Abstract
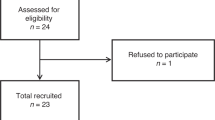
Postoperative hyponatremia in women has been associated with the development of serious neurological disorders and even death, with a predisposition for menstruant women. The objective of this study was to evaluate the immediate hormonal, water and electrolyte responses to pelvic surgery in both pre and postmenopausal women. Of the twenty-five consecutive women studied, twenty were premenopausal while five were postmenopausal. Mean age was 45.4 ± l.6 years. Measurements of plasma renin activity, follicular stimulating hormone and luteinizing hormone showed no significant change pre to postoperatively. There was a significant decrease in pre to postoperative values of estrogen, 97.4 ± 20.3 to 36.3 ± 7.5 pg/mL (p < 0.05). There was also a significant decline in postoperative values for plasma aldosterone and plasma progesterone. Data were similar in pre and postmenopausal patients. Serum sodium levels decreased from 141.5 ± 0.5 to 137.2 ± 0.5 mEq/L (p < 0.0l). During the twenty-four hours following surgery, mean net sodium balance was positive 122 mEq and mean measured fluid balance was positive 1108 mL. Ringers lactate or normal saline were used. On the first postoperative day, plasma arginine vasopressin levels were elevated at 4.0 ± 0.8 pg/mL, with a mean urine osmolality of 504 ± 29 mOsm/kg H2O. The data illustrate that women undergoing pelvic surgery decrease their serum sodium in the immediate postoperative period. Despite both positive sodium and water balance, there is a stronger tendency to conserve water. Decreased estrogen levels occur and this decrease may facilitate brain cell adaptation to plasma hypotonicity. Since the administration of isotonic fluid will not protect against the decrease in serum sodium, postoperative sodium concentration should be carefully monitored.
Similar content being viewed by others
References
Ayus JC, Arieff AI. Brain damage and postoperative hyponatremia: The role of gender. Neurology 1996; 46: 323–328.
Agraharkar M, Agraharkar A. Posthysteroscopic hyponatremia: Evidence for a multifactorial cause. Am J Kid Dis 1997; 30(5): 717–719.
Kozniewska E, Roberts TPL, Vexler ZS et al. Hormonal dependence of the effects of metabolic encephalopathy on cerebral perfusion and oxygen utilization in the rat. Circ Res 1995; 76: 551–558.
Arieff AI. Hyponatremia, convulsions, respiratory arrest, and permanent brain damage after elective surgery in healthy women. N Engl J Med 1986; 314: 1529–1535.
Ayus C, Wheeler JM, Arieff AI. Postoperative hyponatremic encephalopathy in menstruant women. Ann Int Med 1992; 117(11): 891–897.
Wijdicks EFM, Larson TS. Absence of postoperative hyponatremia syndrome in young, health females. Ann Neurol 1994; 35: 626–628.
Fieldman NR, Forsling ML, Le Quesne LP. The effect of vasopressin on solute and water excretion during and after surgical operations. Ann Surg 1985; 201(3): 383–390.
Fraser CL, Swanson RA. Female sex hormones inhibit volume regulation in rat brain astrocyte culture. Am J Physiol 1994; 267: C909–C914.
Vexler ZS, Ayus JC, Roberts TPL et al. Hypoxic and ischemic hypoxia exacerbate brain injury associated with metabolic encephalopathy in laboratory animals. J Clin Invest 1994; 93: 256–264.
Gowrishankar M, Chen CB, Cheema-Dhadli S, Halperin ML. Prevention of acute hyponatremia by mannitol: An unanticipated mechanism. Clin Nephrol 1998; 50(6): 352–360.
Gullick HD, Raisz LG. Changes in renal concentrating ability associated with major surgical procedures. N Engl J Med 1960; 262(26): 1309–1314.
Verbalis JG. Hyponatremia and Hypoosmolar Disorders. Primer on Kidney Diseases Academic Press, San Diego, 1994; 361–367.
Ayus JC, Arieff AI. Morbidity and Mortality from chronic symptomatic hyponatremia in elderly women. J Am Soc Nephrol 1998; 9: 104A.
Flear CTG, Gill GV. Hyponatremia: Mechanisms and management. Lancet 1981; 26–31.
Laragh JH, Atlas SA. Atrial natriuretic hormone: A regulator of blood pressure and volume homeostasis. Kidney Int 1988; 25(suppl): S64–S71.
Olson BR, Gumowski J, Rubino D, Oldfield EH. Pathophysiology of hyponatremia after transsphenoidal pituitary surgery. J Neurosurg 1997; 87: 499–507.
Soupart A, Penninckx R, Stenuit A, Decaux G. Lack of major hypoxia and significant brain damage in rats despite dramatic hyponatremic encephalopalthy. J Lab Clin Med 1997; 130: 226–231.
Fraser CL, Sarnacki P. Na+-ATPase pump function in rat brain synaptosomes is different in males and females. Am J Physiol 1989; 257: E284–E289.
Gowrishankar M, Lin SH, Mallie JP et al. Acute hyponatremia in the perioperative period: Insights into its pathophysiology and recommendations for management. Clinical Nephrology 1998; 50(6): 352–360.
Moran WH, Miltenberger FW, Shuayb WA, Zimmerman B. The relationship of antidiuretic hormone secretion to surgical stress. Surgery 1964; 56(1): 99–108.
Ayus JC, Arieff AI. Glycine-induced hypo-osmolar hyponatremia. Arch Int Med 1997; 157: 223–226.
Steele A, Gowrishankar M, Abrahamson S et al. Postoperative hyponatremia despite near-isotonic saline infusion: A phenomenon of desalination. Ann Intern Med 1997; 126: 20–25.
Metzler CH, Ramsay DJ. Atrial peptide potentiates renal responses to volume expansion in conscious dogs. Am J Physiol 1989; 256: R284–R289.
Arieff AI, Kozniewska E, Roberts TPL et al. Age, gender, and vasopressin affect survival and brain adaptation in rats with metabolic encephalopathy. Am J Physiol 1995; 268: R1143–R1152.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Amede, F.J., James, K.A., Michelis, M.F. et al. Changes in serum sodium, sodium balance, water balance, and plasma hormone levels as the result of pelvic surgery in women. Int Urol Nephrol 34, 545–550 (2002). https://doi.org/10.1023/A:1025601304345
Issue Date:
DOI: https://doi.org/10.1023/A:1025601304345