Abstract
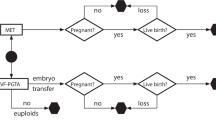
Purpose: To assess the influence of the presence of qualitysupernumerary embryos on the clinical outcome and risk ofmultiple conception in patients having their first in vitrofertilization (IVF) cycle.
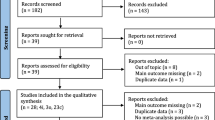
Methods: Retrospective cohort study of 1448 women havingtheir first IVF treatment cycle who received 4004 embryoswhere at least six embryos were available for transfer treatedin an Assisted Conception Unit based in a large teachinghospital.
Results: The replacement of three rather than two embryos towomen under 35 years who had good-quality supernumeraryembryos resulted in a higher twin (12.5 vs. 11.9%) and tripletbirth rates (2.1 vs. 0%), without significantly improving theclinical pregnancy (50.5 vs. 45.2%) or total live birth rates(38.9 vs. 35.7%). In the absence of quality spare embryos,these women who had three rather than two embryosreplaced had a significantly higher clinical pregnancy rate(39.3 vs. 28.8%; P = 0.04), total live birth (32.7 vs. 19.4%;P = 0.02) and singleton birth rate per cycle (20.8 vs. 14.4%;P = 0.04), without significantly influencing the multiplebirth rate. In women over 35 years, the replacement of threeinstead of two embryos in the presence or absence of qualitysupernumerary embryos led to a significant improvement inclinical outcome, without being associated with a concurrentincrease in the multiple birth rate. Women in both age groupswho had either two or three embryos replaced in the presenceof quality supernumerary embryos had a notably better clinicaloutcome compared with their counterparts who had thesame number of embryos replaced, but with no qualityembryos to spare.
Conclusions: The presence of good-quality supernumeraryembryos can be used as a reference to determine the optimalnumber of embryos to transfer and as an indicator of theprobability of success of an individual couple in a givencycle. Optimal pregnancy rates and simultaneous reductionof multiple gestation can be achieved with a flexible embryoreplacement policy that is based on embryo quality, maternalage, and the presence or absence of surplus quality embryos.
Similar content being viewed by others
REFERENCES
Levene MI, Wild J, Steer P: Higher order births and the modern management of infertility in Britain. Br J Obstet Gynaecol 1992;99:607–613
Tuppin P, Blondel B, Kaminiski M: Trends in multiple deliveries and infertility treatments in France. Br J Obstet Gynaecol 1993;100:383–385
Callahan TL, Hall JE, Ettner SL, Christiansen CL, Greene MF, Crowley WF: The economic impact of multiple-gestation pregnancies and the contribution of assisted-reproduction techniques to their incidence. N Engl J Med 1994;331:244–249
Seoud MA, Toner JP, Kruithoff C, Muasher SJ: Outcome of twin, triplet and quadruplet in vitro fertilisation pregnancies: the Norfolk experience. Fertil Steril 1992;57:825–834
Lipitz S, Reichman B, Uval J, Shalev J, Archiron R, Barkai G: A prospective comparison of the outcome of triplet pregnancies managed expectantly or by mutifetal reduction to twins. Am J Obstet Gynecol 1994;170:874–879
Sassoon DA, Castro LC, Davis JL, Hobel CJ: Perinatal outcome in triplets versus twin gestation. Obstet Gynecol 1990;75:817–820
Yokoyama Y, Shimizu T, Hayakawa K: Incidence of handicaps in multiple births and associated factors. Acta Genet Med Gemellol 1995;44:81–91
Yokoyama Y, Shimizu T, Hayakawa K: Prevalence of cerebral palsy in twins, triplets and quadruplets. Int J Epidemiol 1995;24:943–948
