Abstract
Purpose. This investigation determines the drug delivery capacity of Lipospheres, which are drug-containing solid-filled vesicles made of triglyceride with a phospholipid outer covering, to release local anesthetic in vitro and to produce sustained peripheral nerve block in vivo.
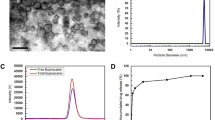
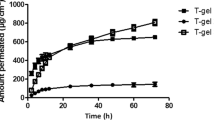
Methods. The local anesthetic, bupivacaine, was loaded into Lipospheres in several dosage forms, characterized, and measured for in vitrorelease. In rats, Lipospheres were administered into a large space between muscle layers surrounding the sciatic nerve to assess sensory and motor block in vivo.
Results. The particle size of Lipospheres was determined to be between 5 and 15 μm, with over 90% surface phospholopid. Lipospheres released bupivacaine over two days under ideal sink conditions. Liposphere nerve application produced dose-dependent and reversible block. Indeed, sustained local anesthetic block (SLAB) was observed for 1−3 days in various in vivo tests: a) Hind paw withdrawal latency to noxious heat was increased over 50% for 96 hr period after application of 3.6% or 5.6% bupivacaine-Lipospheres. The 3.6% and 5.6% doses were estimated to release bupivacaine at 200 and 311 μg drug/ hr, respectively, based on release spanning 72 hr. Application of 1.6% bupivacaine-Lipospheres increased withdraw latency 25−250% but for only a 24 hr duration; b) Similarly, vocalization threshold to hind paw stimulation was increased 25−50% for 72 hr following application of 3.6% bupivacaine-Lipospheres; c) Finally, sensory blockade outlasted or equaled corresponding motor block duration for all Liposphere drug dosages.
Conclusions. Liposphere delivery of local anesthetic drugs may be well suited for site-specific pharmacotherapy of neural tissue to produce SLAB. Dose-dependent effects in duration of action may include lipophilic tissue storage.
Similar content being viewed by others
REFERENCES
M. J. Cousins. The spinal route of analgesia for acute and chronic pain. In R. Dubner, G. F. Gebhart, and M. R. Bond (eds.), Proceedings of the 5th World Congress on Pain, Elsevier, Amersterdam, 1988, pp. 454–471.
D. B. Masters, C. B. Berde, S. Dutta, and R. Langer. Prolonged sciatic nerve blockade using sustained release of bupivacaine from a biodegradable polymer matrix. Anesthesiol. 75:A765 (1991).
D. B. Masters, C. B. Berde, J. M. Ward, J. A. J. Martyn, and W. J. Kupsky. Biochemical and histologic effects of prolonged sciatic nerve blockade with bupivacaine using a biodegradable polymer matrix. Anesthesiol. 75:A680 (1991).
D. B. Masters, C. B. Berde, S. Dutta, T. Turek, and R. Langer. Sustained local anesthetic release from bioerodible polymer matrices: a potential method for prolonged regional anesthesia. Pharm. Res. 10:1527–1532 (1993).
D. B. Masters, C. B. Berde, S. K. Dutta, C. T. Griggs, D. Hu, W. Kupsky, and R. Langer. Prolonged regional nerve blockade by controlled release of local anesthetic from a biodegradable polymer matrix. Anesthesiol. 79:340–346 (1993).
D. B. Masters and C. B. Berde. Drug delivery to peripheral nerves. In A. J. Domb (eds.), Polymer Site-Specific Pharmacotherapy, John Wiley & Sons Ltd., New York, 1994, pp. 443–455.
R. Langer. New methods of drug delivery. Science 249:1527–1533 (1990).
R. Langer. 1994 Whitaker Lecture: Polymers for drug delivery and tissue engineering. Ann. Biomed. Eng. 23:101–111 (1995).
N. Wakiyama, K. Juni, and M. Nakano. Preparation and evaluation in vitro and in vivo of polylactic acid microspheres containing dibucaine. Chem. Pharm. Bull. 30:3719–3727 (1982).
