Abstract
Purpose. Activation of hepatic Kupffer cells (KCs) during organ preservation and subsequent reperfusion causes release of proinflammatory mediators and is responsible, at least in part, for rejection of transplanted livers. Our hypothesis was that donor pretreatment, before liver harvest, with methylprednisolone (MP) or its dextran prodrug (DMP) would reduce KC activation.
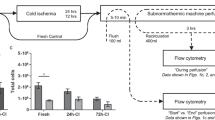
Methods. Adult donor rats were administered a single 5-mg/kg (MP equivalent) IV dose of MP or DMP or saline 2 h before liver harvest. The livers were then stored in University of Wisconsin solution for 24, 48, or 96 h (n = 4/treatment/time). A recirculating perfusion model was used to study, for 180 min, the release of KC activation markers, tumor necrosis factor (TNF)-α and acid phosphatase, and other biochemical indices from the cold-preserved livers.
Results. Cold ischemia-reperfusion resulted in release of substantial levels of TNF-α in untreated groups. Pretreatment of rats with MP or DMP caused a significant (p < 0.0001) reduction in TNF-α AUC in the perfusate, with no significant differences between MP and DMP. The maximum inhibitory effect of MP (77.5 ± 10.2%) was observed after 48 h of preservation, whereas DMP showed maximal inhibition of TNF-α AUC at both 24 (74.5 ± 15.8%) and 48 (74.8 ± 12.6%) h of preservation. Similarly, both MP and DMP resulted in a significant (p < 0.0004) decrease in acid phosphatase levels of cold-preserved livers. However, neither pretreatment had any substantial effect on the levels of other biochemical markers.
Conclusions. Both MP and DMP pretreatments decreased the release of TNF-α and acid phosphatase from livers subjected to cold ischemia preservation. Therefore, pretreatment of liver donors with MP or its prodrug decreases KC activation by cold ischemia-reperfusion.
Similar content being viewed by others
REFERENCES
J. J. Lemasters and R. G. Thurman. Reperfusion injury after liver preservation for transplantation. Annu. Rev. Pharmacol. Toxicol. 37:327–338 (1997).
D. Adams and J. M. Neuberger. Treatment of acute rejection. Semin. Liver Dis. 12:80–87 (1992).
S. N. Lichtman and J. J. Lemasters. Role of cytokines and cytokine-producing cells in reperfusion injury to the liver. Semin. Liver Dis. 19:171–187 (1999).
P. Schemmer, B. U. Bradford, M. L. Rose, H. Bunzendahl, J. A. Raleigh, J. J. Lemasters, and R. G. Thurman. Intravenous glycine improves survival in rat liver transplantation. Am. J. Physiol. 276:G924-G932 (1999).
K. Kozaki, H. Egawa, L. Bermudez, E. B. Keefe, S. K. So, and C. O. Esquivel. Effects of pentoxifylline pretreatment on Kupffer cells in rat liver transplantation. Hepatology 21:1079–1082 (1995).
M. Kukan, K. Vajdova, J. Horecky, A. Nagyova, H. M. Mehendale, and T. Trnovec. Effects of blockade of Kupffer cells by gadolinium chloride on hepatobiliary function in cold ischemia–reperfusion injury of rat liver. Hepatology 26:1250–1257 (1997).
J. Fornander, A. Hellman, and P. O. Hasselgren. Effects of methylprednisolone on protein synthesis and blood flow in the postischemic liver. Circ. Shock 12:287–295 (1984).
M. Wang, M. Sakon, K. Umeshita, M. Okuyama, K. Shiozaki, H. Nagano, K. Dohno, S. Nakamori, and M. Monden. Prednisolone suppresses ischemia–reperfusion injury of the rat liver by reducing cytokine production and calpain mu activation. J. Hepatol. 34:278–283 (2001).
X. Zhang and R. Mehvar. Dextran-methylprednisolone succinate as a prodrug of methylprednisolone: plasma and tissue disposition. J. Pharm. Sci. 90:2078–2087 (2001).
I. Ahmed, M. S. Attia, N. Ahmad, J. P. A. Lodge, and D. J. Potts. Use of isolated perfused rat liver model for testing liver preservation solutions. Transplant. Proc. 33:3709–3711 (2001).
G. E. Gondolesi, N. Lausada, G. Schinella, A. M. Semplici, M. S. Vidal, G. C. Luna, J. Toledo, P. M. deBuschiazzo, and J. C. Raimondi. Reduction of ischemia–reperfusion injury in parenchymal and nonparenchymal liver cells by donor treatment with DL-alpha-tocopherol prior to organ harvest. Transplant. Proc. 34:1086–1091 (2002).
I. V. Deaciuc, G. J. Bagby, M. R. Niesman, N. Skrepnik, and J. J. Spitzer. Modulation of hepatic sinusoidal endothelial cell function by Kupffer cells: an example of intercellular communication in the liver. Hepatology 19:464–470 (1994).
H. Nakano, K. Boudjema, E. Alexandre, P. Imbs, M. P. Chenard, P. Wolf, J. Cinqualbre, and D. Jaeck. Protective effects of N-acetylcysteine on hypothermic ischemia–reperfusion injury of rat liver. Hepatology 22:539–545 (1995).
J. C. Caldwell-Kenkel, R. G. Thurman, and J. J. Lemasters. Selective loss of nonparenchymal cell viability after cold ischemic storage of rat livers. Transplantation 45:834–837 (1988).
T. Higa, M. Shiraishi, S. Hiroyasu, H. Tomori, Y. Okuhama, T. Kusano, and Y. Muto. Effect of exogenous L-arginine for hepatic ischemia–reperfusion injury in an isolated rat liver in vitro. Transplant. Proc. 30:3728–3729 (1998).
