Abstract
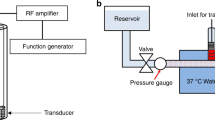
Background: In vitro studies showed that low-frequency ultrasound (US) causes blood clot dissolution. This effect is augmented with thrombolytics, microbubbles and microparticles. However, in animal models of transcutaneous delivery, US alone is not effective, probably due to attenuation of US energy by overlying skin. When combined with thrombolytics or microbubbles, transcutaneous US is highly effective. Purpose: To assess the synergistic effect of low-intensity low-frequency US and saline, hydroxyethyl starch (HAES) (a non-gas filled microparticle containing solution), streptokinase (STK), and their combination on blood clot disruption. Methods: Human blood clots from 4 healthy donors, 2–4 hours old, were immersed for 0, 15, or 30 min in 37°C in 10 ml of the above-mentioned solutions, and then were randomized to 10 sec of 20 kHz US or no US. The % difference in weight was calculated. Results: Immersion for 30 min without US resulted in 13.8 ± 1.2% clot lysis in saline, and 22.0 ± 1.3%, 21.7 ± 2.1%, and 23.2 ± 1.9% in STK, HAES, and STK + HAES, respectively (p = 0.002). US augmented clot lysis in all groups and at all time points. With low-intensity US, HAES was not better than saline. However, the combination of HAES + STK with US resulted in larger clot disruption at 15 sec incubation time (46.7 ± 3.2%) than with saline (29.6 ± 2.1%), HAES (29.6 ± 2.5%), and STK (32.8 ± 3.6%) (p < 0.001). Conclusion: low-frequency, low-intensity US combined with HAES and STK resulted in greater clot disruption at short incubation times. This combination may assist in achieving faster reperfusion in in vivo models.
Similar content being viewed by others
References
Rosenschein U, Bernstein JJ, DiSegni E, Kaplinsky E, Bernheim J, Rozenzsajn LA. Experimental ultrasonic angioplasty: Disruption of atherosclerotic plaques and thrombi in vitroand arterial recanalization in vivo.J Am Coll Cardiol 1990; 15: 711-17.
Hong AS, Chae JS, Dubin SB, Lee S, Fishbein MC, Siegel RJ. Ultrasonic clot disruption: An in vitrostudy. Am Heart J 1990; 120:4 18-22.
Ariani M, Fishbein MC, Chae JS, et al. Dissolution of peripheral arterial thrombi by ultrasound. Circulation 1991; 84: 1680-88.
Sehgal CM, Leveen RF, Shlansky-Goldberg RD. Ultrasound-assisted thrombolysis. Invest Radiol 1993; 28:9 39-43.
Porter TR, Le Veen RF, Fox R, Kricsfeld A, Xie F. Thrombolytic enhancement with perfluorocarbon-exposed sonicated dextrose albumin microbubbles. Am Heart J 1996; 132: 964-68.
Kondo I, Mizushige K, Ueda T, Masugata H, Ohmori K, Matsuo H. Histological observations and the process of ultrasound contrast agent enhancement of tissue plasminogen activator thrombolysis with ultrasound exposure. Jpn Circ J 1999; 63: 478-84.
Birnbaum Y, Atar S, Luo H, Nagai T, Siegel RJ. Ultrasound has synergistic effects in vitrowith tirofiban and heparin for thrombus dissolution. Thromb Res 1999; 96:4 51-58.
Birnbaum Y, lakobishvili Z, Porter A, et al. Microparticlecontaining oncotic solutions augment in vitroclot disruption by ultrasound. Thromb Research 2000; 98:5 49-57.
Luo H, Steffen W, Cercek B, Arunasalam S, Maurer G, Siegel RJ. Enhancement of thrombolysis by external ultrasound. Am Heart J 1993; 125:15 64-69.
Kimura M, Iijima S, Kobayashi K, Furuhata H. Evaluation of the thrombolytic effect of tissue-type plasminogen activator with ultrasonic irradiation: In vitroexperiment involving assay of the fibrin degradation products from the clot. Biol Pharm Bull 1994; 17:1 26-30.
Harpaz D, Chen X, Francis CW, Meltzer RS. Ultrasound accelerates urokinase-induced thrombolysis and reperfusion. Am Heart J 1994; 127:12 11-19.
Kornowski R, Meltzer RS, Chernine A, Vered Z, Battler A. Does external ultrasound accelerate thrombolysis? Results from a rabbit model. Circulation 1994; 89:3 39-44.
Olsson SB, Johansson B, Nilsson AM, Olsson C, Roijer A. Enhancement of thrombolysis by ultrasound. Ultrasound Med Biol 1994; 20:3 75-82.
