Abstract
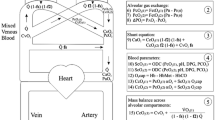
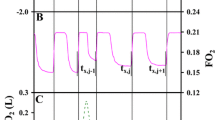
Objectives.This work attempts to show how pulmonary blood flow (Qp), cardiac output (COFick) and the lung volume of effective gas exchange (ELV ) can be determined from breath-by-breath measurements of the tidal exhaled CO2 elimination V (litre/min) and the end tidal CO2 concentration P (%) using the differential Fick method. The measurements are made during steady state ventilation and when the CO2 balance in the lungs changes subsequent to a perturbation of the gas exchange conditions. Methods.A short breath hold is used to implement such a perturbation. V and P were measured in patients on mechanical ventilation. When the end tidal CO2 values were stable, the end inspiratory pause of a single breath was prolonged 3 seconds as compared to the normal ventilation pattern. From the changes induced in P and V, Qp, COFick and ELV are obtained. Results:Cardiac output values were measured in 18 patients after CABG. COFick was found to be in good agreement with the thermodilution cardiac output reference COth. (n= 51 and (COth–COFick) with Mean = −0.17 litre/minute and SD = 0.62 litre/minute). Conclusions.With a single breath perturbation, the differential Fick method can yield cardiopulmonary information using 2–3 breaths only and with a minimum of interference with the patient. Complete data analysis results in multiple determinations of the Qp and ELV values which improve the attainable precision. Our investigation points to the possibility to determine Qp, COFick and ELV also during spontaneous breathing, by using the natural tidal variations of V and P.
Similar content being viewed by others
REFERENCES
Löwy A, v Schrötter H. Untersuchungen uber die Blutcirkulation beim Menschen. Zeitschr f exp Pathol u Therapie 1905; 1: 197-311
Kirsch F, Schwarz H. Das Herzschlagvolumen und die Methodik seiner Bestimmung. Ergebnisse der Inneren Med uKi nderheilkunde 1925; 27: 170-244
Nunn J. Applied Respiratory Physiology, 4th ed. Oxford England: Butterworth Ltd, 1993
Gedeon A, Forslund L, Hedenstierna G, Romano E. A new method for noninvasive bedside determination of pulmonary blood flow. Med Biol Eng Comput 1980; 18: 411-418
Gedeon A. Noninvasive pulmonary blood flow for optimal PEEP. Clin Physiol 1985; 5 (Suppl 3): 49-58
Capek JM, Roy RJ. Noninvasive measurement of cardiac output using partial CO2 rebreathing. IEEE Trans Biomed Eng 1988; 35: 653-661
Gama de Abreu M, Quintel M, Ragaller M, Albreth M. Partial carbon dioxide rebreathing: A reliable technique for noninvasive measurement of nonshunted pulmonary capillary blood flow. Crit Care Med 1997; 25: 675-683
Orr JA, Westenskow DR, Kofoed S, Turner R. A noninvasive cardiac output system using the partial rebreathing Fick method. J Clin Monit 1996; 12: 464-465 (Abstract)
Gedeon A, Krill P, Kristensen J, Gottlieb I. Noninvasive cardiac output determined with a new method based on gas exchange measurements and carbon dioxide rebreathing: A study in animals/pigs. J Clin Monit 1992; 8: 267-278
Linnarson D, Larsson H. Pulmonary blood flow determination with selective rebreathing of CO2. Clin Physiol 1985; 5 (Suppl 3): 39-48
Jaffe BM. Partial CO2 rebreathing cardiac output-operating principles of the NICOTM system. J Clin Monit 1999; 15: 387-401
Gedeon A, Österlund B. Effective lung volume (ELV) measured with a breath holding technique to evaluate PEEP therapy 11th Annual Congr Eur Soc Int Care Med 1998; 24 (Suppl 1): S117 (Abstract 366)
Hyde WR, Puy JMR, Raub FW, Forster ER. Rate of disappearance of labeled carbon dioxide from the lungs of humans during breath holding: A method for studying the dynamics of pulmonary CO2 exchange. J Clin Invest 1968; 47: 1535-1550
Plewes JL, Olszowka AJ, Farhi LE. Amount and rates of CO2 storage in lung tissue. Resp Physiol 1976; 28: 359-370
Dubois AB. Alveolar CO2 and O2 during breath holding, expiration, and inspiration. J Appl Physiol 1952; 5: 1-12
Knowles HJ, Newman W, Fenn OW. Determination of oxygenated, mixed venous blood CO2 tension by a breath-holding method. J Appl Physiol 1960; 15 (2): 225-228
Kim TS, Rahn H, Farhi LE. Estimation of true venous and arterial Pco2 by gas analysis of a single breath. J Appl Physiol 1966; 21 (4): 1338-1344
Hoffstein V, Rebuck AS. Determination of cardiac output based on breath-holding. Crit Care Med 1980; 8: 671-674
Arnold JH, Stenz R, Greiner B, Thompson JE, Arnold LW. Single breath CO2 analysis in an animal model of acute lung injury and pulmonary hypoperfusion. Anesthesiology 1995; 83 (3A): A465
Deriaz H, Song Q, Delva E, Lienhart A. Relationship between cardiac output and end-tidal carbon dioxide tension in anesthesized patients. Anesthesiology 1993; 79 (3A): A509
Shibutani K, Shirasaki S, Kubal K, Gupte P. Changes in cardiac output affect PETCO2 and CO2 transport during unsteady state in man. Anesthesiology 1992: 77 (3A): A468
Murray IP, Modell HJ, Gallagher TJ, Banner JM. Titration of PEEP by the arterial minus end-tidal carbon dioxide gradient. Chest 1984; 85: 100-104
Lachmann B. Open up the lung and keep the lung open. Intensive Care Med 1992; 18: 319-321
Kallas JH, Domino BK, Glenny WR, Andersson AE, Hlastala PM. Pulmonary blood flow redistribution with low levels of positive end-expiratory pressure. Anesthesiology 1998; 88: 1291-1299
Wagner PD, West JB. Ventilation-perfusion relationships. In: West J B, ed. Pulmonary gas exchange. New York: Academic Press, 1980
Gedeon A, Krill P, Kristenssen J, Hedenstierna G. Method for clinical determination of VA/Q distributions. Comparison with results from the Multiple Inert Gas Elimination Technique (MIGET). Crit Care Med 1997; 25: A96 (Abstract 196)
Pettenkofer M. Ueber einen neuen Respirations-Apparat. Abh d k Ak d Wiss 1861; II: 231-276
Österlund B, Gedeon A, Krill P, Johansson G, Reiz S. A new method of using gas exchange measurements for the noninvasive determination of cardiac output: Clinical experiences in adults following cardiac surgery. Acta Anaesth Scand 1995; 39: 727-732
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gedeon, A., Krill, P. & Österlund, B. Pulmonary Blood Flow (Cardiac Output) and the Effective Lung Volume Determined from a Short Breath Hold Using the Differential Fick Method. J Clin Monit Comput 17, 313–321 (2002). https://doi.org/10.1023/A:1021232624767
Issue Date:
DOI: https://doi.org/10.1023/A:1021232624767