Abstract
The study investigated the influence of L-carnitine on the formation of malondialdehyde, an indicator of lipid peroxidation, in isolated Langendorff rat hearts. Earlier investigations of hemodynamic parameters and the recovery of ATP and creatine phosphate, carried out by means of 31P-NMR spectroscopy, had demonstrated that, depending on the composition of the perfusates (content of glucose, fatty acids, and carnitine), quite strong differences may occur in the reperfusion period after ischemia.
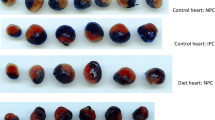
In order to determine a possible relationship between these differences and the addition of carnitine, the study investigated whether carnitine penetrated into the tissue during the experiments, and whether it was able to reduce the concentration of detrimental substances. The concentrations of free and total carnitine as well as the malondialdehyde content as an indicator of ischemia/reperfusion damage were determined in different parts of the cardiac tissue as follows: After the Langendorff-experiments the hearts were dissected, homogenized and reconditioned; then carnitine and malondialdehyde were determined. The study included 63 hearts, which were divided into 8 different perfusion groups.
Carnitine concentrations in heart tissue perfused with L-carnitine were much higher than those of the controls. Since exogenous L-carnitine and formed esters could be found in the tissue after the experiment, they must have permeated the cellular membrane rapidly. The concentrations of malondialdehyde behaved in an inverted way; as expected they were lower in carnitine-perfused hearts. The favourable effects of L-carnitine, expressed both by improved cardiac dynamics and ATP and CrP recovery in the reperfusion period, are obviously due to the fact that L-carnitine reduces ischemic damage.
Similar content being viewed by others
References
De Jong JW, Ferrari R (eds): The carnitine system - A new therapeutical approach to cardiovascular diseases. Kluwer Academic Publishers, Dordrecht/Boston/London, 1995
Arduini A: Carnitine and its acyl esters as secondary antioxidants? Am Heart J 123: 1726–1727, 1992
Löster H, Punzel M: Effects of L-carnitine on mechanical recovery of isolated rat hearts in relation to the perfusion with glucose and palmitate. Mol Cell Biochem 185: 65–75, 1998
Löster H, Keller T, Grommisch J, Gründer W: Effects of L-carnitine and its acetyl and propionyl esters on ATP and PCr levels of isolated rat hearts perfused without fatty acids and investigated by means of 31P-NMR spectroscopy. Mol Cell Biochem 200: 93–102, 1999
McGarry JD, Foster DW: An improved and simplified radioisotopic assay for the determination of free and esterified carnitine. J Lipid Res 17: 277–281, 1976
Uchiyama M, Mihara M: Determination of malondialdehyde precursors in tissues by thiobarbituric acid test. Anal Biochem 86: 271–278, 1978
Ohkawa H, Ohishi N, Yagi K: Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95: 351–358, 1979
Lilienthal JL, Zierler KL, Folk BP, Buka R, Riley M: A reference base and system for analysis of muscle constituents. J Biol Chem 182: 501–508, 1950
Lowry OH, Rosenbrough NI, Farr AL, Randell RI: Protein measurements with the folin reagent. J Biol Chem 193: 265–275, 1951
Arduini A, Fernandez E, Pallini R, Mancinelli G, Di Toppi GS, Belfiglio M, Scurti R, Federici G: Effect of propionyl-L-carnitine on rat spinal cord ischaemia and post-ischaemic reperfusion injury. Free Rad Res Commun 10: 325–332, 1990
Ferrari R, Ciampalini G, Agnoletti G, Cargnoni A, Ceconi C, Visioli O: Effect of L-carnitine derivatives on heart mitochondrial damage induced by lipid peroxidation. Pharmacol Res Commun 20: 125–132, 1988
Schinetti ML, Mazzini A: Effect of L-carnitine on human neutrophil activity. Int J Tissue React 8: 199–203, 1986
Schinetti ML, Rossini D, Greco R, Bertelli A: Protective action of acetylcarnitine on NADPH-induced lipid peroxidation of cardiac microsomes. Drugs Exp Clin Res 13: 509–515, 1987
Schinetti ML, Rossini D, Bertelli A: Prevention by propionylcarnitine of NADPH and tert-butyl hydroperoxide-dependent chemiluminescence in heart microsomes. Basic Life Sci 49: 243–247, 1988
Di Giacomo C, Latteri F, Fichera C, Sorrenti V, Campisi A, Castorina C, Russo A, Pinturo R, Vanella A: Effect of acetyl-L-carnitine on lipid peroxidation and xanthine oxidase activity in rat skeletal muscle. Neurochem Res 18: 1157–1162, 1993