Vauthier-Brouzes D, Lefébvre G: Selective reduction in multifetal pregnancies: Technical and psychological aspects. Fertil Steril 1992;57:1012–1016
Goldfarb JM, Austin C, Lisbona H, Peskin B, Clapp M: Cost-effectiveness of in-vitro fertilisation. Obstet Gynecol 1996;87:18–21
Waterstone J, Parsons J, Bolton V: Elective transfer of two embryos. Lancet 1991;I:975–
Staessen C, Janssenswillen C, Van Den Abbeel E, Devroey P, Van Steirteghem AC: Avoidance of triplet pregnancies by elective transfer of two good quality embryos. Hum Reprod 1993;8:1650–1653
Staessen C, Nagy ZPM, Lui J: One year's experience with elective transfer of two good quality embryos in the human in-vitro fertilisation and intracytoplasmic sperm injection programmes. Hum Reprod 1995;10:3305–3312
Tasdemir M, Tasdemir I, Kodama H, Fukuda J, Tanaka T: Two instead of three embryo transfer in in-vitro fertilisation. Hum Reprod 1995;10:2155–2158
Roest J, Van Heusden AM, Verhoeff A, Mous HVH, Zeilmaker GH: A triplet pregnancy after in-vitro fertilisation is a procedure-related complication that should be prevented by replacement of two embryos only. Fertil Steril 1997;67:290–295
Matson PL, Browne J, Deakin R, Bellinge B: The transfer of two embryos instead of three to reduce the rate of multiple pregnancy: a retrospective analysis. J Assist Reprod Genet 1999;16:1–5
Human Fertilisation and Embryology Authority Sixth Annual Report 1997. HFEA, London, UK
Society for Assisted Reproductive Technology (SART), American Society for Reproductive Medicine (ASRM). Assisted reproduction technology in the United States and Canada: 1993 results generated from the American Society for Reproductive Medicine/Society for Assisted Reproductive Technology Registry. Fertil Steril 1995;64:13–21
Bollen N, Camus M, Tournaye H, Wisanto, A, Van Steirteghem AC, Devroey, P: Embryo reduction in triplet pregnancies after assisted procreation: a comparative study. Fertil Steril 1993;60:504–509
Berkowitz RL, Lynch L, Stone J, Alvarez M: The current status of multifetal pregnancy reduction. Am J Obstet Gynecol 1996;174:1265–1272
Widra EA, Gindoff PR, Smotrich DB, Stillman RJ: Achieving multiple-order embryo transfer identifies women over 40 years of age with improved in-vitro fertilisation outcome. Fertil Steril 1996;65:103–108
Wood C, McMaster R, Rennie G, Trounson A, Leeton J: Factors influencing pregnancy rates following in-vitro fertilisation and embryo transfer. Fertil Steril 1985;43:245–250
Check JH, Nowroozi K, De Cooman S, Thomas K: Influence of endometrial thickness and echo patterns on pregnancy rates during in-vitro fertilisation. Fertil Steril 1991;56:1173–1175
Paulson RJ, Sauer MV, Lobo RA: Embryo implantation after human in vitro fertilisation: Importance of endometrial receptivity. Fertil Steril 1990;53:870–874
Copperman AB, Selick CE, Grunfeld L, Sandler B, Bustillo M: Cumulative number and morphological score of embryos resulting in success: Realistic expectations from in-vitro fertilisation-embryo transfer. Fertil Steril 1995;64:88–92
Roseboom TJ, Vermeiden JW, Schoute E, Lens JW, Schats R: The probability of pregnancy after embryo transfer is affected by the age of the patient, cause of infertility, number of embryos transferred and the average morphology score, as revealed by multiple logistic regression analysis. Hum Reprod 1995;10:3035–3041
Salha O, Nugent D, Dada T, Kaufmann S, Levett S, Jenner L, Lui S, Sharma V. The relationship between follicular fluid aspirate volume and oocyte maturity in in-vitro fertilisation cycles. Hum Reprod 1998;13:1901–1906
