Abstract
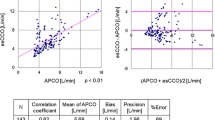
Cardiac output (CO) is a parameter usually requested to assess hemo dynamic status of patient and efficacy of therapy especially in critically ill patients. This paper, in line with other research activities and new market availability, intends to correlate a parameter derived from data already acquired in standard patient monitoring (systemic arterial pressure – Pas) in order to identify CO trends and, more generally, to obtain information on the efficiency of cardiovascular system of the patient in examination. Attention has been focussed on patients undergoing abdominal aneurysm aortic (AAA) surgery with combined anaesthesia (epidural and light general). Awake correlation was found between maximum value of Pas time derivative, max (dPas/dt), and CO measured with thermodilution method on 56 measurements on 10 patients. To evaluate further diagnostic capability of max (dPas/dt), we compare its trend with other parameters but no statistical significant results have been obtained. Therefore the target parameter can be profitably used in the examined patients to monitor CO trend and, in correlation with other parameters, as a sign of efficiency of the cardio circulatory system.
Similar content being viewed by others
REFERENCES
Jellema WT, Wesseling KH, Groeneveld AB, Stoutenbeek CP, Thijs LG, van Lieshout JJ. Continuous cardiac output in septic shock by simulating a model of the aortic input impedance: A comparison with bolus injection thermodilution. Anesthesiology 1999; 90(5): 1317–1328
Ceriana P, Mauelli M, Braschi A, Baiardi P, De Amici D. Noninvasive cardiac output assessment during heart surgery. J Clin Monit Comput 2002; 17(2): 147–149
Berton C, Cholley B. New techniques for cardiac output measurement – oesophageal Doppler, Fick principle using carbon dioxide, and pulse contour analysis. Crit Care 2002; 6(3): 216–221
Connors AF, Speroff T, Dawson NV, Thomas C, Harrell FE, Wagner D, Desbiens N, Goldman L, Wu AW, Califf RM, Fulkerson WJ, Vidaillet H, Broste S, Bellamy P, Lynn J, Knaus WA. The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT investigators. JAMA 1996; 276(11): 889–897
Ramsey SD, Saint S, Sullivan S, Dey L, Kelley K, Bowdle A. Clinical and economic effects of pulmonary artery cathererization in non emenergent coronary artery by pass graft surgery. J Cardio Vasc Anesth 2000; 14(2): 113–118
Darovic GO. Hemodynamic monitoring: Invasive and non invasive clinical applications, 3rd edn. Philadelphia: W.B Saunders Company, 2002
Odenstedt H, Stenqvist O, Lundin S. Clinical evaluation of a partial CO2 rebreathing technique for cardiac output monitoring in critically ill patients. Acta Anaesthesiol Scand 2002; 46(2): 152–159
Clemente F, Antonini M, De Lazzari C, Ferrari G, Mimmo R, Guaragno M, Tosti G. A virtual instrument (VI) for hemodynamic management in ICU and during surgery. JMed EngTechnol 2000; 24(3): 111–116
Clemente F, De Lazzari C, Darowski M, Ferrari G, Mimmo R, Guaragno M, Tosti G. Study of systolic pressure variation (SPV) in presence of mechanical ventilation. Int J Artif Organs 2002; 25(4): 313–320
Caro CG, Pedley TJ, Schroter RC, Seed WA. The mechanics of the circulation, Oxford: Oxford University Press, 1978: 227–228
Braunwald E. Assessment of cardiac function. In Braunwald E, ed. Heart diseases, Philadelphia: W.B. Saunders Company, 1988: 449–470
Brinton TJ, Cotter B, Kailasam MT, Brown DL, Chio SS, O'Connor DT, DeMaria AN. Development and validation of a noninvasive method to determine arterial pressure and vascular compliance. Am J Cardiol 1997; 80(3): 323–330
Kyriazis J, Glotsos J, Bilirakis L, Smirnioudis N. The (dP/dt)max derived from arterial pulse waveforms: Prospective, applications in the haemodialysis setting. Nephrol Dial Transplant 2001; 16(5): 1087–1088
IEC 60601-1 (1988-12), Medical electrical equipment – Part 1: General requirements for safety
IEC 60601-1-1 (2000-12), Medical electrical equipment – Part 1-1: General requirements for safety – Collateral standard: Safety requirements for medical electrical systems
Rolf N, Van Aken H. Phisiology and pathophisiology of thoracic sympathetic blockade. Bailliere's Clinical Anaesthesiology 1999; 13(1): 1–7
Marino PL.The ICU book, 2nd edn. Baltimore: Williams & Wilkins, 1998
Pizov R, Choen M, Weiss Y, Segal E, Cotev S, Perel A. Positive end-expiratory pressure-induced hemodynamic changes are re£ected in the arterial pressure waveform. Crit CareMed 1996; 24: 1381–1387
Author information
Authors and Affiliations
Additional information
CNR
From
Rights and permissions
About this article
Cite this article
Clemente, F., D'Avino, E., Guaragno, M. et al. An on line technique to detect cardiac output variations and cardiovascular performances during abdominal aortic surgery. J Clin Monit Comput 18, 81–87 (2004). https://doi.org/10.1023/B:JOCM.0000032696.16467.3d
Issue Date:
DOI: https://doi.org/10.1023/B:JOCM.0000032696.16467.3d