Abstract
Introduction: Limitations in lesion volume and particularly lesion depth may negatively effect the efficacy of catheter ablation procedures using radiofrequency energy. This study evaluated the safety and efficacy of myocardial ablation using direct intramural injection of ethanol with a novel injection catheter system.
Methods: Left ventricular lesions were performed in 9 male swine (80–85 pounds); two animals were studied 6 weeks following anterior infarction produced by agarose gel embolization. An 8 Fr deflectable catheter equipped with a 27 gauge adjustable depth, retractable needle was directed to the LV using a retrograde aortic approach. Lesion deployment was guided by fluoroscopy and intracardiac echocardiography (ICE). Lesion characteristics were assessed with ICE imaging and pathologic analysis.
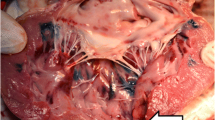
Results: Ethanol lesions were confined to the tissue directly adjacent to the injection port. Lesions were intramural with no evidence of overlying thrombus. Lesions delivered with a single port injection needle in normal myocardium (n = 24) averaged 1910 ± 1066 mm3 with a depth of 8.9 ± 3.3 mm. Lesions directed to infarct border zones (n = 4) averaged 929 ± 882 mm3 with a depth of 4.3 ± 2.8 mm. Lesions were immediately evident on ICE imaging, and were visualized by increased echo density and tissue swelling. Pathological analysis revealed homogenous lesions with intramural hemorrhage and contraction band necrosis.
Conclusions: Myocardial catheter ablation using direct ethanol injection is feasible, and relatively large and deep intramural lesions can be delivered, even in the infarct border zone. This technique may prove useful in ablation of arrhythmia substrates that are deep to the endocardial surface.
Similar content being viewed by others
References
Simmers TA, Wittkampf FHM, Hauer RNW. Robles de Medina EO: In vivo ventricular lesion growth in radiofrequency catheter ablation. PACE 1994;17:523–531.
Bartlett TG, Mitchell R, Friedman PL, Stevenson WG. Histologic evolution of radiofrequency lesions in an old human myocardial infarct causing ventricular tachycardia. J Cardiovasc Electrophysiol 1995;6:625–629.
Nakagawa H, Yamanashi WS, Pitha JV, et al. Comparison of in vivo tissue temperature profile and lesion geometry for radiofrequency ablation with a salineirrigated electrode versus temperature control in a canine thigh muscle preparation. Circulation 1995;91: 2264–2273.
Ruffy R, Imran MA, Santel DJ, Wharton JM. Radiofrequency delivery through a cooled catheter tip allows the creation of larger endomyocardial lesions in the ovine heart. J Cardiovasc Electrophysiol 1995;6:1089–1096.
Mittleman RS, Huang SK, de Guzman WT, Cuenoud H, Wagshal AB, Pires LA. Use of the saline infusion electrode catheter for improved energy delivery and increased lesion size in radiofrequency catheter ablation. PACE 1995;18:1022–1027.
Rothman SA, Hsia HH, Chmielewski IL, et al. Standard vs. saline irrigated-tip radiofrequency ablation: lesion size in normal vs scar tissue. J Am Coll Cardiol 1997;29:374A (abstract).
Delacretaz E, Stevenson WG, Winters GL, et al. Ablation of ventricular tachycardia with a saline-cooled radiofrequency catheter: anatomic and histologic characteristics of the lesions in humans. J Cardiovasc Electrophysiol 1999;10:860–865.
Callans DJ, Ren J-F, Narula N, Michele J, Marchlinski FE, Dillon SM. Effects of linear, irrigated-tip radiofrequency ablation in porcine healed anterior infarction. J Cardiovasc Electrophys 2001;12:1037–1042.
Zhou L, Keane D, Reed G, Ruskin JN. Thromboembolic complications of cardiac radiofrequency catheter ablation: a review of the reported incidence, pathogenesis and current research directions. J Cardiovasc Electrophys 1999;10:611–620.
Livraghi T, Bolondi L, Lazzaroni S, et al. Percutaneous ethanol injection in the treatment of hepatocellular carcinoma in cirrhosis. A study on 207 patients. Cancer 1992;69:925–929. Myocardial Ablation using Ethanol Injection 231
Castells A, Bruix J, Bru C, et al. Treatment of small hepatocellular carcinoma in cirrhotic patients: a cohort study comparing surgical resection and percutaneous ethanol injection. Hepatology 1993;18:1121–1126.
Inoue H, Waller BF, Zipes DP. Intracoronary ethyl alcohol or phenol injection ablates aconitine-induced ventricular tachycardia in dogs. J Am Coll Cardiol 1987;10:1342–1349.
Brugada P, de Swart H, Smeets JL, Wellens HJ. Transcoronary chemical ablation of ventricular tachycardia. Circulation 1989;79:475–482.
Kay GN, Bubien RS, Dailey SM, Epstein AE, Plumb VJ. A prospective evaluation of intracoronary ethanol ablation of the atrioventricular conduction system. J Am Coll Cardiol 1991;17:1634–1640.
Sneddon JF, Ward DE, Simpson IA, et al. Alcohol ablation of atrioventricular conduction. Br Heart J 1991;65:143–147.
Qi XQ, Sun RL, Tang CJ, et al. Transcoronary ethanol ablation of experimental ventricular tachycardia after epicardial ice mapping and localizing. Chinese Med J 1991;104:639–644.
Knight C, Kurbaan AS, Seggewiss H, et al. Nonsurgical septal reduction therapy for hypertrophic obstructive cardiomyopathy: outcome in the first series of patients. Circulation 1997;95:2075–2081.
Seggewiss H, Gleichmann U, Faber L, et al. Percutaneous transluminal septal myocardial ablation in hypertrophic obstructive cardiomyopathy: acute results and 3-month follow-up in 25 patients. J Am Coll Cardiol 1998;31:252–258.
Lakkis NM, Nagueh SF, Kleiman NS, et al. Echocardiography-guided ethanol septal reduction for hypertrophic obstructive cardiomyopathy. Circulation 1998;98:1750–1755.
Haines DE, Verow AF, Sinusas AJ, Whayne JG, DiMarco JP. Intracoronary ethanol ablation in swine: characterization of myocardial injury in target and remote vascular beds. J Cardiovasc Electrophysiol 1994;5:41–49.
Weismuller P, Mayer U, Richter P, et al. Chemical ablation by subendocardial injection of ethanol via catheter―preliminary results in the pig heart. Eur Heart J 1991;12:1234–1239.
Eldar M, Ohad D, Bor A, Varda-Bloom N, Swanson DK, Battler A. A closed chest pig model of sustained ventricular tachycardia. PACE 1994;17:1603–1609.
Callans DJ, Ren J-F, Michele J, Marchlinski FE, Dillon SM. Electroanatomic left ventricular mapping in the porcine model of healed anterior myocardial infarction: correlation with intracardiac echocardiography and pathologic analysis. Circulation 1999;100:1744–1750.
Ren JF, Marchlinski FE, Callans DJ, Zado ES. Echocardiographic lesion characteristics associated with successful ablation of inappropriate sinus tachycardia. J Cardiovasc Electrophysiol 2001;12:814–818.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Callans, D.J., Ren, JF., Narula, N. et al. Left Ventricular Catheter Ablation using Direct, Intramural Ethanol Injection in Swine. J Interv Card Electrophysiol 6, 225–231 (2002). https://doi.org/10.1023/A:1019505703083
Issue Date:
DOI: https://doi.org/10.1023/A:1019505703083