Abstract
Study Design
Retrospective comparative study.
Objectives
We aimed to characterize the frequency of perioperative laboratory tests for posterior spinal fusion (PSF) for adolescent idiopathic scoliosis (AIS) and to assess whether test results affected clinical management.
Summary of Background Data
Perioperative laboratory tests for PSF including complete blood count, coagulation laboratory tests, basic metabolic panels (BMPs), and type and screen, are commonly ordered based on providers’ discretion or existing order sets. Studies have shown unnecessary laboratory tests as financially and physically costly in adults; however, no studies have examined the necessity of common perioperative laboratory tests in pediatric spinal deformity surgery.
Methods
Retrospective review of patients aged 10–18 years who underwent PSF for AIS at our center in the past three years. The clinical utility of perioperative laboratory tests was assessed based on detected incidence of anemia, blood transfusions, hematology/endocrinology/nephrology consultations, insulin administration, and postponed/canceled surgeries.
Results
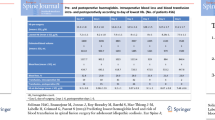
A total of 234 patients were included (mean age 14.4 ± 1.8 years, 75% female). Of 105 (44.9%) patients with preoperative coagulation laboratory tests, 21 (20%) had abnormal results; however, none had subsequent hematology consultations or canceled/postponed surgeries. Postoperatively, only 5 (2.1%) patients and 30 (12.8%) patients had hemoglobin values less than 8 g/dL on postoperative day (POD) 1 and 2, respectively. Multivariate analysis identified POD1 hemoglobin ≤9.35 g/dL as the only predictor of hemoglobin <8 g/dL on POD2. Overall, there were 8 (3.4%) indicated blood transfusions postoperatively. Costs of unnecessary laboratory tests averaged $95.27 (range $49.72 to $240.27) per patient.
Conclusions
Many perioperative laboratory orders may be unnecessary in pediatric spinal deformity surgery, subjecting patients to extraneous costs and needlesticks. In particular, preoperative coagulation laboratory tests, perioperative BMPs, and additional postoperative CBCs for those with hemoglobin >9.35 on POD1 may not be warranted.
Level of Evidence
Level III, retrospective cohort study.
Similar content being viewed by others
References
Iams W, Heck J, Kapp M, et al. A multidisciplinary housestaff-led initiative to safely reduce daily laboratory testing. Acad Med 2016;91:813–20.
Stuebing EA, Miner TJ. Surgical vampires and rising health care expenditure: reducing the cost of daily phlebotomy. Arch Surg 2011;146:524–7.
Thavendiranathan P, Bagai A, Ebidia A, et al. Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. J Gen Intern Med 2005;20:520–4.
Howanitz PJ, Cembrowski GS, Bachner P; Laboratory phlebotomy. College of American Pathologists Q-Probe study of patient satisfaction and complications in 23,783 patients. Arch Pathol Lab Med 1991;115:867–72.
Howanitz PJ, Schifman RB. Phlebotomists’ safety practices. A College of American Pathologists Q-Probes study of 683 institutions. Arch Pathol Lab Med 1994;118:957–62.
Shaner JL, Karim AR, Casper DS, et al. Routine postoperative laboratory tests are unnecessary after partial knee arthroplasty. J Arthroplasty 2016;31:2764–7.
Aydin D, Sahiner NC, Ciftci EK. Comparison of the effectiveness of three different methods in decreasing pain during venipuncture in children: ball squeezing, balloon inflating and distraction cards. J Clin Nurs 2016;25:2328–35.
Cohen LL, Lemanek K, Blount RL, et al. Evidence-based assessment of pediatric pain. J Pediatr Psychol 2008;33:939–55; discussion 956–7.
Pillai Riddell RR, Racine NM, Turcotte K, et al. Non-pharmacological management of infant and young child procedural pain. Cochrane Database Syst Rev 2011;10:CD006275.
Canbulat N, Inal S, Sonmezer H. Efficacy of distraction methods on procedural pain and anxiety by applying distraction cards and kaleidoscope in children. Asian Nurs Res (Korean Soc Nurs Sci) 2014;8:23–8.
American Academy of Pediatrics, Committee on Psychosocial Aspects of Child and Family Health. Task Force on Pain in Infants, Children, and Adolescents. The assessment and management of acute pain in infants, children, and adolescents. Pediatrics 2001;108:793–7.
Fletcher ND, Glotzbecker MP, Marks M, et al. Development of consensus-based best practice guidelines for postoperative care following posterior spinal fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2017;42:E547–54.