Luo H, Birnbaum Y, Fishbein MC, et al. Enhancement of thrombolysis in vivowithout skin and soft tissue damage by transcutaneous ultrasound. Thromb Res 1998; 89:1 71-77.
Luo H, Nishioka T, Fishbein MC, et al. Transcutaneous ultrasound augments lysis of arterial thrombi in vivo.Circulation 1996; 94:7 75-78.
Riggs PN, Francis CW, Bartos SR, Penney DP. Ultrasound enhancement of rabbit femoral artery thrombolysis. Cardiovasc Surg 1997; 5:2 01-07.
Francis CW, Blinc A, Lee S, Cox C. Ultrasound accelerates transport of recombinant tissue plasminogen activator into clots. Ultrasound Med Biol 1995; 21:4 19-24.
Akiyama M, Ishibashi T, Yamada T, Furuhata H. Lowfrequency ultrasound penetrates the cranium and enhances thrombolysis in vitro.Neurosurgery 1998; 43: 828-832; discussion 832-33.
Larsson J, Carlson J, Olsson SB. Ultrasound enhanced thrombolysis in experimental retinal vein occlusion in the rabbit. Br J Ophthalmol 1998; 82:14 38-40.
Tachibana K, Tachibana S. Albumin microbubble echocontrast material as an enhancer for ultrasound accelerated thrombolysis. Circulation 1995; 92:11 48-50.
Nishioka T, Luo H, Fishbein MC, et al. Dissolution of thrombotic arterial occlution by high intensity low frequency ultrasound and dodecafluoropentane emulsion: In vitroand in vivostudy. Am Coll Cardiol 1997; 30: 561-68.
Birnbaum Y, Luo H, Nagai T, et al. Noninvasive in vivoclot dissolution without a thrombolytic drug: Recanalization of thrombosed iliofemoral arteries by transcutaneous ultrasound combined with intravenous infusion of microbubbles. Circulation 1998; 97:1 30-34.
Rosenschein U, Roth A, Rassin T, Basan S, Laniado S, Miller HI. Analysis of coronary ultrasound thrombolysis endpoints in acute myocardial infarction (ACUTE trial). Results of the feasibility phase. Circulation 1997; 95: 1411-16.
Hamm CW, Steffen W, Terres W, et al. Intravascular therapeutic ultrasound thrombolysis in acute myocardial infarctions. Am J Cardiol 1997; 80: 200-04.
Rosenschein U, Gaul G, Erbel R, et al. Percutaneous transluminal therapy of occluded saphenous vein grafts: Can the challenge be met with ultrasound thrombolysis? Circulation 1999; 99: 26-29.
Siegel RJ, Cumberland DC, Myler RK, Belli A, DonMichael TA. Percutaneous peripheral ultrasonic angioplasty. Herz 1990; 15: 329-34.
Rosenschein U, Rozenszajn LA, Kraus L, et al. Ultrasonic angioplasty in totally occluded peripheral arteries. Initial clinical, histological, and angiographic results. Circulation 1991; 83:19 76-86.
Lauer CG, Burge R, Tang DB, Bass BG, Gomez ER, Alving BM. Effect of ultrasound on tissue-type plasminogen activator-induced thrombolysis. Circulation 1992; 86:12 57-64.
Siegel R, Atar S, Fishbein MC, et al. Noninvasive transthoracic low frequency ultrasound augments thrombolysis in a canine model of acute myocardial infarction. Circulation 2000; 101:20 26-29.
Lincoff AM, Topol EJ. Illusion of reperfusion: Does anyone achieve optimal reperfusion during acute myocardial infarction? Circulation 1993; 88:13 61-74.
Hensel M, Wrobel R, Volk T, Pahlig H, Kox WJ. Changes in coagulation physiology and rheology after preoperative normovolemic hemodilution. Anasthesiol Intensivmed Notfallmed Schmerzther 1996; 31: 481-87.
Munsch CM, MacIntyre E, Machin SJ, Mackie IJ, Treasure T. Hydroxyethyl starch: An alternative to plasma for postoperative volume expansion after cardiac surgery. Br J Surg 1988; 75:6 75-78.
Claes Y, Van Hemelrijck J, Van Gerven M, et al. Influence of hydroxyethyl starch on coagulation in patients during the perioperative period. Anesth Analg 1992; 75: 24-30.
Boldt J, Muller M, Heesen M, Heyn O, Hempelmann G. Influence of different volume therapies on platelet function in the critically ill. Intensive Care Med 1996; 22:10 75-81.