Gürtler AK, Löster H: Carnitin und seine Bedeutung bei der Pathogenese und Therapie der Herz-und Kreislauferkrankungen. Ponte Press Verlag, Bochum, 1996
Rebouche CJ, Paulson DJ: Carnitine metabolism and functions in humans. Ann Rev Nutr 6: 41–66, 1986
Leipälä JA, Bhatnagar R, Pineda E, Najibi S, Massoumi K, Packer L: Protection of the reperfused heart by L-propionylcarnitine. J Appl Physiol 71: 1518–1522, 1991
Liedtke AJ, DeMaison L, Nellis SH: Effects of L-propionylcarnitine on mechanical recovery during reflow in intact hearts. Am J Physiol 255: H169–H176, 1988
Broderick TL, Quinney HA, Barker CC, Lopaschuk GD: Beneficial effect of carnitine on mechanical recovery of rat hearts reperfused after transient period of global ischemia is accompanied by a stimulation of glucose oxidation. Circulation 87: 972–981, 1993
Corr PB, Creer MH, Yamada KA, Saffitz JE, Sobel BE: Prophylaxis of early ventricular fibrillation by inhibition of acylcarnitine accumulation. J Clin Invest 83: 927–936, 1989
Martina B, Zuber M, Weiss P, Burkart F, Ritz R: Antiarrhythmische Behandlung mit L-Carnitin beim akuten Myokardinfarkt. Schweiz Med Wochenschr 122: 1352–1355, 1992
Sugiyama S, Myazaki Y, Kotaka K, Kato T, Suzuki S, Ozawa T: Mechanism of free fatty acid-induced arrhythmias. J Electrocardiol 15: 227–232, 1982
Canale C, Terrachini V, Biagini A, Vallebona A, Masperone MA, Valice S, Castellono A: Bicycle ergometer and echocardiographic study in healthy subjects and patients with angina pectoris after administration of L-carnitine: Semiautomatic computerized analysis of M-mode tracings. Int J Clin Pharmacol Ther Toxicol 26: 221–224, 1988
Ferrari R, Cucchini F, Visioli O: The metabolic effects of L-carnitine in angina pectoris. Int J Cardiol 5: 213–216, 1984
Kamikawa T, Suzuki Y, Kobayashi A, Hayashi H, Masumura Y, Nishihara K, Abe M, Yamazaki N: Effects of L-carnitine on exercise tolerance in patients with stable angina pectoris. Jpn Heart J 25: 587–597, 1984
Lagioia R, Scrutinio D, Mangini SG, Ricci A, Mastropasqua F, Valentini G, Ramunni G, Totaro-Filia G, Rizzon P: Propionyl-L-carnitine: A new compound in the metabolic approach to the treatment of effort angina. Int J Cardiol 34: 167–172, 1992
Chiariello O, Brevetti G, Policicchio A, Nevola E, Condorelli M: Lcarnitine in acute myocardial infarction; a multicenter randomized trial. In: P.R. Borum (ed). Clinical Aspects of Human Carnitine Deficiency. Pergamon Press, New York, 1986, pp 242–243
Rizzon R, Biasco G, Di Biase M, Boscia F, Rizzo U, Minafra F, Bortone A, Siliprandi N, Procopio A, Bagiella E: High doses of L-carnitine in acute myocardial infarction: Metabolic and antiarrhythmic effects. Eur Heart J 10: 502–508, 1989
Spagnoli LG, Corsi M, Villaschi S, Palmieri G, Maccari F: Myocardial carnitine deficiency in acute myocardial infarction. Lancet i: 1419–1420, 1982
Sushamakumari S, Jayadeep A, Kumar JS, Menon VP: Effect of carnitine on malondialdehyde, taurine and glutathion levels in heart of rats subjected to myocardial stress by isoproterenol. Indian J Exp Biol 27: 134–137, 1989
Subramanian R, Plehn S, Noonan J, Schmidt M, Shug AL: Free radical-mediated damage during myocardial ischemia and reperfusion and 90 protection by carnitine esters. Z Kardiol 76: 41–45, 1987
Shug AL, Paulson D, Subramanian R, Regitz V: Protective effects of propionyl-L-carnitine during ischemia and reperfusion. Cardiovasc Drugs Ther 5 (Suppl 1): 77–83, 1991
Tatlican O, Kalaycioglu S, Gokgoz L, Oktar L, Oz E, Soncul H, Sinci V, Turkozkan N, Yener A, Ersoz A: The dose-dependent effects of L-carnitine in myocardial protection in normothermic ischemia. Cardiovasc Surg 6: 145–148, 1998
Packer L, Valenza M, Serbinova E, Starke Reed P, Frost K, Kagan VE: Free radical scavenging in the protective effect of L-propionyl-carnitine against ischemia-reperfusion injury of the heart. Arch Biochem Biophys 288: 533–537, 1991
Reznick AZ, Kagan VE, Ramsey R, Tsuchiya M, Khwaja S, Serbinova EA, Packer L: Antiradical effects in L-propionyl carnitine protection of the heart against ischemia-reperfusion injury: The possible role of iron chelation. Arch Biochem Biophys 296: 394–401, 1992
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Löster, H., Böhm, U. L-Carnitine reduces malondialdehyde concentrations in isolated rat hearts in dependence on perfusion conditions. Mol Cell Biochem 217, 83–90 (2001). https://doi.org/10.1023/A:1007255021484
Issue Date:
DOI: https://doi.org/10.1023/A:1007255021484