Abstract
Purpose: This study was initiated to determine the negative effect (cryodamage) on human spermatozoa after freeze–thawing and to find out whether freezing of spermatozoa with a computerized biological freezer is more advantageous than freezing above static liquid nitrogen vapour with regard to spermatozoa vitality, chromatin normality, morphology, and membrane integrity.
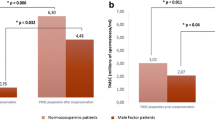
Methods: Forty-four semen samples were obtained from patients attending andrology laboratory, and each sample was divided into two aliquots. One aliquot was frozen using static liquid nitrogen vapour (G.II) and the second with a computerized biological freezer (G.III). Acridine orange was used for assessment of chromatin cryoinjury, whereas the morphology was evaluated according to WHO criteria. Hypo-osmotic swelling test was used to identify membrane integrity and eosin–nigrosin staining was used to determine the vitality of spermatozoa.
Results: The mean percentage of normally condensed chromatin in the native semen sample (G.I) decreased significantly (p < .001) after freeze–thawing by using either liquid nitrogen vapour (G.II), or a biological freezer (G.III), which was significantly higher (p < .001) after freezing with liquid nitrogen vapour than after freezing with the biological programmed freezer. Morphologically normal spermatozoa decreased significantly (p < .001) in both freezing methods in comparison to the native semen samples. In addition, membrane integrity of spermatozoa (HOS-test positive) was significantly lower (p < .001) after the freeze–thawing procedure in G.II and G.III compared to G.I. In both these parameters the deterioration was similar among the two freezing procedures. Finally the mean percentage of live spermatozoa decreased significantly (p < .001) in both freezing techniques in relation to the mean value in the neat semen samples.
Conclusions: Freeze–thawing procedure has a detrimental effect on chromatin, morphology, membrane integrity, and vitality of human spermatozoa not only by freezing above static liquid nitrogen vapour but even by using a computerized biological freezer. However, the chromatin deterioration rates are significantly higher by freezing above static liquid nitrogen vapour in comparison to freezing with a programmed biological freezer. Therefore, we recommend the use of this technique for freezing semen especially when ICSI technique is considered as the main therapeutic procedure.
Similar content being viewed by others
REFERENCES
Polge C, Smith AU, Parks AS: Survival of spermatozoa after vitrification and dehydration at low temperatures. Nature 1949;164:666-676
Farrant J: General principles of cell preservation. In Frozen Human Semen, DW Richardson, D Joce, EM Symond (eds), Boston, Martinus Nijhoff, 1980, p 6
Holt WV: Basic aspect of frozen storage of seme. Anim Reprod Sci 2000;62:3-22
Foote RH: Semen quality from the bull to the freezer: An assessment. Theriogenology 1975;4:219-235
Graham EG: Fundamentals of the preservation of spermatozoa. In The Integrity of Frozen Spermatozoa, Washington, DC, National Academy of Science, 1978, pp 4-44
Watson PF: The preservation of semen in mammals. In Oxford Review of Reproductive Biology, CA Finn (ed), London, Oxford University Press, 1979, pp 283-350
Mazur P: Equilibrium quasi-equilibrium and non equilibrium freezing of mammalian embryos. Cell Biophys 1990;17:53-92
Mazur P: Kinetics of water loss from cells at subzero temperatures and the likelihood of intracellular freezing. J Gen Physiol 1963;47:368
Farrant J: Mechanism of injury and protection in living cells and tissues at low temperaturees. In Current Trends in Cryobiology, AU Smith (ed), New York, Plenum, 1970, pp 139-152
Muldrew K, McGann LE: The osmotic rupture hypothesis of intracellular freezing injury. Biophys J 1994;66:532-541
Watson PF, Duncan AE: Effect of salts concentration and unfrozen water fraction on the viability of slowly frozen ram spermatozoa. Cryobiology 1988;25:131-142
