Abstract
Introduction: Schistosomiasis is a parasitosis affecting 200 to 250 million people around the world, mainly in tropical and subtropical regions of Africa, Asia, Central and South America. Most clinical manifestations are related to egg deposition and the formation of granulomas and fibrous tissues around the eggs produced by the worms. Fibrosis of the ureter and the bladder are well-known occurrences. Obstruction of the bladder neck is also a known but rarely diagnosed manifestation. Our experience from the endemic area (Yemen) is presented.
Patients: In two years bladder outlet obstruction was observed in 8 young (mean age: 33 years) Yemeni male patients. The symptoms were frequency, dysuria and - in 4 cases - suprapubic pain. For the diagnosis we obtained detailed history, performed proper ultrasound examination, plain X-ray, intravenous pyelography and urethro-cystoscopy.
Results: One patient suffered from active bilharzial infection (the eggs were visible in the urine), all others developed the disease years (on average 10 years) later. Seven males have been previously treated for chronic prostatitis for months. Obstruction has been confirmed with postvoid residual urine measurement and cystoscopic evaluation. All patients showed hyperechoic wall at the base of the bladder. Four patients were treated. Treatment for these young patients should be chosen prudently in order to preserve normal ejaculation. In the active infection medical treatment (praziquantel 40 mg/kg), in late forms transurethral prostate incision were performed. All treated patients became symptom-free.
Conclusion: Bladder neck obstruction is a known - nevertheless rarely diagnosed - manifestation of urinary schistosomiasis. On the endemic territory it is useful to keep in mind this disease in case of obstructive symptoms in young males. In the acute phase medical treatment and in late forms transurethral incision can be successful.
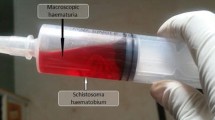
Schistosomiasis or bilharziasis is a parasitosis affecting 200 to 250 million people around the world. Three main species of schistosomes are commonly affecting man: S. mansoni (endemic in much of Africa, parts of Southwest Asia, the Caribbean and South America); S. Japonicum (endemic in Japan, China, the Philippines and parts of Southeast Asia); S. haematobium endemic in much of Africa and parts of Southwest Asia). Around the world about 80 million people are infected with S. haematobium. This number is on the increase in endemic areas because of the construction of modern irrigation systems that provide favourable conditions for the intermediate host (Bulinus Truncatus). The life-cycle is similar in the three groups. The adult worm of S. haematobium lives in the perivesical plexus and lies the eggs into the lumen of the submucosal veins. The eggs penetrate the urothelium and pass into the lumen of the bladder and pass out with the urine. In active infection end-spined eggs are visible during urine analysis. Most clinical manifestations are related to egg deposition and the formation of granulomas and fibrous tissue around the eggs produced by the worms. Fibrosis of the ureter and the bladder are well-known events. Obstruction of the bladder neck is a known, but rarely diagnosed manifestation. In Yemen out of 17 million inhabitants 2–3 million suffer from the disease [1]. The accurate incidence is not known but there are areas where 60–70% of males are infected [2].
Similar content being viewed by others
References
Arafa, F.: Schistosomiasis Republic of Yemen. WHO Assignment report 1990; YES/PDP/001.
Hazza, Y. A., Arrfa, F., Haggar, M.: Studies on schistosomiasis in Taiz Province, Yemen Arab Republic. Am. J. Trop. Med. Hyg., 32, 1023 (1983).
Trockman, B. A., Gerspach, J., Dmochowski, R., Haab, F., Zimmern, P. E., Leach, G. E.: Primary bladder neck obstruction: urodynamic findings and treatment results in 36 men. J. Urol., 156, 1418 (1996).
Bruskewitz, R. C., Christensen, M. M.: Critical evaluation of transurethral resection and incision of the prostate. Prostate (Suppl.), 3, 27 (1990).
Norlen, L. J., Blaivas, J. G.: Unsuspected proximal urethral obstruction in young and middle-aged men. J. Urol., 135, 972 (1986).
Atalah, A., Zaher, M. F., Ragy, I.: Bilharzial bladder outlet obstruction. J. Urol., 10, 183 (1969).
Badr, M. M., Torky, H.: Bilharzial bladder neck obstruction. Med. J. Cairo University, 34, 141 (1966).
Zaher, M. F., El-Deeb, A.: Bilharziasis of the prostate: Its relationship to bladder neck obstruction and its management. J. Urol., 106, 257 (1971).
Zaher, M. F., Safwat, M. M., Fawzy, R. M., Badr, M. M.: Bilharzial bladder neck obstruction, a neglected syndrome. J. Egyptian Med. Ass., 39, 481 (1956).
Koraitim, M., Al-Ghorab, M.: Normal ejaculation after Y-V urethrocystoplasty. Br. J. Urol., 42, 465 (1970).
Radi, I.: A new look on bladder neck obstruction syndrome with evaluation of different surgical corrections. Experience with 92 cases. Egyptian Journal of Urology, 4, 67 (1978).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Salah, M.A., Böszörményi-Nagy, G., Alsaaidi, A.A. et al. Bladder Neck Obstruction in Young Males with History of Bilharzial Infection. Int Urol Nephrol 31, 781–786 (1999). https://doi.org/10.1023/A:1007149714281
Issue Date:
DOI: https://doi.org/10.1023/A:1007149714281