Collins JA, Bustillo M, Visscher RD, Lawrence LD: An estimate of the cost of in-vitro fertilisation in the United States in 1995. Fertil Steril 1995;64:538–545
Templeton A, Morris JK: Reducing the risk of multiple births by transfer of two embryos after in-vitro fertilisation. N Engl J Med 1998;339:573–577
Bronson R: How should the number of embryos transferred to the uterus following in-vitro fertilisation be determined to avoid the risk of multiple gestation? Hum Reprod 1997;12:1605–1607
Faber K: IVF in the US: Multiple gestation, economic competition, and the necessity of excess. Hum Reprod 1997;12:1614–1616
Murdoch A: Triplets and embryo transfer policy. Hum Reprod 1997;12(Suppl 2):88–92
Hill AG, Freeman M, Bastias MC, Rogers BC, Herbert CM, Osteen KG, Wentz AC: The influence of oocyte maturity and embryo quality on pregnancy rate in a program for in-vitro fertilisation-embryo transfer. Fertil Steril 1989;52:801–806
Claman P, Armant RD, Seibel MM, Wang TN, Oskowitz SP, Taymor ML: The impact of embryo quality and quantity on implantation and establishment of viable pregnancies. J Vitro Fertil Embryo Transfer 1987;4:218–222
Puissant F, Rysselberge MV, Barlow P, Deweze J, Leroy F: Embryo scoring as a prognostic tool in IVF treatment. Hum Reprod 1987;2:705–708
Leese HJ, Hoope MAK, Edwards RG, Smith AMJ: Uptake of pyruvate by early human embryos determined by a non-invasive technique. Hum Reprod 1986;1:181–
Magnuson C, Hillenjo T, Homberger L, Nilson L: Oxygen consumption by human oocyte and balstocysts grown in vitro. Hum Reprod 1986;1:183–
Munné S, Alikani M, Tomkin G, Grifo J, Cohen J: Embryo morphology, developmental rates, and maternal age are correlated with chromosome abnormalities. Fertil Steril 1995;64:382–391
Hu Y, Maxson W, Hoffman D, Ory S, Eager S, Dupre J, Lu C: Maximising pregnancy rates and limiting higher-order multiple conceptions by determining the optimal number of embryos to transfer based on quality. Fertil Steril 1998;69:650–657
Sakkas D, Shoukir Y, Chardonnens D, Bianchi PG, Campana A: Early cleavage of human embryos to the two-cell stage after intracytoplasmic sperm injection as an indicator of embryo viability. Hum Reprod 1998;13:182–187
Shulman A, Ben-Nun I, Ghetler Y, Kaneti H, Shilon M, Beyth, Y: Relationship between embryo morphology and implantation rate after in vitro fertilisation treatment in conception cycles. Fertil Steril 1993;60:123–126
Medical Research International, Society for Assisted Reproductive Technology (SART), The American Fertility Society. In-vitro fertilisation-embryo transfer (IVF-ET) in the United States: 1990 results from the IVF-ET Registry. Fertil Steril 1992;57:15–24
Seibel, MM, Ranoux C, Kearnan M: In-vitro fertilisation: how much is enough. N Engl J Med 1989;321:1052–1053
Svendsen T, Jones D, Butler L, Muasher S: The incidence of multiple gestations after in vitro fertilisation is dependent on the number of embryos transferred and maternal age. Fertil Steril 1996;65:561–565
Van Os H C, Alberda ATh, Janssen-Caspers HAB, Leerentveld RA, Scholtes MCW, Zeilmaker GH: The influence of the interval between in-vitro fertilisation and embryo transfer and some other variables on treatment outcome. Fertil Steril 1989;51:360–362
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Salha, O., Dada, T., Levett, S. et al. The Influence of Supernumerary Embryos on the Clinical Outcome of IVF Cycles. J Assist Reprod Genet 17, 335–343 (2000). https://doi.org/10.1023/A:1009457112230
Issue Date:
DOI: https://doi.org/10.1023/A:1009457112230