R. Mehvar. Simultaneous analysis of dextran-methylprednisolone succinate, methylprednisolone succinate, and methylprednisolone by size-exclusion chromatography. J. Pharm. Biomed. Anal. 19:785–792 (1999).
A. N. Kong and W. J. Jusko. Disposition of methylprednisolone and its sodium succinate prodrug in vivo and in perfused liver of rats: nonlinear and sequential first-pass elimination. J. Pharm. Sci. 80:409–415 (1991).
R. V. Lenth. Some practical guidelines for effective sample size determination. Am. Stat. 55:187–193 (2001).
H. Itasaka, T. Suehiro, S. Wakiyama, K. Yanaga, M. Shimada, and K. Sugimachi. The mechanism of hepatic graft protection against reperfusion injury by prostaglandin E1. Surg. Today 29:526–532 (1999).
E. Mishina, R. Straubinger, N. Pyszczynski, and W. Jusko. Enhancement of tissue delivery and receptor occupancy of methylprednisolone in rats by a liposomal formulation. Pharm. Res. 10:1402–1410 (1993).
R. Mehvar and X. P. Zhang. Development and application of an isolated perfused rat liver model to study the stimulation and inhibition of tumor necrosis factor-α production ex vivo. Pharm. Res. 19:47–53 (2002).
A. P. Chimalakonda and R. Mehvar. Dextran-methylprednisolone succinate as a prodrug of methylprednisolone: local immunosuppressive effects in liver after systemic administration to rats. Pharm. Res. 20:198–204 (2003).
R. Mehvar, R. O. Dann, and D. A. Hoganson. Simultaneous analysis of methylprednisolone, methylprednisolone succinate, and endogenous corticosterone in rat plasma. J. Pharm. Biomed. Anal. 22:1015–1022 (2000).
O. Le Moine, H. Louis, A. Demols, F. Desalle, F. Demoor, E. Quertinmont, M. Goldman, and J. Deviere. Cold liver ischemia–reperfusion injury critically depends on liver T cells and is improved by donor pretreatment with interleukin 10 in mice. Hepatology 31:1266–1274 (2000).
R. Wiesner, J. Ludwig, R. Krom, J. Steers, M. Porayko, G. Gores, and J. Hay. Treatment of early cellular rejection following liver transplantation with intravenous methylprednisolone. The effect of dose on response. Transplantation 58:1053–1056 (1994).
M. S. Cattral, L. B. Lilly, and G. A. Levy. Immunosuppression in liver transplantation. Semin. Liver Dis. 20:523–531 (2000).
M. Lutterova, Z. Szatmary, M. Kukan, D. Kuba, and K. Vajdova. Marked difference in tumor necrosis factor-alpha expression in warm ischemia-and cold ischemia–reperfusion of the rat liver. Cryobiology 41:301–314 (2000).
I. Marzi, Z. Zhong, J. J. Lemasters, and R. G. Thurman. Evidence that graft survival is not related to parenchymal cell viability in rat liver transplantation. The importance of nonparenchymal cells. Transplantation 48:463–468 (1989).
R. Sundberg, S. Lindell, N. V. Jamieson, J. H. Southard, and F. O. Belzer. Effects of chlorpromazine and methylprednisolone on perfusion preservation of rabbit livers. Cryobiology 25:417–424 (1988).
J. A. Handler, D. C. Kossor, and R. S. Goldstein. Assessment of hepatobiliary function in vivo and ex vivo in the rat. J. Pharmacol. Toxicol. Methods 31:11–19 (1994).
X. Bossuyt, M. Muller, B. Hagenbuch, and P. J. Meier. Polyspecific drug and steroid clearance by an organic anion transporter of mammalian liver. J. Pharmacol. Exp. Ther. 276:891–896 (1996).
X. Wu, R. Kekuda, W. Huang, Y. J. Fei, F. H. Leibach, J. Chen, S. J. Conway, and V. Ganapathy. Identity of the organic cation transporter OCT3 as the extraneuronal monoamine transporter (uptake2) and evidence for the expression of the transporter in the brain. J. Biol. Chem. 273:32776–32786 (1998).
R. Mehvar and D. A. Hoganson. Dextran-methylprednisolone succinate as a prodrug of methylprednisolone: immunosuppressive effects after in vivo administration to rats. Pharm. Res. 17:1402–1407 (2000).
T. Yamada, H. Hirose, Y. Mori, E. Sasaki, A. Onitsuka, M. Hayashi, S. Senga, N. Futamura, K. Sakamoto, T. Sago, M. Yasumura, and H. Iwata. An experimental estimation of the maximum period of liver preservation using dielectric parameters. Transplant Proc. 34:1098–1104 (2002).
H. Furukawa, S. Todo, O. Imventarza, A. Casavilla, Y. M. Wu, C. Scotti-Foglieni, B. Broznick, J. Bryant, R. Day, and T. E. Starzl. Effect of cold ischemia time on the early outcome of human hepatic allografts preserved with UW solution. Transplantation 51:1000–1004 (1991).
K. Claesson, S. Lindell, J. H. Southard, and F. O. Belzer. Chlorpromazine, quinacrine, and verapamil as donor pretreatment in liver preservation, tested in the isolated perfused rat liver. Cryobiology 28:422–427 (1991).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chimalakonda, A.P., Mehvar, R. Attenuation of Kupffer Cell Activation in Cold-Preserved Livers After Pretreatment of Rats with Methylprednisolone or Its Macromolecular Prodrug. Pharm Res 20, 1001–1008 (2003). https://doi.org/10.1023/A:1024402121053
Issue Date:
DOI: https://doi.org/10.1023/A:1024402121053