL.0000020298.04291.13
Issue Date:
DOI: https://doi.org/10.1023/B:UROL.0000020298.04291.13