Abstract
Introduction: Fractionated electrograms and double potentials have been well described within the coronary sinus (CS) in humans. The pattern of circumferential activation in the CS has not been investigated. Furthermore, no data exist on conduction characteristics within the great cardiac vein (GCV) or the middle cardiac vein (MCV).
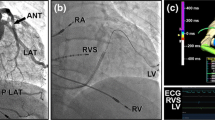
Methods and Results: Twenty patients underwent catheter mapping of the CS, the MCV, and the GCV. Anatomical areas were verified by cannulation of the left superior pulmonary vein. The pattern of circumferential muscle activation within the proximal CS was also studied with a circular mapping catheter (Lasso 12 mm). At conventional mapping during sinus rhythm and high right atrial pacing, discrete double potentials or fractionated electrograms were recorded during left, right atrial and CS pacing at the CS ostium, mid-CS, and distal CS-ligament of Marshall area, in 2 (10%), 1 (5%), and 9 (45%) patients, respectively, whereas no patient displayed such signals in the MCV or GCV (p < 0.001). Proximal CS mapping with the Lasso was accomplished in 10 patients, 7 of whom had no evidence of multicomponent potentials in the CS at conventional mapping. Specific CS potentials dissociated from the atrial electrograms were recorded in all patiens with the use of circumferential mapping. The perimetric distribution of electrograms within the CS suggested an oblique course of conduction across the CS musculature.
Conclusion: Potentials representing activation of the CS musculature, with an oblique course of conduction across the CS, can be recorded in human CS but not in the GCV or MCV. This is compatible with anatomical observations of sinus venosus musculature covering the CS but not other cardiac veins, and supports the rationale for the role of CS musculature in the generation of atrial arrhythmias.
Similar content being viewed by others
References
Hwang C, Wu TJ, Doshi RN, Peter CT, Chen PS. Vein of Marshall cannulation for the analysis of electrical activity in patients with focal AF. Circulation 2000;101: 1503-1505.
Katritsis D, Ioannidis J, Anagnostopoulos CE, Sarris G, Giazitzoglou E, Korovesis S, Camm AJ. Catheter ablation of extracardiac and intracardiac components of ligament of Marshall tissue: A novel approach for the treatment of atrial fibrillation. J Cardiovasc Electrophysiol 2001;12:750-758.
Kasai A, Anselme F, Saoudi N. Myocardial connections between left atrial myocardium and coronary sinus musculature in man. J Cardiovasc Electrophysiol 2001;12:981-985.
Katritsis D, Ioannidis JPA, Giazitzoglou E, Korovesis S, Anagnostopoulos CE, Camm AJ. Conduction delay within the coronary sinus in humans: Implications for atrial arrhythmias. J Cardiovasc Electrophysiol 2002;13:859-862.
Antz M, Otomo K, Arruda M, Scherlag BJ, Pitha J, Tondo C, Lazzara R, Jackman WM. Electrical conduction between the right atrium and the left atrium via the musculature of the coronary sinus. Circulation 1998;98:1790-1795.
Chauvin M, Shah DC, Haissaguerre M, Marcellin L, Brechenmacher C. The anatomic basis of connections between the coronary sinus musculature and the left atrium in humans. Circulation 2000;101:647-652.
Gerlis LM, Davies MJ, Boyle R, Williams G, Scott H. Preexcitation due to accessory siniventricular connexions associated with coronary sinus aneurysms. A report of two cases. Br Heart J 1985;53:314-322.
von Ludinghausen M, Ohmachi N, Boot C. Myocardial coverage of the coronary sinus and related veins. Clin Anat 1992;5:1-15.
Wilcox BR, Anderson RH. Surgical Anatomy of the Heart. 2nd edn. London: Gower Medical Publishers; 1982:220.
von Ludinghausen M, Ohmachi N, Besch S, Mettenleiter A. Atrial veins of the human heart. Clin Anat 1995;8:169-189.
Zipes DP, Knope RF. Electrical properties of the thoracic veins. Am J Cardiol 1972;29:372-376.
Spach MS, Barr RC, Jewett PH. Spread of excitation from the atrium into thoracic veins in human beings and dogs. Am J Cardiol 1972;30:844-854.
Haissaguerre M, Shah DC, Jais P, Hocini M, Yamane T, Deisenhofer I, Chauvin M, Garrigue S, Clementy J. Electrophysiological breakthroughs from the left atrium to the pulmonary veins. Circulation 2000;102:2463-2465.
Katritsis D, Ioannidis JPA, Giazitzoglou E, Korovesis S, Anagnostopoulos CE, Camm AJ. Epicardial origin of atrial ectopy apparently originating from the left pulmonary veins: Implications for the treatment of paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol 2002;13:319-323.
Tsai CF, Tai CT, Hsieh MH, Lin WS, Yu WC, Ueng KC, Ding YA, Chang MS, Chen SA. Initiation of atrial fibrillation by ectopic beats originating from the superior vena cava: Electrophysiological characteristics and results of radiofrequency ablation. Circulation 2000;102:67-74.
Goya M, Ouyang F, Ernst S, Volkmer M, Antz M, Kuck KH. Electroanatomic mapping and catheter ablation of breakthroughs from the right atrium to the superior vena cava in patients with atrial fibrillation. Circulation 2002;106:1317-1320.
Sun Y, Arruda M, Otomo K, Beckman K, Nakagawa H, Calame J, Po S, Spector P, Lustgarten D, Herring L, Lazzara R, Jackman W. Coronary sinus-ventricular accessory connections producing posteroseptal and left posterior accessory pathways: incidence and electrophysiological identification. Circulation 2002;106:1362-1367.
Tse HF, Lau CP, Kou W, Pelosi F, Oral H, Kim M, Michaud GF, Knight BP, Moscucci M, Strickberger SA, Morady F. Comparison of endocardial activation times at effective and ineffective ablation sites within the pulmonary veins. J Cardiovasc Electrophysiol 2000;11:155-159.
Volkmer M, Antz M, Hebe J, Kuck KH. Focal atrial tachycardia originating from the musculature of the coronary sinus. J Cardiovasc Electrophysiol 2002;13:68-71.
Pavin D, Boulmier D, Daubert JC, Mabo P. Permanent left atrial tachycardia: radiofrequency catheter ablation through the coronary sinus. J Cardiovasc Electrophysiol 2002;13:395-398.
Eckardt L. Automaticity in the coronary sinus. J Cardiovasc Electrophysiol 2002;13:288-289.
Corcoran SJ, Lawrence C, McGuire MA. The valve of Vieussens: An important cause of difficulty in advancing catheters into the cardiac veins. J Cardiovasc Electrophysiol 1999;10:804-808.
von Ludinghausen M. Clinical anatomy of cardiac veins, Vv. cardiacae. Surg Radiol Anat 1987;9:159-168.
Ortale JR, Gabriel EA, Iost C, Marquez CQ. The anatomy of the coronary sinus and its tributaries. Surg Radiol Anat 2001;23:15-21.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Katritsis, D.G., Giazitzoglou, E., Korovesis, S. et al. Conduction Patterns in the Cardiac Veins: Electrophysiologic Characteristics of the Connections Between Left Atrial and Coronary Sinus Musculature. J Interv Card Electrophysiol 10, 51–58 (2004). https://doi.org/10.1023/B:JICE.0000011485.98197.df
Issue Date:
DOI: https://doi.org/10.1023/B:JICE.0000011485.98197.df