Abstract
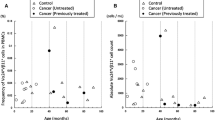
Adoptive immunotherapy using MHC-nonrestricted-lymphocytes, peripheral blood γδT cells and NK cells was devised. Peripheral blood mononuclear cells (3 x 107) were selected by immobilization to anti-CD3 monoclonal antibody for 4 days and cultured for 2 weeks in the presence of IL-2. Thereafter they were reactivated by 500 U/ml of IFN-α and 1000 U/ml of IL-2 for 1 hour. Enhancement of NK and LAK activities was confirmed. Peripheral blood γδT cells proliferated in response to immobilized anti-CD3 antibody (3% to 30%). Approximately 6 x 109 BRM-activated killer (BAK) cells composed of CD56+ γδT cells and CD56+ NK cells, were dispensed to cancer patients via intravenous drip infusion. Nine patients were treated with BAK cells every 2 weeks or every month on an outpatient basis. During the course of adoptive immunotherapy, the crossed affinity immunoelectrophoresis (CAIE) pattern of serum immunosuppressive acidic protein (IAP) was analysed. Both the production and glycosylation pattern of IAP is changed in response to tumor enlargement and may therefore act as a marker of the disease progression. During the course of BAK therapy, the glycosylation IAP pattern of 6 patients changed from tumor (T) to normal (N). In addition, the performance status of all patients was maintained at 90–100% of the Karnofsky scale and any side effects including fever were not observed during treatments with BAK cells. Moreover, the overall quality of life (QOL) of the patients, scored at the Face scale was favorable. In addition, blood levels of activated γδT cells producing IFN-γ were assayed as an indication marker of BAK therapy. The normal range of IFN-γ producing γδT cells comprised 6.9 ± 0.9% of peripheral blood mononuclear cells (PBMC), according to a single cell FACScan analyses of PBMCs derived from normal individuals. IFN-γ producing γδT cells of Patients No. 8 and 9, who received extensive chemotherapy before initiation of BAK therapy, comprised only 0.2% and 2% of PBMC, respectively. These patients died 3 and 6 months after beginning BAK therapy. Peripheral blood γδT cells of Patients Nos. 1–7 proliferated in response to immobilized anti-CD3 antibody and the frequency of IFN-γ producing γδT cells in PBMC preparation of these patients were over 3% before initiation of BAK therapy. Since our data show a positive correlation between survival time and initial γδT cell counts, a low frequency of these cells may contraindicate BAK therapy.
Similar content being viewed by others
References
Lorish CD, Maisiak R. The Face Scale: a brief, nonverbal method for assessing patient mood. Arthritis and Rheumatism 1986; 29: 906–9.
Rosenberg SA. An immunotherapy of cancer using interleukin-2. Immunology Today 1988; 9: 58–62.
Fisher B, Packard BS, Read EJ, Carrasquillo JA, Carter CS, Topalian SL, Yang JC, Yolles P, Larson SM, Rosenberg SA. Tumor localization of adoptively transferred indium-111 la-beled tumor infiltrating lymphocytes in patients with metasta-tic melanoma. J Clin Oncol 1989; 7: 250–61.
Belldegrun A, Kasid A, Uppenkamp M, Topalian SL, Rosen-berg SA. Human tumor infiltrating lymphocytes, Analysis of lymphokine mRNA expression and relevance to cancer immunotherapy. J Immunol 1989; 142: 4520–6.
Ioannides CG, Freedman RS, Platsoucas CD, Rashed S, Kim YP. Cytotoxic T cell clones isolated from ovarian tumor-infiltrating lymphocytes recognize multiple antigenic epitopes on autologus tumor cells. J Immunol 1991; 146: 1700–7.
Maeda N, Hamasato S, Miyazawa H, Takata M, Yamamoto H, Fujimoto S. Augmentation of human cytotoxic T lymphocytes against autologous tumor by a factor released from human monocytic leukemia cell line. Jpn J Cancer Res 1989; 80: 537–45.
Karnofsky DA, Abelmann WH, Craver LF, Burchenal JH. The use of the nitrogen mustards in the palliative treatment of carcinoma. Cancer 1948; 1: 634–56.
Haas W, Pereira P, Tonegawa S. γ /δ_cells. Annu Rev Immunol 1993; 11: 673–86.
Brenner MB, McLean J, Dialynas DP, Strominger JL, Smith JA, Owen FL, Seidman JG, Ip S, Rosen F, Krangel MS. Iden-tification of a putative second T-cell receptor. Nature 1986; 322: 145–59.
Mombaerts P, Mizoguchi E, Ljunggren H-G, Iacomini J, Ishikawa H, Wang L, Grusby MJ, Glimcher LH, Winn HJ, Bhan AK, Tonegawa S. Peripheral lymphoid development and function in TCR mutant mice. Int Immunol 1994; 6: 1061–70.