Gornitzky AL, Flynn JM, Muhly WT, Sankar WN. A rapid recovery pathway for adolescent idiopathic scoliosis that improves pain control and reduces time to inpatient recovery after posterior spinal fusion. Spine Deform 2016;4:288–95.
Muhly WT, Sankar WN, Ryan K, et al. Rapid recovery pathway after spinal fusion for idiopathic scoliosis. Pediatrics 2016;137.
Dewan M, Galvez J, Polsky T, et al. Reducing unnecessary postoperative complete blood count testing in the pediatric intensive care unit. Perm J 2017;21:16–051.
Parker RI. Transfusion in critically ill children: indications, risks, and challenges. Crit Care Med 2014;42:675–90.
Jones T, DeMore M, Cohen LL, et al. Childhood healthcare experience, healthcare attitudes, and optimism as predictors of adolescents’ healthcare behavior. J Clin Psychol Med Settings 2008;15:234–40.
Kennedy RM, Luhmann J, Zempsky WT. Clinical implications of unmanaged needle-insertion pain and distress in children. Pediatrics 2008;122(suppl 3):S130–3.
Leahy S, Kennedy RM, Hesselgrave J, et al. On the front lines: lessons learned in implementing multidisciplinary peripheral venous access pain-management programs in pediatric hospitals. Pediatrics 2008;122(suppl 3):S161–70.
Mahoney L, Ayers S, Seddon P. The association between parent’s and healthcare professional’s behavior and children’s coping and distress during venepuncture. J Pediatr Psychol 2010;35:985–95.
Mutlu B, Balci S. Effects of balloon inflation and cough trick methods on easing pain in children during the drawing of venous blood samples: a randomized controlled trial. J Spec Pediatr Nurs 2015;20:178–86.
ABIM Foundation. Things providers and patients should question. Choosing Wisely. Available at: http://www.choosingwisely.org. Accessed April 26, 2018.
Samkova A, Blatný J, Fiamoli V, et al. Significance and causes of abnormal preoperative coagulation test results in children. Haemophilia 2012;18:e297–301.
Shaw PH, Reynolds S, Gunawardena S, et al. The prevalence of bleeding disorders among healthy pediatric patients with abnormal preprocedural coagulation studies. J Pediatr Hematol Oncol 2008;30:135–41.
Levy JH, Szlam F, Wolberg AS, Winkler A. Clinical use of the activated partial thromboplastin time and prothrombin time for screening: a review of the literature and current guidelines for testing. Clin Lab Med 2014;34:453–77.
Tobias JD. Strategies for minimizing blood loss in orthopedic surgery. Semin Hematol 2004;41(1 suppl 1):145–56.
McLeod LM, French B, Flynn JM, et al. Antifibrinolytic use and blood transfusions in pediatric scoliosis surgeries performed at US children’s hospitals. J Spinal Disord Tech 2015;28:E460–6.
Lakomkin N, Sathiyakumar V, Dodd AC, et al. Pre-operative labs: wasted dollars or predictors of post-operative cardiac and septic events in orthopaedic trauma patients? Injury 2016;47:1217–21.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: AJA (none), PJC (personal fees from Biogen, Inc., and NuVasive, Inc., outside the submitted work; other from AAOS [board or committee member], Journal of Bone and Joint Surgery–American [editorial or governing board], Pediatric Orthopaedic Society of North America [board or committee member], Scoliosis Research Society [board or committee member], Spine Deformity [editorial or governing board]), JMF (personal fees from Biomet, other from Wolters Kluwer Health–Lippincott Williams & Wilkins, outside the submitted work; and AAOS [board or committee member], American Board of Orthopaedic Surgery, Inc. [board or committee member], Orthopedics Today [editorial or governing board], Pediatric Orthopaedic Society of North America [board or committee member], Scoliosis Research Society [board or committee member]), and WNS ( receive royalties from Wolter Kluwer Health for edited textbooks, committees for the Pediatric Orthopaedic Society of North America).
IRB approval: This was an IRB approved study performed at The Children’s Hospital of Philadelphia (17-014629).
Sources of funding: None.
Rights and permissions
About this article
Cite this article
Adams, A.J., Cahill, P.J., Flynn, J.M. et al. Utility of Perioperative Laboratory Tests in Pediatric Patients Undergoing Spinal Fusion for Scoliosis. Spine Deform 7, 875–882 (2019). https://doi.org/10.1016/j.jspd.2019.02.009
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2019.02.009