Abstract
Study Design
Prognostic study and validation using prospective clinical trial data.
Objective
To derive and validate a model predicting curve progression to ≥45° before skeletal maturity in untreated patients with adolescent idiopathic scoliosis (AIS).
Summary of Background Data
Studies have linked the natural history of AIS with characteristics such as sex, skeletal maturity, curve magnitude, and pattern. The Simplified Skeletal Maturity Scoring System may be of particular prognostic utility for the study of curve progression. The reliability of the system has been addressed; however, its value as a prognostic marker for the outcomes of AIS has not. The BrAIST trial followed a sample of untreated AIS patients from enrollment to skeletal maturity, providing a rare source of prospective data for prognostic modeling.
Methods
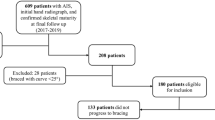
The development sample included 115 untreated BrAIST participants. Logistic regression was used to predict curve progression to ≥45° (or surgery) before skeletal maturity. Predictors included the Cobb angle, age, sex, curve type, triradiate cartilage, and skeletal maturity stage (SMS). Internal and external validity was evaluated using jackknifed samples of the BrAIST data set and an independent cohort (n = 152). Indices of discrimination and calibration were estimated. A risk classification was created and the accuracy evaluated via the positive (PPV) and negative predictive values (NPV).
Results
The final model included the SMS, Cobb angle, and curve type. The model demonstrated strong discrimination (c-statistics 0.89–0.91) and calibration in all data sets. The classification system resulted in PPVs of 0.71–0.72 and NPVs of 0.85–0.93.
Conclusions
This study provides the first rigorously validated model predicting a short-term outcome of untreated AIS. The resultant estimates can serve two important functions: 1) setting benchmarks for comparative effectiveness studies and 2) most importantly, providing clinicians and families with individual risk estimates to guide treatment decisions.
Level of Evidence
Level 1, prognostic.
Similar content being viewed by others
References
Noshchenko A, Hoffecker L, Lindley EM, et al. Predictors of spine deformity progression in adolescent idiopathic scoliosis: a systematic review with meta-analysis. World J Orthop 2015;6:537–58.
Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 1983;65:447–55.
Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am 1984;66:1061–71.
Bunnell WP The natural history of idiopathic scoliosis before skeletal maturity. Spine (Phila Pa 1976) 1986;11:773–6.
Peterson LE, Nachemson AL. Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity. Logistic regression analysis based on data from the brace study of the Scoliosis Research Society. J Bone Joint Surg Am 1995;77:823–7.
Ward K, Ogilvie JW, Singleton MV, et al. Validation of DNA-based prognostic testing to predict spinal curve progression in adolescent idiopathic scoliosis. Spine 2010;35:E1455–64.
Yeung HY, Tang NL, Lee KM, et al. Genetic association study of insulin-like growth factor-i (IGF-I) gene with curve severity and osteopenia in adolescent idiopathic scoliosis. Stud Health Technol Inform 2006;123:18–24.
Lam TP, Hung VW, Yeung HY, et al. Quantitative ultrasound for predicting curve progression in adolescent idiopathic scoliosis: a prospective cohort study of 294 cases followed-up beyond skeletal maturity. Ultrasound Med Biol 2013;39:381–7.
Yip BH, Yu FW, Wang Z, et al. Prognostic value of bone mineral density on curve progression: a longitudinal cohort study of 513 girls with adolescent idiopathic scoliosis. Sci Rep 2016;6:39220.
Cheung J, Veldhuizen AG, Halbertsma JP, et al. The relation between electromyography and growth velocity of the spine in the evaluation of curve progression in idiopathic scoliosis. Spine (Phila Pa 1976) 2004;29:1011–6.
LeBlanc R, Labelle H, Forest F, et al. Morphologic discrimination among healthy subjects and patients with progressive and nonprogressive adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 1998;23:1109–15; discussion 15–6.
Kindsfater K, Lowe T, Lawellin D, et al. Levels of platelet calmodulin for the prediction of progression and severity of adolescent idiopathic scoliosis. J Bone Joint Surg Am 1994;76:1186–92.
Lowe TG, Burwell RG, Dangerfield PH. Platelet calmodulin levels in adolescent idiopathic scoliosis (AIS): can they predict curve progression and severity? Summary of an electronic focus group debate of the IBSE. Eur Spine J 2004;13:257–65.