Fujimiya Y, Suzuki Y, Katakura R, Miyagi T, Yamaguchi T, Yoshimoto T, Ebina T. In vitrointerleukin 12 activation of peripheral blood CD3±CD56± and CD3±CD56−γ δ T cells from glioblastoma patients. Clin Cancer Res 1997; 3: 633–43.
Naume B, Nonstad U, Steinkjer B, Funderud S, Smeland E, Espevik T. Immunomagnetic isolation of NK and LAK cells. J Immunological Methods 1996; 136: 1–9.
Yamaguchi T, Fujimiya Y, Suzuki Y, Katakura R, Ebina T. A simple method for the propagation and purification of γ δT cells from the peripheral blood of glioblastoma patients using solid-phase anti-CD3 antibody and soluble IL-2. J Immuno-logical Methods 1997; 205: 19–28.
. Tamura K, Shibata Y, Matsuda Y, Ishida N. Isolation and characterization of an immunosuppressive acidic protein from ascitic fluids of cancer patients. Cancer Research 1981; 41: 3244–52.
Hansen S, Iversen J, Lihme A, Bog-Hanse L. Acute phase reaction, heterogeneity, and microheterogeneity of serum pro-teins as nonspecific tumor markers in lung cancer. Cancer 1987; 60: 1630–5.
16. Picker LJ, Shingh MK, Zdraveski Z, Treer JR, Waldrop SL, Bergstressor PR, Maino VC. Direct demonstration of cytokine synthesis heterogeneity among human menory/effector T cell by flow cytometry. Blood 1995; 86: 1408–19.
Sekine T, Shiraiwa H, Yamazaki T, Tobisu K, Kakizoe T. A feasible method for expansion of peripheral blood lym-phocytes by culture with immobilized anti-CD3 monoclonal antibody and interleukin-2 for use in adoptive immunotherapy of cancer patients. Biomed Pharmacother 1993; 47: 73–8.
Ochoa AC, Hasz DE, Rezonzew R, Anderson PM, Bach FH. Lymphokine-activated killer activity in long-term cultures with anti-CD3 plus interleukin 2: Identification and isolation of effector subsets. Cancer Res 1989; 49: 963–8.
Shibata Y, Tamura K, Ishida N. In vivoanalysis of the sup-pressive effects of immunosuppressive acidic protein, a type of alfa-1 acid glycoprotein, in connection with its high level in tumor-bearing mice. Cancer Res 1983; 43: 2889–96.
Ebina T, Murata K, Tamura K. Antitumor effect of intratu-moral administration of biological response modifiers: Induc-tion of immunosuppressive acidic protein, a type of α1-acid glycoprotein, in mice. Jpn J Cancer Res 1994; 85: 93–100.
Agneray J. Glycan microheterogeneity forms of alpha 1-acid glycoprotein (AGP). In: Alpha 1-Acid Glycoprotein: Genetics, Biochemistry, Physiological Functions, and Pharmacology, New York: Alan R. Liss, Inc., 1989; 47–65.
Yoshimura A, Niitani H, et al. Combined effects of PSK with chemotherapy in the treatment of adenocarcinoma of the lung, assessment of quality of life (QOL). Biotherapy 1992; 6: 256–7 (Japanese with English abstract).
Takeuchi K, Sato N, Kasahara H, Funayama N, Nagafuchi A, Yonemura S, Tsukita S, Tsukita S. Perturbation of cell adhe-sion and microbilli formation by antisense oligonucleotides to ERM family members. J Cell Biol. 1994; 125: 1371–84.
Rüegg C, Yilmaz A, Bieler G, Bamat J, Caubert P, Lejeune FJ. Evidence for the involvement of endothelial cell integrin αVβ3 by TNF and IFN-γ. Nature Med. 1998; 4: 408–14.
Saito M, Seki S, Hashimoto W, Ogasawara K, Kobayashi T, Kumagai K, Matsuno S, Takeda K. Cytotoxic γδ or _α β T cells with a natural killer cell marker, CD56, induced from human peripheral blood lymphocytes by a combination of IL-12 and IL-2. J Immunol 1996; 157: 3886–9
Antel JP, McCrea E, Ladiwala U, Qim Y, Becher B. Non-MHC-restricted cell-mediated lysis of human oligodendro-cytes in vitro: relation with CD56 expression. J. Immunol. 1998; 160: 1606–11.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ebina, T., Fujimiya, Y., Yamaguchi, T. et al. The use of BRM-activated killer cells in adoptive immunotherapy: A pilot study with nine advanced cancer patients. Biotherapy 11, 241–253 (1998). https://doi.org/10.1023/A:1008047628284
Issue Date:
DOI: https://doi.org/10.1023/A:1008047628284