Abstract
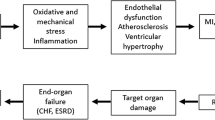
Background. ACE inhibition reduces morbidity and mortality among a variety of patients. Among mechanisms explaining these beneficial effects are the effects on the sympathetic system and on local vasodilating substances such as nitric oxide and bradykinins at the level of the endothelium. The PERFECT study was designed to verify the above mentioned pathophysiological concepts.
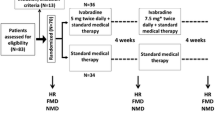
Methods. The PERFECT study is a study nested within the EUROPA trial, a three year double-blind, multi-centre, placebo-controlled randomised study that aims at studying the effect of the ACE-inhibitor Perindopril on morbidity and mortality in over 12,000 patients with stable coronary artery disease without clinical heart failure. The PERFECT study is designed as a parallel group randomised placebo controlled trial to determine the effect of Perindopril (8 mg) on brachial artery endothelial function in patients with stable coronary artery disease without clinical heart failure. In the PERFECT study, B-mode ultrasonography of the brachial artery is used as a model for changes in the coronary arteries. Endothelial function in response to ischaemia (reactive hyperaemia) and to vasoconstriction (cold pressor test) is assessed. The ischemia test is used a model to assess the effects of ACE inhibition on nitric oxide/bradykinine mediated vasodilatatory response to ischaemia, whereas the cold pressor test is applied to assess the effect of ACE inhibition on the neurohormonal response. The recruitment for the PERFECT study started in May 1998 en was completed in June 1999. 345 patients were recruited in 20 European centers. The Vascular Imaging Center Utrecht, an ultrasound core laboratory, is performing the endothelial function measurements. The primary study outcomes are (1) percentage change in flow-mediated vasodilatation of the brachial artery between the 36 month measurement and the baseline measurement and (2) percentage change in neurohormonal mediated vasoconstriction of the brachial artery between the 36 month measurement and the baseline measurement. The size of the study allows detection of an absolute difference in FMD of 2.0% with a 90% power and a two-sided alpha of 5%.
Conclusion. The findings of the PERFECT study may help to understand and explain the effects of ACE inhibition, in particular Perindopril, on cardiovascular morbidity and mortality.
Similar content being viewed by others
References
CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure: Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med 1987;316:1429–1435.
Kjekshus J, Swedberg K, Snapinn S. Effects of enalapril on long-term mortality in severe congestive heart failure: CONSENSUS trial group. Am J Cardiol69:103–107.
SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fraction and congestive heart failure. N Engl J Med 1991;325:293–302.
Acute Infarction Ramipril Efficacy (AIRE) Study Investigators. Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet 1993;342:821–828.
Hall AS, Murray GD, Ball SG. Follow-up study of patients randomly allocated ramipril or placebo for heart failure after acute MI: AIRE Extension (AIREX) study. Lancet 1997;349:1493–1497.
SAVE Investigators, Pfeffer MA, Braunwald E, Moye LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after MI: Results of the Survival and Ventricular Enlargement trial. N Engl J Med 1992;327:669–677.
SOLVD Investigators. Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. N Engl J Med 1992;327:685–691.
CONSENSUS-II Study Group, Swedberg K, Held P, Kjekshus J, et al. Effects of the early administration of enalapril on mortality in patients with acute MI: Results of the CooperativeNewScandinavian Enalapril Survival study II (CONSENSUS-11). N Engl J Med 1992;327:678–684.
Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico, GISSI-3: Effects of lisinopril and transdermal glyceryl trinitrate singly and together on sixweek mortality and ventricular function after acute MI. Lancet 1994;343:1115–1122.
ISIS-4 (Fourth International Study of Infarct Survival) Collaborative Group, ISIS-4: A randomized factorial trial assessing early oral captopril, oral mononitrate and intravenous magnesitun sulphate in 58,050 patients with suspected acute MI. Lancet 1995;345:669–685.
Survival of MI Long-term Evaluation (SMILE) Study Investigators, Ambrosioni E, Borghi C, Magnani B. The effect of the angiotensin-converting enzyme inhibitor zofenopril on mortality and morbidity after anterior MI.NEngl J Med 1995;332:80–85.
Rutherford JD, Pfeffer MA, Moye LA, et al. Effects of captopril on ischemic events after MI: Results of the Survival And Ventricular Enlargement trial (SAVE investigators). Circulation 1994;90:1731–1738.