Blaicher AM, Reiter WJ, Blaicher W, et al. The effect of hydroxyethyl starch on platelet aggregation in vitro.Anesth Analg 1998; 86:13 18-21.
Kapiotis S, Quehenberger P, Eichler HG, et al. Effect of hydroxyethyl starch on the activity of blood coagulation and fibrinolysis in healthy volunteers: Comparison with albumin. Crit Care Med 1994; 22:6 06-12.
Strauss Rg. Review of the effects of hydroxyethyl starch on the blood coagulation system. Transfusion 1981; 21:2 99-02.
Treib J, Haass A, Pindur G, Treib W, Wenzel E, Schimrigk K. Influence of intravascular molecular weight of hydroxyethyl starch on platelets. Eur J Haematol 1996; 56:1 68-72.
Vogt NH, Bothner U, Lerch G, Lindner KH, Georgieff M. Large-dose administration of 6% hydroxyethyl starch 200/0.5 total hip arthroplasty: Plasma homeostasis, hemostasis, and renal function compared to use of5%human albumin. Anesth Analg 1996; 83:2 62-68.
Ota T, Hillman ND, Craig D, Kisslo J, Smith PK. Contrast echocardiography: Influence of ultrasonic machine settings, mixing conditions, and pressurization on pixel intensity and microsphere size of Albunex solution in vitro.J Am Soc Echocardiogr 1997; 10: 31-40.
Vandenberg BF, Melton HE. Acoustic lability of albumin microspheres. J Am Soc Echocardiogr 1994; 7:5 82-89.
Wu J, Tong J. Experimental study of stability of a contrast agent in an ultrasound field. Ultrasound Med Biol 1998; 24:2 57-65.
Jamnicki M, Zollinger A, Seifert B, Popovic D, Pasch T, Spahn DR. Compromised blood coagulation: An in vitrocomparison of hydroxyethyl starch 130/0.4 and hydroxyethyl starch 200/0.5 using thrombelastography. Anesth Analg 1998; 87:9 89-93.
Langer R, Jordan U, Wolfle A, Henrich HA. Action of hydroxyethyl starch (HES) on the activity of plasmatic clotting factors. Clin Hemorheol Microcirc 1998; 18:1 03-16.
Tobias MD, Wambold D, Pilla MA, Greer F. Differential effects of serial hemodilution with hydroxyethyl starch, albumin, and 0.9% saline on whole blood coagulation. J Clin Anesth 1998; 10:3 66-71.
Conroy JM, Fishman RL, Reeves ST, Pinosky ML, Lazarchick J. The effects of desmopressin and 6% hydroxyethyl starch on factor VIII:C. Anesth Analg 1996; 83: 804-07.
Farrugia A, Griffin B, Pepper D, Prowse C. Studies on the procurement of coagulation factor VIII: Selective precipitation of factor VIII with hydrophilic polymers. Thromb Haemost 1984; 51:3 38-42.
Sanfelippo MJ, Suberviola PD, Geimer NF. Development of a von Willebrand-like syndrome after prolonged use of hydroxyethyl starch. Am J Clin Pathol 1987; 88: 653-55.
Stump DC, Strauss RG, Henriksen RA, Petersen RE, Saunders R. Effects of hydroxyethyl starch on blood coagulation, particularly factor VIII. Transfusion 1985; 25: 349-54.
Lazarchick J, Conroy JM. The effect of 6% hydroxyethyl starch and desmopressin infusion on von Willebrand factor: Ristocetin cofactor activity. Ann Clin Lab Sci 1995; 25:3 06-09.
Dalrymple-Hay M, Aitchison R, Collins P, Sekhar M, Colvin B. Hydroxyethyl starch induced acquired von Willebrand's disease. Clin Lab Haematol 1992; 14: 209-11.
Egli GA, Zollinger A, Seifert B, Popovic D, Pasch T, Spahn DR. Effect of progressive haemodilution with hydroxyethyl starch, gelatin and albumin on blood coagulation. Br J Anaesth 1997; 78: 684-89.
Treib J, Haass A, Pindur G. Coagulation disorders caused by hydroxyethyl starch. Thromb Haemost 1997; 78: 974-83.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Adler, Y., Attar, D., Vaturi, M. et al. The Effects of Streptokinase and Hydroxyethyl Starch on in vitro Clot Disruption by Ultrasound. Cardiovasc Drugs Ther 15, 119–123 (2001). https://doi.org/10.1023/A:1011166711358
Issue Date:
DOI: https://doi.org/10.1023/A:1011166711358