Ajemba PO, Ramirez L, Durdle NG, et al. A support vectors classifier approach to predicting the risk of progression of adolescent idiopathic scoliosis. IEEE Trans Inf Technol Biomed 2005;9:276–82.
Yamauchi Y, Yamaguchi T, Asaka Y. Prediction of curve progression in idiopathic scoliosis based on initial roentgenograms. A proposal of an equation. Spine (Phila Pa 1976) 1988;13:1258–61.
Skalli W, Vergari C, Ebermeyer E, et al. Early detection of progressive adolescent idiopathic scoliosis: a severity index. Spine (Phila Pa 1976) 2017;42:823–30.
Nault ML, Mac-Thiong JM, Roy-Beaudry M, et al. Three-dimensional spinal morphology can differentiate between progressive and nonprogressive patients with adolescent idiopathic scoliosis at the initial presentation: a prospective study. Spine (Phila Pa 1976) 2014;39:E601–6.
Kadoury S, Mandel W, Roy-Beaudry M, et al. 3-D morphology prediction of progressive spinal deformities from probabilistic modeling of discriminant manifolds. IEEE Trans Med Imaging 2017;36:1194–204.
Hung VW, Qin L, Cheung CS, et al. Osteopenia: a new prognostic factor of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am 2005;87:2709–16.
Sanders JO, Khoury JG, Kishan S, et al. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am 2008;90:540–53.
Sanders JO, Browne RH, McConnell SJ, et al. Maturity assessment and curve progression in girls with idiopathic scoliosis. J Bone Joint Surg Am 2007;89:64–73.
Verma K, Sitoula P, Gabos P, et al. Simplified skeletal maturity scoring system: learning curve and methods to improve reliability. Spine 2014;39:E1592–8.
Sitoula P, Verma K, Holmes Jr L, et al. Prediction of curve progression in idiopathic scoliosis: validation of the Sanders Skeletal Maturity Staging System. Spine 2015;40:1006–13.
Nicholson AD, Sanders JO, Liu RW, et al. The relationship of calcaneal apophyseal ossification and Sanders hand scores to the timing of peak height velocity in adolescents. Bone Joint J 2015;97:1710–7.
Vira S, Husain Q, Jalai C, et al. The interobserver and intraobserver reliability of the Sanders classification versus the Risser stage. J Pediatr Orthop 2017;37:e246–9.
Minkara A, Bainton N, Tanaka M, et al. High risk of mismatch between Sanders and Risser staging in adolescent idiopathic scoliosis: are we guiding treatment using the wrong classification. J Pediatr Orthop 2018 [Epub ahead of print].
Collins G, Reitsma J, Altman D, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Br J Surg 2015;102:148–58.
Weinstein SL, Dolan LA, Wright JG, et al. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013;369:1512–21.
Katz DE, Herring JA, Browne RH, et al. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am 2010;92:1343–52.
Karol LA, Virostek D, Felton K, et al. The effect of the Risser stage on bracing outcome in adolescent idiopathic scoliosis. J Bone Joint Surg Am 2016;98:1253–9.
Akaike H. A new look at the statistical model identification. IEEE Trans Automatic Control 1974;19:716–23.
Moons KG, Donders AR, Steyerberg EW, et al. Penalized maximum likelihood estimation to directly adjust diagnostic and prognostic prediction models for overoptimism: a clinical example. J Clin Epidemiol 2004;57:1262–70.
Hosmer D, Lemeshow S. Applied logistic regression. 2nd ed. New York, NY: John Wiley & Sons; 2000.
Vergouwe Y, Steyerberg EW, Eijkemans MJ, et al. Substantial effective sample sizes were required for external validation studies of predictive logistic regression models. J Clin Epidemiol 2005;58:475–83.
Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the brace study of the Scoliosis Research Society. J Bone Joint Surg Am 1995;77:815–22.
Danielsson AJ, Hasserius R, Ohlin A, et al. A prospective study of brace treatment versus observation alone in adolescent idiopathic scoliosis: a follow-up mean of 16 years after maturity. Spine (Phila Pa 1976) 2007;32:2198–207.
Vickers AJ, Elkin EB. Decision curve analysis: A novel method for evaluating prediction models. Med Decis Making 2006;26:565–74.
Dolan LA, Sabesan V, Weinstein SL, et al. Preference assessment of recruitment into a randomized trial for adolescent idiopathic scoliosis. J Bone Joint Surg Am 2008;90:2594–605.