Yusuf S, Pepine CJ, Garces C, et al. Effect of enalapril on MI and unstable angina in patients with low ejection fractions. Lancet 1992;340:1173–1178.
Borghi C, Ambrosioni E, Evidence-based medicine andACE inhibition. J Cardiovasc Pharmacol 1998;32 Suppl 2:S24–S35.
Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensinconverting enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients: The Heart Outcomes Prevention Evaluation study investigators. N Engl J Med 2000;342:145–153.
Simoons ML, Vos J, de Feyter PJ, et al. EUROPA substudies, confirmation of pathophysiological concepts. European trial on reduction of cardiac events with perindopril in stable coronary artery disease. Eur Heart J 1998;19 Suppl J:J56–J60.
TheEUROPAtrial: Design, baseline demography and status of the substudies. Cardiovasc Drugs Ther 2001;15(2):169–179.
Khalil ME, Basher AW, Brown EJ Jr, Alhaddad IA. A remarkable medical story: Benefits of angiotensin-converting enzyme inhibitors in cardiac patients. J Am Coll Cardiol 2001;37:1757–1764.
Barsotti A, Di Napoli P, Taccardi AA, et al. MK-954 (losartan potassium) exerts endothelial protective effects against reperfusion injury: Evidence of an e-NOS mRNA overexpression after global ischemia. Atherosclerosis 2001;155:53–59.
Luvara G, Pueyo ME, Philippe M, et al. Chronic blockade of NO synthase activity induces a proinflammatory phenotype in the arterial wall: Prevention by angiotensin II antagonism. Arterioscler Thromb Vasc Biol 1998;18:1408–1416.
Huang H, Arnal JF, Llorens-Cortes C, et al. Discrepancy between plasma and lung angiotensin-converting enzyme activity in experimental congestive heart failure: A novel aspect of endothelium dysfunction. Circ Res 1994;75:454–461.
Lewis DA, Rud KS, Miller VM. Endothelium-dependent relaxation by angiotensin-converting enzyme inhibitors in canine femoral arteries. J Cardiovasc Pharmacol 1993;22:443–448.
Thuillez C, Mulder P, Elfertak L, et al. Prevention of endothelial dysfunction in small and large arteries in a model of chronic heart failure: Effect of angiotensin-converting enzyme inhibition. Am J Hypertens 1995;8:7S–12S.
Anderson T. Current trials on angiotensin-converting enzyme inhibitors and endothelial dysfunction. Can J Cardiol 1998;14 Suppl D:33D–34D.
Mancini GBJ, Henry GC, Macaya C, et al. Angiotensinconverting enzyme inhibition with quinapril improves endothelial vasomotor dysfunction in patients with coronary artery disease: The TREND (Trial on Reversing Endothelial Dysfunction) study. Circulation 1996;94:258–265.
Hornig B, Drexler H. Endothelial function and bradykinin in humans. Drugs 1997;54 Suppl 5:42–47.
Mancini GB. Long-term use of angiotensin-converting enzyme inhibitors to modify endothelial dysfunction: A review of clinical investigations. Clin Invest Med 2000;23:144–161.
Taddei S, Virdis A, Ghiadoni L, et al. Effects of angiotensinconverting enzyme inhibition on endothelium-dependent vasodilation in essential hypertensive patients. J Hypertens 1998;16:447–456.
Nakamura M, Funakoshi T, Arakawa N, et al. Effect of angiotensin-converting enzyme inhibitors on endothelium dependent peripheral vasodilation in patients with chronic heart failure. J Am Coll Cardiol 1994;24:1321–1327.
Hornig B, Arakawa N, Drexler H. Effect of ACE inhibition on endothelial dysfunction in patients with chronic heart failure. Eur Heart J 1998;19 Suppl G:G48–G53.
Remme WJ, Kruijssen HACM, LookMP, et al. Systemic and cardiac neuro-endocrine activation and severity of myocardial ischemia in humans. J Am Coll Cardiol 1994;23:82–91.
Remme WJ. The sympathetic nervous system and ischaemic heart disease. Eur Heart J 1998 Jun;19 Suppl F:F62–F71.
Bartels GL, van den Heuvel FM, vanVeldhuisen DJ, van der Ent M, Remme WJ. Acute anti-ischemic effects of perindoprilat in men with coronary artery disease and their relation with left ventricular function. Am J Cardiol 1999;83:332–336.
