Abstract
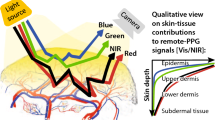
Objective. Recent studies have renewed interest in reflectance pulse oximetry, specifically for monitoring the patient's forehead. Blood circulation on the forehead immediately above the eyebrow is fed by arteries that branch from the internal carotid artery and lack the vasoconstrictor response present in more peripheral regions. Some investigators question, however, the reliability of monitoring SpO2 on the forehead due to prior reported inaccurate readings with reflectance sensors. The present study evaluates pulse oximetry accuracy when reflectance sensors are placed over potentially pulsing or moving larger arterial vessels, or over more homogeneous microvasculature devoid of larger subcutaneous vessels. Methods. Ten healthy adult volunteers were fitted with reflectance pulse oximetry sensors and exposed to a controlled desaturation to 70%. Sensors were placed immediately above the left and right eyebrows as well as over the temple. Additionally, numerical modeling was used to simulate light signals and photon migration through a homogeneous tissue bed with an added static or dynamic artery. Results. Sensors placed above the eyebrows tracked one another with significantly better accuracy than when comparing temple with the brow placement (RMS of the Differences = 1.12% vs. 4.24%, respectively). Photon migration simulations indicate that the detected light bypasses the interior of larger vessels, while vessel presence affects the red and IR light pulse amplitudes independent of SaO2. Conclusions. Placement of reflectance pulse oximetry sensors directly over larger cardio-synchronously pulsing or moving vasculature can significantly degrade SpO2 reading accuracy. Reflectance sensors placed low on the forehead directly over the eyebrow and slightly lateral to the iris appear to avoid such vasculature and provide consistent and accurate estimates of SaO2.
Similar content being viewed by others
REFERENCES
American Society of Anesthesiologists. Standards for Basic Anesthetic Monitoring, Approved October 1986, last amended October 1998.
Hertzmann AB, Roth LW. The absence of vasoconstrictor reflexes in the forehead circulation. Effects of cold. Am J Physiol 1942; 136: 692–697.
Pälve H. Reflection and transmission pulse oximetry during compromised peripheral perfusion. J Clin Monit 1992; 8: 12–15.
Bebout DE, Mannheimer PD. Effects of cold-induced periph-eral vasoconstriction on pulse amplitude at various pulse oxime-ter sensor sites. Anesthesiology 2002; 96: A558.
Severinghaus JW, Naifeh KH. Accuracy of response of six pulse oximeters to profound hypoxia. Anesthesiology 1987; 67: 551–558.
Severinghaus JW, Spellman MJ, Jr. Pulse oximeter failure thresh-olds in hypotension and vasoconstriction. Anesthesiology 1990; 73(3): 532–537.
Reynolds LM, Nicolson SC, Steven JM, et al. Influence of sensor site location on pulse oximetry kinetics in children. Anesth Analg 1993; 76: 751–754.
Bebout DE, Mannheimer PD, Chin RP, et al.Site-dependent time delays in pulse oximetry monitoring. Am J Respir Crit Care Med 2001; 163(5): A–134.
Dassel AC, Graaff R, Aardema M, et al.Effect of location of the sensor on reflectance pulse oximetry. Br J Obstet Gynaecol 1997; 104(8): 910–916.
Nijland R, Jongsma HW, van den Berg PP, et al.The effect of pulsating arteries on reflectance pulse oximetry: Measurements in adults and neonates. J Clin Monit 1995; 11: 118–122.
Mannheimer PD, Fein ME, Casciani JR. Physio-optical con-siderations in the design of fetal pulse oximetry sensors. Eur J Obstet Gynaecol Reprod Biol. 1997; 72(Suppl 1): S9–S19.
Mannheimer PD. Design and validation of pulse oximetry for low saturation. Anesth Analg 2002; 94(Suppl 1): S21–S25.
Bonner R, Nossal R, Havlin S, et al.Model for photon mi-gration in turbid biological media. J Opt Soc Am A 1987; 4: 423–432.
Zilstra W, Buursma A, Meeuwesen-van der Roest W. Ab-sorption spectra of human fetal and adult oxyhemoglobin, de-oxyhemoglobin, carboxyhemoglobin, and methemoglobin. Clin Chem 1991; 37: 1633–1638.
Schmitt J. Simple photon diffusion analysis of the effects of mul-tiple scattering on pulse oximetry. IEEE Trans Biom Eng 1991; 38: 1194–1203.
Nellcor MAX-FASTsensor when used with the Nellcor Oxi-Max N-595 monitor. Data provided by Nellcor/Tyco Health-care, Pleasanton CA; FDA 510(k) #K021089.
Mannheimer PD, Casciani JR, Fein ME, Nierlich S. Wavelength selection for low-saturation pulse oximetry. IEEE Trans Biom Eng1997; 44(3): 148–158.
Jorgensen JS, Schmid ER, König V, et al.Limitations of forehead pulse oximetry. J Clin Monit 1995; 11: 253–256.
Frick HF, Kummer AB, Putz RV, eds. Atlas of Human Anatomy, 4th ed Basel, Switzerland: Karger, 1990: 171.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Mannheimer, P.D., O'Neil, M.P. & Konecny, E. The Influence of Larger Subcutaneous Blood Vessels on Pulse Oximetry. J Clin Monit Comput 18, 179–188 (2004). https://doi.org/10.1023/B:JOCM.0000042924.16052.5e
Issue Date:
DOI: https://doi.org/10.1023/B:JOCM.0000042924.16052.5e