Abstract
In order to investigate the clinical characteristics, neuroimaging findings, pathological features, treatment, and outcomes, and to provide valuable guidance for the diagnosis and management of intracranial gangliogliomas, 34 cases of intracranial gangliogliomas were retrospectively analyzed.
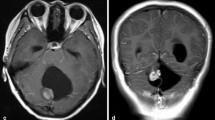
This study included 23 males and 11 females. Age at operation ranged from 17 days to 50 years. All patients had preoperative magnetic resonance imaging (MRI). Computed tomography (CT), magnetic resonance spectroscopy (MRS), 18F-FDG–PET (positron emission tomography), and 99Tc-HMPAO-SPECT (single photon emission computed tomography) were also performed in some cases. All pathological specimens and all available neuroimages were re-evaluated. The follow-up period varied from 12 to 89 months (mean 36 months). Seizure was the most common presenting symptom (85%). Tumor calcification was detected by CT scan in six of 11 cases. Seventeen gangliogliomas (50%) showed cystic components and 18 tumors (53%) were enhanced on MRI. All temporal lobe gangliogliomas were located intracortically and most of them had poor demarcation on MRI. In comparison with the contralateral normal area, the gangliogliomas showed a reduced Cho/Cr and NAA/Cr ratio, and an increased Cho/NAA ratio. On 18F-FDG-PET, gangliogliomas were usually hypometabolic. HMPAO-SPECT indicated tumor hypoperfusion or isoperfusion. A gross total resection was achieved in 25 patients. Tumor progression was observed in three patients who underwent an incomplete tumor resection. Two of them underwent a malignant transformation to a glioblastoma. Twenty-seven patients could carry on their normal life activity with the Karnofsky Performance Scale (KPS) of more than 80.
Even though ganglioglioma is a slowly growing benign tumor, which could be demonstrated by magnetic resonance spectroscopy (MRS), PET, and SPECT, there is a chance of malignant transformation, especially in cases of incomplete tumor resection. Gangliogliomas should be resected gross totally, if feasible, to achieve the best long-term outcomes.
Similar content being viewed by others
References
Kleihues P, Cavanee WK (eds): Pathology and Genetics of Tumours of the Nervous System: World Health Organization Classification of Tumours. International Agency for Research on Cancer, Lyon, 2nd edn, 2000
Campos MG, Zentner J, Ostertun B, Wolf HK, Schramm J: Anaplastic ganglioglioma: case report and review of the literature. Neurol Res 16: 317–320, 1994
Hall WA, Yunis EJ, Albright AL: Anaplastic ganglioglioma in an infant: case report and review of the literature. Neurosurgery 19: 1016–1020, 1986
Jay V, Squire J, Becker LE, Humphreys R: Malignant transformation in a ganglioglioma with anaplastic neuronal and astrocytic components. Cancer 73: 2862–2868, 1994
Silver JM, Rawlings III CE, Rossitch E, Zeidman SM, Friedman AH: Ganglioglioma: a clinical study with longterm follow-up. Surg Neurol 35: 261–266, 1991
Rumana CS, Valadka AB, Contant CF: Prognostic factors in supratentorial ganglioglioma. Acta Neurochir 141: 63–69, 1999
Isimbaldi G, Sironi M, Tonnarelli GP, Roncoroni M, Declich P, Galli C: Ganglioglioma: a clinical and pathological study of 12 cases. Clinical Neuropathology 15: 192–199, 1996
Mickle JP: Ganglioglioma in children. A review of 32 cases at the University of Florida. Pediatr Neurosurg 18: 310–314, 1992
Seong SO, Chang KH, Song IC, Han MH, Kim HD, Yeon KM, Han MC: In vivo H-1 MR Spectroscopy of intracranial solid tumors. J Korean Soc Magn Reson Med 1: 86–93, 1997
Palmini A, Andermann F, Olivier A, Tampieri D, Robitaille Y: Focal neuronal migration disorders and intractable partial epilepsy: results of surgical treatment. Ann Neurol 30: 750–757, 1991
Haddad SF, Moore SA, Menezes AH, VanGilder JC: Ganglioglioma: 13 years of experience. Neurosurgery 31: 171–178, 1992
Henriksen O: MR spectroscopy in clinical research. Acta Radiol 35: 96–116, 1994
Poptani H, Gupta RK, Roy R, Pandey R, Jain VK, Chhabra DK: Characterization of intracranial mass lesions with in vivo proton MR spectroscopy. AJNR Am J Neuroradiol 16: 1593–1603, 1995
Kincaid PK, El-Saden SM, Park SH, Goy BW: Cerebral gangliogliomas: preoperative grading using FDG-PET and 201Tl-SPECT. AJNR Am J Neuroradiol 19: 801–806, 1998
Davis WK, Boyko OB, Hoffman JM, Hanson MW, Schold SC Jr, Burger PC, Friedman AH, Coleman RE: [18F]2-fluoro-2-deoxyglucose-positron emission tomography correlation of gadolinium-enhanced MR imaging of central nervous system neoplasia. AJNR Am J Neuroradiol 14: 515–523, 1993
Dash RC, Provenzale JM, McComb RD, Perry DA, Longee DC, McLendon RE: Malignant supratentorial ganglioglioma (ganglion cell-giant cell glioblastoma). A case report and review of the literature. Arch Path Lab Med 123: 342–345, 1999
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Im, SH., Chung, C.K., Cho, BK. et al. Intracranial Ganglioglioma: Preoperative Characteristics and Oncologic Outcome after Surgery. J Neurooncol 59, 173–183 (2002). https://doi.org/10.1023/A:1019661528350
Issue Date:
DOI: https://doi.org/10.1023/A:1019661528350