Abstract
Objective. To develop and evaluate alternative methods of adjusting primary medical care capitation payments for variations in relative need for health care among enrolled practice populations.
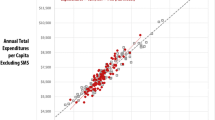
Methods. We developed alternative needs-based capitation formulae and applied them to a sample of capitation-funded primary care practices to assess each formula's performance against a reference standard of capitation payments based on age, sex and self-assessed health status of the enrolled populations. The alternative formulae were based on: (1) age and sex; (2) age, sex and individually-measured socioeconomic characteristics; (3) age, sex and socioeconomic characteristics imputed from census data for enrollees' neighbourhood of residence; (4) age, sex and standardized mortality ratio for enrollees' neighbourhood of residence.
Results. Age/sex-adjusted capitation payments for the six practices studied ranged from 10% higher to 18% lower than the reference standard payments. Capitation formulae based on socioeconomic and mortality data did not perform consistently better than the current age/sex-based formula.
Conclusions. Primary medical care capitation payments adjusted only for age and sex do not reflect the relative health care needs of enrolled practice populations. Our alternative formulae based on socioeconomic and mortality data also failed to reflect relative needs. Methods that use other approaches to adjusting for differences in relative need among enrolled populations should be investigated.
Similar content being viewed by others
References
S. Birch, J. Eyles and K.B. Newbold, Proxies for health care need among populations: validation of alternatives - a study in Quebec, J. Epidemiol. Community Health 50 (1996) 564–9.
W.G.W. Boerma, F.A.J.M. de Jong and P.H. Mulder, Health Care and General Practice Across Europe (Netherlands Institute of Primary Health Care (NIVEL), Utrecht, 1993).
C. Carter and J. Peel, Equalities and Inequalities in Health (Academic Press, London, 1976).
T. Crane, Hospital cost control in Norway: a decade's experience with prospective payment, Public Health Reports 100 (1985) 406–17.
A.R. Davies and J.E. Ware, Jr., Measuring Health perceptions in the Health Insurance Experiment (The Rand Corporation, Santa Monica, CA, 1981).
Department of Health and Social Security, Inequalities in Health (Department of Health and Social Security, London, 1980).
Department of Health and Social Security, Review of the resource allocation working party, Final report by the NHS Management Board, London, HMSO (1988).
R.G. Evans, M.L. Barer and T.R. Marmor, eds., Why Are Some People Healthy and Others Not? The Determinants of Health of Populations (Aldine de Gruyer, New York, 1994).
J. Eyles, From equalisation to rationalisation: public health care provision in New South Wales, Australian Geographical Studies 23 (1985) 243–68.
J. Eyles, S. Birch and S. Chambers, Fair shares for the zone: allocating health-care resources for the native populations of the Sioux Lookout zone, Northern Ontario, Canadian Geographer 38 (1994) 134–50.
J. Eyles and S. Birch, A population needs-based approach to health care resource allocation and planning in Ontario, Can. J. Public Health (1993) 112–17.
J. Eyles, S. Birch, S. Chambers, J. Hurley and B. Hutchison, A needs-based methodology for allocating health care resources in Ontario, Canada: development and an application, Social Science and Medicine 33 (1991) 489–500.
G.G. Fillenbaum, Social context and self-assessments of health among the elderly, Journal of Health and Social Behaviour 20 (1979) 45–51.
H.J. Friedsam and H.W. Martin, A comparison of self and physicians' health ratings in an older population, Journal of Health and Human Behaviour 4 (1963) 179–83.
General practice in the National Health Service: the 1990 contract, Health Departments of Great Britain (August 1989).
R. Gilbert, B. Gibberd and J. Stewart, The New South Wales resource allocation formula: a method for equitable health funding, Australian Health Review 15 (1992) 6–21.
M.dR. Giraldes, The equity and efficiency principle in the financing system of the NHS in Portugal, Health Policy 14 (1990) 13–28.