Isabelle Antony, Guy Lerebours, Alain Nitenberg. Angiotensin-converting enzyme inhibition restores flow-dependent and cold pressor test-induced dilations in coronary arteries of hypertensive patients. Circulation 1996;94: 3115–3122.
Roos de, NM, Bots ML, Katan MB. Replacement of dietary saturated fatty acids by trans fatty acids lowers serumHDL cholesterol and impairs endothelial function in healthy men and women. Arterioscl Tromb Vasc Biol 2001;21:1233–1237.
Roos NM de, Bots ML, Schouten E, Katan MB. Flow mediated vasodilatation is not impaired when HDL cholesterol is lowered by substituting carbohydrates for monounsaturated fat. Br J Nutr 2001;86:181–188.
Wilmink HW, de Kleijn MJJ, Bots ML, et al. Lipoprotein (a) is associated with endothelial function in healthy postmenopausal women. Atherosclerosis 2000;153:249–254.
Celemajer DS, Adams MR, Clarkson P, et al. Passive smoking and impaired endothelium dependent arterial dilatation in healthy young adults. N Eng J Med 1996;334:150–154.
Anderson TJ, Uehata A, Gerhard MD, et al. Close relation of endothelial function in the human coronary and peripheral circulations. J Am Coll Cardiol 1995;26:1235–1241.
Moncada S, Palmer RMJ, Higgs EA. Nitric oxide: Physiology, pathophysiology and pharmacology. Pharmacol Rev 1991;43:109–142.
Joannides R, Haefeli WE, Linder L, et al. Nitric oxide is responsible for flow dependent dilatation of human peripheral conduit arteries in vivo. Circulation 1995;91:1314–1319.
Motoyama T, Kawano H, Kugiyama K, et al. Flow mediated endothelium dependent dilatation of the brachial arteries is impaired in patients with coronary spastic angina.AmHeart J 1997;133:263–267.
Jensen-Urstad KJ, Reichard PG, Rosfors JS, et al. Early atherosclerosis is retarded by improved long-term glucose control in patients with IDDM. Diabetes 1996;45:1253–1258.
Celemajer DS, Sorensen KE, Bull C, Robinson J, Deanfield. Endothelium dependent dilatation in the systemic arteries of asymptomatic subjects relates to coronary risk factors and their interaction. J Am Coll Cardiol 1994;24:1468–1474.
Sorensen KE, Celermajer DS, Spiegelhalter DJ, et al. Noninvasive measurement of human endothelium dependent arterial responses: Accuracy and reproducibility. Br Heart J 1995;74:247–253.
SchachingerV, Britten MB, Zeiher AM. Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation 2000;101:1899–1906.
Suwaidi JA, Hamasaki S, Higano ST, Nishimura RA, Holmes DR Jr, Lerman A. Long-term follow-up of patients with mild coronary artery disease and endothelial dysfunction. Circulation 2000;101:948–954.
Perticone F, Ceravolo R, Pujia A, et al. Prognostic significance of endothelial dysfunction in hypertensive patients. Circulation 2001;104:191–196.
Doshi SN, Lewis MJ, Goodfellow J. Improving endothelial vasomotor function. May reduce cardiovascular risk, but the current evidence is circumstantial. BMJ 2001;323:352–353.
Corretti MC, Plotnick GD, Vogel RA. Smoking correlates with flow-mediated brachial artery vasoactivity but not cold pressor vasoactivity in men with coronary artery disease. Int J Card Imaging 1998;14:11–17.
Rubenfire M, Rajagopalan S, Mosca L. Carotid artery vasoreactivity in response to sympathetic stress correlates with coronary disease risk and is independent of wall thickness. J Am Coll Cardiol 2000;36:2192–2197.
Corretti MC, Plotnick GD, Vogel RA. Correlation of cold pressor and flow-mediated brachial artery diameter responses with the presence of coronary artery disease. Am J Cardiol 1995;75:783.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Bots, M.L., Remme, W.J., Lüscher, T.F. et al. PERindopril—Function of the Endothelium in Coronary Artery Disease Trial: The PERFECT Study—Sub Study of EUROPA: Rationale and Design. Cardiovasc Drugs Ther 16, 227–236 (2002). https://doi.org/10.1023/A:1020600522518
Issue Date:
DOI: https://doi.org/10.1023/A:1020600522518