Appendix References
Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013;369:1512–21.
Sitoula P, Verma K, Holmes Jr L, et al. Prediction of curve progression in idiopathic scoliosis: validation of the Sanders Skeletal Maturity Staging System. Spine 2015;40:1006–13.
Katz DE, Herring JA, Browne RH, et al. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am 2010;92:1343–52.
Karol LA, Virostek D, Felton K, et al. The effect of the Risser stage on bracing outcome in adolescent idiopathic scoliosis. J Bone Joint Surg Am 2016;98:1253–9.
Akaike H. A new look at the statistical model identification. IEEE Trans Automat Contr 1974;AC-19:716–23.
Moons KG, Donders AR, Steyerberg EW, Harrell FE. Penalized maximum likelihood estimation to directly adjust diagnostic and prognostic prediction models for overoptimism: a clinical example. J Clin Epidemiol 2004;57:1262–70.
SAS/STAT(R) 9.2 User’s Guide, 2nd ed. The LOGISTIC procedure. Predicted probability of an event for classification. Available at, https://support.sas.com/documentation/cdl/en/statug/63033/HTML/default/viewer.htm#statug_logistic_sect037.htm#statug.logistic.logisticppec. Accessed July 30, 2018.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: LAD (grants from NIH/NIAMS, Canadian Institutes of Health Research, Shriner’s Hospitals for Children, Children’s Miracle Network, and Joan and Phill Berger Charitable Fund; other from Estate of Herb and Nancy Townsend, during the conduct of the study; grants from Pediatric Orthopedic Society of North America [POSNA], consulting agreement with Green Sun Medical via the University of Iowa, outside the submitted work), SLW (grants from NIH/NIAMS, Canadian Institutes of Health Research, Shriner’s Hospitals for Children, Children’s Miracle Network, and Joan and Phill Berger Charitable Fund; other from Estate of Herb and Nancy Townsend, during the conduct of the study), MFA (grants from NIH/NIAMS, during the conduct of the study), PPB (none), MBD (none), TOF (none), MFH (none), MTH (other from Boston Orthotics and Prosthetic, other from NuVasive, outside the submitted work; and member, board of directors, POSNA, committee chair, Scoliosis Research Society), WFK (none), CTM (grants from NIH/NIAMS, University of Iowa, during the conduct of the study; personal fees from Hawaii Orthopaedic Association, Albert Einstein Hospital Sao Paulo, Brazil, Denver Children’s Hospital, University of Colorado, Michigan State University, and Vanderbilt University; and other from US News & World Report, Best Children’s Hospital; nonfinancial support from Journal of Pediatric Orthopaedics, Journal of Orthopaedic Trauma, Journal of Children’s Orthopaedics, and the Spine Journal; personal fees from Oakstone Medial Publishing, outside the submitted work), JOS (grants from University of Iowa, SRS and POSNA, outside the submitted work), JOS (grants from Joan and Phill Berger Charitable Fund, during the conduct of the study; grants from SRS and POSNA, outside the submitted work; and committee chair, POSNA, SRS Stock ownership, Abbot Labs, Abbvie, GE, Green Sun Medical), RMS (other from POSNA and American Academy of Pediatrics; personal fees, nonfinancial support, and other from Medtronic; other from Project Perfect World, outside the submitted work), SAS (personal fees from DePuy Synthes Spine, grants from Setting Scoliosis Straight Foundation, outside the submitted work), KV (personal fees from Spine Mark, outside the submitted work).
Human subjects’ research approval for BrAIST was obtained from the local boards of all participating centers; approval for collection and use of additional data was obtained from the University of Iowa and Nemours/Alfred I. duPont Hospital for Children.
Financially supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (R21AR049587 and R01AR052113); the Children’s Miracle Network, the Canadian Institutes of Health Research (FRN-81050), the Shriners Hospitals for Children, the University of Rochester, Children’s Mercy Kansas City, the Joan and Phill Berger Charitable Fund, and the Estate of Herb and Nancy Townsend.
Rights and permissions
About this article
Cite this article
Dolan, L.A., Weinstein, S.L., Abel, M.F. et al. Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST): Development and Validation of a Prognostic Model in Untreated Adolescent Idiopathic Scoliosis Using the Simplified Skeletal Maturity System. Spine Deform 7, 890–898 (2019). https://doi.org/10.1016/j.jspd.2019.01.011
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2019.01.011