Kincade RC, Colvin KL, Kleinhans FW, Critser ES, Mazur P, Critser JK: The effect of cooling rate and repeated freezing on human sperm cryosurvival. J Androl 1989;10(Suppl):48
Henry MA, Noiles EE, Gao DY, Mazur P, Critser JK: Cryopreservation of human spermatozoa. IV. The effect of cooling rate and warming rate on the maintenance of motility, plasma membrane integrity, and mitochondrial function. Fertil Steril 1993;60:911-918
Holt WV, North RD: Cryopreservation, actin localization and thermotropic phase transmsition inramspermatozoa. J Reprod Fertil 1991;91:451-461
Hammerstedt RH, Graham JK, Nolan JP: Cryopreservation of mammalian sperm: What we ask them to survive. J Androl 1990;11:73-88
Alvarez JG, Storey BT: Evidence of increased lipid peroxidative damage and loss of superoxide dismutase activity as amode of sublethal cryodamge to human sperm during cryopreservation. J Androl 1992;13:232-241
Crister JK, Arenson BW, Aaker DV, Huse-Benda AR, Ball GD: Cryopreservation of human spermatozoa. II. Postthaw chronology of motility and of zona-free hamster ova penetration. Fertil Steril 1987;47:980-984
Check ML, Check JH: Poor hypo-osmotic swelling test result from cryopreserved sperm despite preservation of sperm motility. Arch Androl 1991;26:37-41
Cross LN, Hanks SE: Effect of cryopreservationon human sperm acrosomes. Hum Reprod 1991;6:1279-1283
Hammadeh ME, Georg T, Rosenbaum P, Schmidt W: Association between freezing agent and acrosome damage of human spermatozoa from subnormal and normal semen. Andrologia; in press
Royere D, Barthelemy C, Hamamah S, Lansac J: Cryopreservation of spermatozoa: A review. Hum Reprod Update 1996;2:553-559
World Health Organisation (WHO): Laboratory Manual for the Examination of Human Semen and Semen-Cervical Mucus Interaction. Cambridge, UK, Cambridge University Press, 1999
Menkveld R, Stander FSH, Kotze TJW, Kruger TF, Van Zyl JA: The evaluation of morphologic characteristics of human spermatozoa according to strict criteria. Hum Reprod 1990;5:586-592
Tejada RI, Mitchell JC, Norman A, Marik JJ, Friedman S: A test for the practical evaluation of male fertility by acridine orange (AO) fluorescence. Fertil Steril 1984;42:87-91
Jeyendran RPS, Van der Ven HH, Perez-Palez M, Crabo BG, Zaneveld LJ: Development of an assay to assess the functional integrity of the human sperm membrane and its relationship to other semen characteristics. Reprod Fertil 1984;70:219-228
Eliasson R, Treich L: Supravital staining of human spermatozoa. Fertil Steril 1971;22:134
Dott HM, Foster GC: A technique for studying the morphology of mammalian spermatozoa which are eosinophilic in a differential life dead stain. J Reprod Fertil 1972;29:443
Centola GM, Raubertas RF, Mattox JH: Cryopreservation of human semen: Comparison of cryopreservation, sources of variability, and prediction of post-thaw survival. J Androl 1992;13:283-288
Sherman JK: Current status of clinical cryobanking of human sperm. In Andrology: Male Fertility and Sterility, JD Paulson, A Negrovilar, E Lucena, L Martinia (eds), New York, Academic Press, 1986, pp 517-549
McLaughlin EA, Ford WCL, Hull MGR: A comparison of the freezing semen in the uncerculated vapour above liquid nitrogen and in a commercial semi-programmable freezer. Hum Reprod 1990;5:728-734
Serafini PC, Hauser D, Moyer D, Marrs RP: Cryopreservation of human spermatozoa: Correlation of ultrastructural sperm head configuration with sperm motility and ability to penetrate zona free hamster ova. Fertil Steril 1986;46:691-695
Ragni G, Caccamo AM, Della Serra A, Guercilena S: Computerized slow-staged freezing of semen from men with testicular tumours or Hodgkin's disease preserves sperm better than standard vapour freezing. Fertil Steril 1990;53:1072-1075
Verheyen G, Pletinex I, Van Steirtegham A: Effect of freezing method, thawing temperature and post-thaw dilution/washing on motility ( CASA) and morphology characteristics of highquality human sperm. Hum Reprod 1993;8:1678-1684