D. Haynes and A. Kirkpatrick. Ultra-long-duration local anesthesia produced by injection of lecithin-coated methoxyflurane microdroplets. Anesthesiol. 63:490–499 (1985).
L. Langerman, E. Golomb, and S. Benita. Spinal anesthesia: significant prolongation of the pharmacologic effect of tetracaine with lipid solution of the agent. Anesthesiol. 74:105–107 (1991).
T. Mashimo, I. Uchida, M. Pak, A. Shibata, S. Nishimura, Y. Inagaki, and I. Yoshiya. Prolongation of canine epidural anesthesia by liposome encapsulation of lidocaine. Anesth. Analg. 74:827–34 (1992).
A. J. Domb. Lipospheres for controlled delivery of substances. In US Patent 5,188,837, Feb. 1993.
M. J. Cousins and P. O. Bridenbaugh. In Neural Blockade. In (eds.), Neural Blockade in Clinical Anesthesia and Management of Pain, J. B. Lippincott, Philadelphia, 1988, pp. 121–128.
A. J. Domb and M. Maniar. Development of a novel parenteral drug delivery system: the Liposphere delivery system. In AAPS Meeting, Washington, D.C., 1991.
S. Amselem, C. R. Alving, and A. Domb. Polymeric biodegradable lipospheres as vaccine delivery systems. Polym. Adv. Technol. 3:351–357 (1992).
S. Amselem, A. J. Domb, and C. R. Alving. Lipospheres as a vaccine carrier system: effects of size, charge, and phospholipid composition. Vaccine Res. 1:383–395 (1992).
E. Hersh, M. Maniar, M. Green, and S. Cooper. Anesthetic activity of the lipospheres bupivacaine delivery system in the rat. Anesthes. Prog. 39:197–200 (1993).
A. J. Domb, L. Bergelson, and S. Amselem. Liposphere Delivery Systems. In S. Benita (ed.), Nanosphere Delivery Systems, Marcel Dekker, New York, 1996, p. 381.
R. R. C. New. Liposomes a practical approach. In Oxford Univ. Press, 1990.
N. Oku, D. A. Kendeall, and R. C. MacDonald. A simple procedure for the determination of the trapped volume of liposomes. Biochim. Biophy. A. 691:332–340 (1982).
J. G. Thalhammer, M. Vladimirova, M. S. E. E. Bershadsky, and G. R. Strichartz. Neurologic evaluation of the rat during sciatic nerve with lidocaine. Anesthesiol. 82:1013–1025 (1995).
C. Beyer, L. A. Roberts, and B. R. Komisaruk. Hyperalgesia induced by altered glycinergic activity at the spinal cord. Life Sci. 37:875–882 (1985).
D. B. Masters and B. R. Komisaruk. Neonatal capsaicin treatment attenuates sensory-induced analgesia and nociception. Physiol. Behav. 50:901–906 (1991).
Y. Barenholz, D. Gibbes, B. J. Litman, J. Goll, T. E. Thompson, and F. D. Carlson. A simple method for the preparation of homogenous phospholipid vesicles. Biochem. 16:2806–2810 (1977).
H. C. Powell, M. W. Kalichman, R. S. Garrett, and R. R. Myers. Selective vulnerability of unmyelinated fiber Schwann cells in nerves exposed to local anesthetics. Lab. Invest. 59:271–280 (1988).
D. H. Haynes, M. A. Kolber, and S. J. Morris. Short and long-range forces involved in cation-induced aggregation of chromaffin granule membranes. J. Theor. Biol. 81:713–743 (1985).
S. Reiz and S. Nath. Toxic effects of local anesthetic agents on the central nervous system. Br. J. Anesth. 58:732–735 (1986).
D. B. Scott. Toxic effects of local anesthetic agents on the central nervous system. Br. J. Anesth. 58:732–735 (1986).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Masters, D.B., Domb, A.J. Liposphere Local Anesthetic Timed-Release for Perineural Site Application. Pharm Res 15, 1038–1045 (1998). https://doi.org/10.1023/A:1011978010724
Issue Date:
DOI: https://doi.org/10.1023/A:1011978010724