Abstract
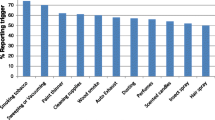
This epidemiological study evaluated respiratory histories in those individuals reporting chemical intolerance (CI) in a community population sample. The subsample of 181 completed standard Respiratory Health Questionnaires. CI was determined from self-ratings of feeling ‘moderately’ to ‘severly’ ill from exposure to at least three of five common chemicals (paint, pesticides, car exhaust, new carpet, and perfume); the prevalence rate was 22.7%. The comparison group (CN) (31.5% of the sample) were selected from their reports of ‘never’ feeling ill from the same chemicals. The prevalence rate of CI in females was over twice that in males (28% vs 12.9%), a significant difference. There were no significant differences in smoking, age, or education between CI and CN. Prevalence rates for symptoms and Relative Risk Ratios (RR) indicated that the CI were significantly more likely to report chronic cough, phlegm, wheeze, chest tightness, exertional dyspnea, acute respiratory illnesses, hay fever, child respiratory trouble, and physician confirmed asthma. Several of these respiratory symptoms were significantly, though differentially, related to ‘current’ asthma and hay fever reports. Results suggest a potential vulnerability to and greater interference from respiratory illness for the CI, which have implications for women's health and quality of life.
Similar content being viewed by others
References
Baldwin CM. Environmental health summit report: Research blueprint for the 21st century. Environ Health Perspec 1996; 104: 210–213.
Bascom R. Multiple chemical sensitivity: A respiratory disorder? Toxicol Indust Health 1992; 8: 221–228.
Bell IR, Hardin EE, Baldwin CM, Schwartz GE. Increased limbic system symptomatology and sensitizability of young adults with chemical and noise sensitivities. Environ Res 1995; 70: 84–97.
Bell IR, Martino GM, Meredith KE, Schwartz GE, Siani MM, Morrow FD. Vascular disease risk factors, urinary free cortisol and health histories in older adults: Shyness and gender interactions. Biol Psychology 1993; 35: 37–49.
Bell IR, Peterson JM, Schwartz GE. Medical histories and psychological profiles of middle-aged women with and without self-reported illness from environmental chemicals. J Clin Psychiatry 1995; 56: 151–160.
Bell IR, Schwartz GE, Peterson JM, Amend D. Self-reported illness from chemical odors in young adults without clinical syndromes or occupational exposures. Arch Environ Health 1993; 48: 6–13.
Bell IR, Schwartz GE, Peterson JM, Amend D. Symptom and personality profiles of young adults from a college student population with self-reported illness from foods and chemicals. J Am Coll Nutrition 1993; 12: 693–702.
Buchwald D, Garrity D. Comparison of patients with chronic fatigue syndrome, fibromyalgia, and multiple chemical sensitivities. Arch Intern Med 1994; 154: 2049–2053.
Burrows B, Knudson RJ, Lebowitz MD. The relationship of childhood respiratory illness to adult obstructive airway disease. Am Rev Respir Dis 1977; 115: 751–760.
Cone JE, Sult TA. Acquired intolerance to solvents following pesticide/solvent exposures in a building: A new group of workers at risk for multiple chemical sensitivity. Toxicol Indust Health 1992; 8: 29–39.
Doty RL. Olfaction and multiple chemical sensitivity. Toxicol Indust Health 1994; 10: 359–368.
Greenberg RS, Daniels SR, Flanders WD, Eley JW, Boring JR. Medical Epidemiology. Norwalk, CT: Appleton & Lange, 1993; 90–92.
Helsing KJ, Comstock GW, Speizer FE, Ferris BG, Lebowitz MD, Tockman MS, Burrows B. Comparison of three standardized questionnaires on respiratory symptoms. Am Rev Resp Dis 1979; 120: 1221–1231.
Kipen HM, Hallman W, Kelly-McNeil K, Fiedler N. Measuring chemical sensitivity prevalence: A questionnaire for population studies. Am J Public Health 1995; 85: 574–577.
Lebowitz MD, Burrows B. Comparison of questionnaires: The BMRC and NHLI respiratory questionnaires and a new self-completion questionnaire. Am Rev Respir Dis 1976; 113: 627–635.
Lebowitz MD, Burrows B, Traver GA, McDonagh DJ, Dodge RR, Barbee RA, Glover J, Kennedy T, Clark D, Resar R. Methodological considerations of epidemiological diagnoses in respiratory disease. Eur J Epidemiol 1985; 1: 188–192.
Meggs WJ. Multiple chemical sensitivities — chemical sensitivity as a symptom of airway inflammation (editorial). J Clin Toxicol 1995; 33: 107–110.
Meggs WJ, Cleveland CH. Rhinolaryngoscopic examination of patients with the multiple chemical sensitivity syndrome. Arch Environ Health 1993; 48: 14–18.
Morrow LA, Ryan CM, Hodgson MJ, Robin N. Alterations in cognitive and psychological functioning after organic solvent exposure. J Occupat Med 1990; 32: 444–450.
Neutra RR. Some preliminary thoughts on the potential contribution of epidemiology to the question of multiple chemical sensitivity. Public Health Rev 1994; 22: 271–278.
Quackenboss JJ, Lebowitz MD, Hayes C. Epidemiological study of respiratory responses to indoor/outdoor air quality. Environ Int 1989; 15: 493–502.
Quackenboss JJ, Lebowitz MD, Krzyzanowski M. The normal range of diurnal changes in peak expiratory flow rates. Am Rev Resp Dis 1991; 143: 323–329.
Rothman K. Modern epidemiology. New York: Brown, Little, Co., 1986, esp. 493–502.
Shim C, Williams MH. Effect of odors in asthma. Am J Med 1986; 80: 18–22.
Speizer F, Burrows B, Comstock G, Ferris B, Lebowitz MD, Samet J. Recommended respiratory disease questionnaires for use with adults and children in epidemiological research. Am Rev Resp Dis 1978; 118 (6, part 2): 7–53.
SPSS, Chicago, IL, 1993.
Szarek MJ, Bell IR, Schwartz, GE. Validation of a brief screening measure of environmental chemical sensitivity: The Chemical Odor Intolerance Index. J Environ Psychology (in press).
Wallace L, Nelson CJ, Kollander M, Leaderer B, Bascom R, Dunteman G. Indoor air quality and work environment study: Multivariate statistical analysis of health, comfort, and odor perceptions as related to personal and workplace characteristics. US Environmental Protection Agency 1991; 4: 32–33 (EPA Headquarters Buildings, Atmospheric Research and Exposure Assessment Laboratory, 21M-3004).
Walter SD. Methods of reporting statistical results from medical research studies. Am J Epidemiol 1995; 141: 896–906.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Baldwin, C., Bell, I., O'Rourke, M. et al. The association of respiratory problems in a community sample with self-reported chemical intolerance. Eur J Epidemiol 13, 547–552 (1997). https://doi.org/10.1023/A:1007341813396
Issue Date:
DOI: https://doi.org/10.1023/A:1007341813396