Thachil JV, Jewett MS: Preservation techniques for human semen. Fertil Steril 1981;35:546
Wolf DP, Patton PE: Sperm cryopreservation: State of the art. J In Vitro Fertil Embryo Trans 1989;6:325-327
Check ML, Check JH, Long R: Detrimental effects of cryopreservation on structural and functional integrity of the sperm membrane. Arch Androl 1991;27:155-160
Spittaler PJ, Tylor JP: Further evaluation of a simple test for determining the integrity of spermatozoa membranes. Clin Reprod Fertil 1985;3:187-196
Chan SY, Craft IL, Chan YM, Leong MK, Leung CK: The hypoosmotic swelling test and cryosurvival of human spermatozoa. Hum Reprod 1990;5:715-718
Esteves SC, Sharma RK, Thomas AJR, Agrawal A: Suitability of the hypo-osmotic swelling test for assessing the viability of cryopreserved sperm. Fertil Steril 1996;66:798-804
Check ML, Check DJ, Katsoff JH: Improved results of thawed sperm cryopreserved with slow stage cooling with a cellevator. Arch Androl 1996;37:61-64
Royere D, Hamamah S, Nicolle JC, Barthelemy C, Lansac J: Freezing and thawing alter chromatin stability of ejaculated human spermatozoa: Fluorescence acridine orange staining and Feulgen-DNA cytophotometrics studies. Gamet Res 1988;21:51
Hamamah S, Royere D, Nicolle JC, Paquignon M, Lansac J: Effect of freezing on the spermatozoa nucleus: A comparative chromatin cytophotometric study in the porcine and human species. Reprod Nutr Dev 1990;30:59-64
Bach O, Glander HJ, Scholz G, Schwarz J: Elektrophoretic patterns of spermatozoal nucleoproteins (NP) in fertile men and infertile patients and comparison with NP of somatic cells. Andrologia 1990;22:217-224
Foresta C, Zorzi M, Rossato M, Varotto, A: Sperm nuclear instability and staining with aniline blue: Abnormal persistence of histones in spermatozoa in infertile men. Int J Androl 1992;15:330-337
Hammadeh ME, Askari A, Gerorg T, Rosenbaum P, Schmidt W: Effect of freeze-thawing procedure on chromatin stability, morphological alteration and membrane integrity of human spermatozoa in fertile and subfertile men. Int J Androl 1999;22:155-162
Nogueira D, Bourgain C, Verheyen G, Van Steirtegham AC. Light and electron microscopic analysis of human testicular spermatozoa and spermatids from frozen and thawed testicular biopsies. Hum Reprod 1999;14:2041-2049
Barthelemy C, Royere D, Hammamah S, Lebos C, Tharanne MJ, Lansac J: Ultrastructure changes in membrane and acrosomes of human sperm during cryopreservation. Arch Androl 1990;25:29-40
Royere D, Hamamah S, Nicolle JC, Lansac J: Chromatin alterations induced by freeze-thawing influence the fertilizing ability of human sperm. Int J Androl 1991;14:328-332
Ohsako S, Nagano R, Sugimoto Y, Goto, K: Comparison of the nuclear DNA stability against freezing-thawing and high temperature treatments between spermatozoa and somatic cells. Vet Med Sci 1997;59:1085-1088
Pederson H, Lebech PE: Ultrastructure changes in the human spermatozoon after freezing for artificial insemination. Fertil Steril 1971;22:125-133
Keel BA, Webster BW, Roberts DK: Effect of cryopreservation on the motility characteristics of human spermatozoa. J Reprod Fertil 1987;81:213-220
Mahadevan M, Trounson AO: Effect of cooling, freezing and thawing rates and storage conditions on preservation of human spermatozoa. Andrologia 1984;16:52-60
McLaughlin EA, Ford WC, Hull MG: The contribution of the toxicity of a glycerol-egg yolk-citrate cryopreservative to the decline in human sperm motility during cryopreservation. J Reprod Fertil 1992;95:749-754
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hammadeh, M.E., Szarvasy, D., Zeginiadou, T. et al. Andrology: Evaluation of Cryoinjury of Spermatozoa After Slow (Programmed Biological Freezer) or Rapid (Liquid Nitrogen Vapour) Freeze–Thawing Techniques. J Assist Reprod Genet 18, 364–370 (2001). https://doi.org/10.1023/A:1016666221500
Issue Date:
DOI: https://doi.org/10.1023/A:1016666221500