S. Greenland and J. Robins, Ecologic studies, Am. J. Epidemiol. 139 (1994) 747–71.
H.S.O. central agreement, Ministry of Health, Toronto (October, 1993).
Health Reforms Directorate, Population-based funding of regional health authorities for the purchase of core personal health services, New Zealand Ministry of Health (1992).
Health and Welfare Canada and Statistics Canada, The health of Canadians: report of the Canada Health Survey, Ottawa, Minister of Supply and Services Canada, Catalogue No. 82-538 (1981).
Health and Welfare Canada, Canada's Health Promotion Survey: technical report, Minister of Supply and Services Canada, Ottawa (1988).
S.C. Ho, Health and social predictors of mortality in an elderly Chinese cohort, Am. J. Epidemiol. 133 (1991) 907–21.
E.L. Idler and R.J. Angel, Self-rated health and mortality in the NHANES-1 Epidemiologic Follow-up Study, Am. J. Public Health 80 (1990) 446–52.
E.L. Idler, S.V. Kasl and J.H. Lemke, Self-evaluated health and mortality among the elderly in New Haven, Connecticut and Iowa and Washington counties, Iowa, 1982-1986, Am. J. Epidemiol. 131 (1990) 91–103.
R. Jamsen, Planning and Financing System for Social and Health Services (Ministry of Social Affairs and Health, Helsinki, 1994).
B. Jarman, Identification of underprivileged areas, Br. Med. J. 286 (1983) 1705–9.
B. Jarman, Underprivileged areas: validation and distribution of scores, Br. Med. J. 289 (1984) 1587–92.
G.A. Kaplan and T. Camacho, Perceived health and mortality: a nine-year follow-up of the human population laboratory cohort, Am. J. Epidemiol. 117 (1983) 292–304.
G. Kaplan, V. Barell and A. Lusky, Subjective state of health and survival in elderly adults, J. Gerontol. 43 (1988) S114–20.
A. Krasnik, P.V. v.Scholten and M.T. Damsgaard, General practitioners' attitudes to a recent change in their remuneration system, Scand. J. Prim. Health Care 9 (1991) 83–7.
A. Krasnik, P.P. Groenewegen, P.P. Pedersen, P. v.Scholten, G. Mooney, A. Gottschau, H.A. Flierman and M.T. Damsgaard, Changing remuneration systems: effects on activity in general practice, Br. Med. J. 300 (1990) 1698–701.
A. LaRue, L. Bank, L. Jarvik and M. Hetland, Health in old age: how do physician ratings and self-ratings compare?, J. Gerontol. 14 (1979) 687–91.
K.-L. Liaw, S.A. Wort and M.V. Hayes, Intra-urban mortality variation and income disparity: a case study of Hamilton-Wentworth Region, Canadian Geographer 33 (1989) 131–45.
M.W. Linn, K.I. Hunter and B.S. Linn, Self-assessed health, impairment and disability in Anglo, black and Cuban elderly, Med. Care 18 (1980) 282–88.
B.S. Linn and M.W. Linn, Objective and self-assessed health in the old and very old, Social Science and Medicine 14A (1980) 311–15.
G.L. Maddox and E. Douglass, Self-assessment of health: a longitudinal study of elderly subjects, Journal of Health and Social Behaviour 14 (1973) 87–93.
A. Majeed, Allocating budgets for fundholding and prescribing: practice based needs assessment may be the only real answer, Br. Med. J. 313 (1996) 1274–5.
M.G. Marmot, M.J. Shipley and G. Rose, Inequalities in healthspecific explanations of a general pattern?, Lancet 1 (1984) 1003–6.
J. McCallum, B. Shadbolt and D. Wang, Self-rated health and survival: a 7-year follow-up study of Australian elderly, Am. J. Public Health 84 (1994) 1100–5.
J.M. Mossey and E. Shapiro, Self-rated health: a predictor of mortality among the elderly, Am. J. Public Health 72 (1982) 800–8.
S.Z. Nagi, An epidemiology of disability among adults in the United States, Millbank Memorial Fund Quarterly/Health and Society (Fall 1976) 439–67.
J. Nagy, Experiences with DRG based reimbursement in Hungary, in: Proceedings: European Public Health Association: Health Care Reforms in Central and Eastern Europe, December 14-16, 1995 (Department of Social Medicine, University Medical School, Debrecen, 1996) pp. 87–112.
E. Orosz, Main challenges for health policy in a period of socioeconomic transformation in Hungary, in: Health Care Reforms in Central and Eastern Europe, December 14-16, 1995 (University Medical School, Department of Social Medicine, Debrecen, 1996) pp. 113–23.
S. Radulescu, Key issues of health care reform in Romania, in: Proceedings: European Public Health Association: Health Care Reforms in Central and Eastern Europe, December 14-16, 1995 (University Medical School, Department of Social Medicine, Debrecen, 1996) pp. 125–9.
Resource Allocation Working Party, Sharing resources for health in England, Report of the Resource Allocation Working Party, HMSO, London (1976).
D. Rublee, European models of physician capitation, in: Primary Care Reform: A Strategy for Stability (Ontario Medical Association, Toronto, 1996).
Services Development and Planning Branch, Operations Division, A Resource Allocation Formula for the New South Wales Health System - 1993 Revision (New South Wales Department of Health, 1993).
T.A. Sheldon, P. Smith, M. Borowitz, S. Martin and R. Carr Hill, Attempt at deriving a formula for setting general practitioner fundholding budgets, Br. Med. J. 309 (1994) 1059–64.
Social Services Committee, Perinatal and Neonatal Mortality: Follow-up (HMSO, London, 1984).
Strategic Programs Branch, Introduction of Needs-Based Allocation of Resources to Saskatchewan District Health Boards for 1993-94 (Saskatchewan Health, Regina, 1994).
S. Syme and L. Berkman, Social class, susceptibility and sickness, in: The Sociology of Health and Illness, eds. P. Conrad and K. Kern (St. Martin's Press, New York, 1986).
T. Tissue, Another look at self-rated health in the elderly, J. Gerontol. 27 (1972) 91–4.
P. Townsend, P. Phillimore and A. Beattie, Health and Deprivation (Routledge, London, 1988).
P. Townsend and N. Davidson, Inequalities in Health: the Black Report (Penguin, Harmondsworth, 1982).
I. Waldron, Why do women live longer than men?, in: The Sociology of Health and Illness, 2nd ed., eds. P. Conrad and R. Kern (St. Martin's Press, New York, 1986).
G. Wannamethee and A.G. Shaper, Self-assessment of health status and mortality in middle-aged British men, Int. J. Epidemiol. 20 (1991) 239–45.
D. Wigle and Y. Mao, Mortality by Income Level in Urban Canada (Health and Welfare Canada, Ottawa, 1980).
R. Wilkins, G.J. Sherman and P.A.F. Best, Birth outcomes and infant mortality by income in urban Canada, 1986, Health Reports 3 (1991) 7–31.
R. Wilkins, O. Adams and A. Brancker, Changes in mortality by income in urban Canada from 1971 to 1986, Health Reports 1 (1989) 137–74.
R. Wilkins and O. Adams, The Healthfulness of Life (Institute for Research in Public Policy, Montreal, 1983).
F.D. Wolinsky and R.J. Johnson, Perceived health status and mortality among older men and women, J. Gerontol. 47 (1992) S304–12.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hutchison, B., Hurley, J., Birch, S. et al. Needs-based primary medical care capitation: Development and evaluation of alternative approaches. Health Care Management Science 3, 89–99 (2000). https://doi.org/10.1023/A:1019093324371
Issue Date:
DOI: https://doi.org/10.1023/A:1019093324371