Abstract
Study Design
Cohort study.
Objectives
To report the two-year revision risk following primary adult spinal deformity (ASD) surgery, describe reasons for revisions, and assess risk factors for revision surgery.
Summary of Background Data
Revision risk following primary ASD surgery has been reported to vary between 7% and 26%, but with loss to follow-up as a considerable challenge.
Methods
Patients ≥18 years of age undergoing primary instrumented surgery for ASD in Denmark during 2006–2014 were identified by procedure and diagnosis codes in the Danish National Patient Registry (DNPR). Complete two-year follow-up on revision surgery for each patient was achieved. Medical records were reviewed to determine reasons for revisions. Overall comorbidity was summarized using the Charlson Comorbidity Index (CCI) based on DNPR data; low comorbidity (CCI 0); medium comorbidity (CCI 1–2); and high comorbidity (CCI ≥3). Risk factors for revision were assessed in a Cox regression model.
Results
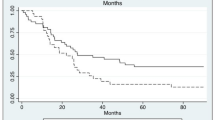
A total of 553 patients were identified. Of these, 19.9% were revised within the two-year follow-up and 7.2% of patients were revised more than once. Median time to revision was 308 days (interquartile range 105–508). The most common reason for revision was implant failure (38.2%) followed by infection (11.8%). Increased age (hazard ratio [HR] = 1.13, 95% confidence interval [CI] 1.01–1.26, per 10 years increment) and high comorbidity burden (HR = 2.10, 95% CI 1.16–3.79) were associated with increased revision risk. Risk of revision increased from 2006 to 2014; hence, year of primary surgery (with 2006 as reference) was associated with increased revision risk (HR = 1.09, 95% CI 1.01–1.18).
Conclusions
The revision risk within 2 years after primary ASD surgery was 19.9% nationwide in Denmark, and implant failure was the most common reason for revision. Increased comorbidity and age were separately associated with increased risk of revision.
Level of Evidence
Level II.
Similar content being viewed by others
References
Pellisé F, Vila-Casademunt A, Ferrer M, et al. Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J 2014;24:3–11.
Schwab F, Dubey A, Pagala M, et al. Adult scoliosis: a health assessment analysis by SF-36. Spine (Phila Pa 1976) 2003;28:602–6.
Sing DC, Berven SH, Burch S, Metz LN. Increase in spinal deformity surgery in patients age 60 and older is not associated with increased complications. Spine J 2017;17:627–35.
Cowan JA, Dimick JB, Wainess R, et al. Changes in the utilization of spinal fusion in the United States. Neurosurgery 2006;59:15–8.
Auerbach JD, Lenke LG, Bridwell KH, et al. Major complications and comparison between 3–column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976) 2012;37:1198–210.
Cho SK, Bridwell KH, Lenke LG, et al. Maj or complications in revision adult deformity surgery. Spine (Phila Pa 1976) 2012;37:489–500.
Soroceanu A, Burton DC, Oren JH, et al. Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine (Phila Pa 1976) 2016;18:345–52.
Schwab FJ, Hawkinson N, Lafage V, et al. Risk factors for major perioperative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. Eur Spine J 2012;21:2603–10.
Pichelmann MA, Lenke LG, Bridwell KH, et al. Revision rates following primary adult spinal deformity surgery. Spine (Phila Pa 1976) 2010;35:219–26.
Mok JM, Cloyd JM, Bradford DS, et al. Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. Spine (Phila Pa 1976) 2009;34:832–9.
Zhu F, Bao H, Liu Z, et al. Unanticipated revision surgery in adult spinal deformity. Spine (Phila Pa 1976) 2014;39:B36–44.
Glassman SD, Dimar JR, Carreon LY. Revision rate after adult deformity surgery. Spine Deform 2015;3:199–203.
Passias PG, Soroceanu A, Yang S, et al. Predictors of revision surgical procedure excluding wound complications in adult spinal deformity and impact on patient-reported outcomes and satisfaction. J Bone Joint Surg Am 2016;98:536–43.
Hallager DW, Karstensen S, Bukhari N, et al. Radiographic predictors for mechanical failure after adult spinal deformity surgery. Spine (Phila Pa 1976) 2017;42:E855–63.
Puvanesarajah V, Shen FH, Cancienne JM, et al. Risk factors for revision surgery following primary adult spinal deformity surgery in patients 65 years and older. J Neurosurg Spine 2016;25(4):486–93.
Faloon MJ, Essig D, Cho W, et al. Unplanned reoperations affect long-term outcomes in adult spinal deformity patients undergoing long fusions to the sacrum. Spine Deform 2015;3:367–71.
Emami A, Deviren V, Berven S, et al. Outcome and complications of long fusions to the sacrum in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976) 2002;27:776–86.
Lapp MA, Bridwell KH, Lenke LG, et al. Long-term complications in adult spinal deformity patients having combined surgery: a comparison of primary to revision patients. Spine (Phila Pa 1976) 2001;26:973–83.
Kim YJ, Bridwell KH, Lenke LG, et al. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976) 2006;31:2329–36.
Kim YJ, Bridwell KH, Lenke LG, et al. Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Joint Surg Am 2006;88:721–8.
Rinella A, Bridwell K, Kim Y, et al. Late complications of adult idiopathic scoliosis primary fusions to L4 and above: the effect of age and distal fusion level. Spine (Phila Pa 1976) 2004;29:318–25.
Cho SK, Bridwell KH, Lenke LG, et al. Comparative analysis of clinical outcome and complications in primary versus revision adult scoliosis surgery. Spine (Phila Pa 1976) 2012;37:393–401.
Diebo BG, Passias PG, Marascalchi BJ, et al. Primary versus revision surgery in the setting of adult spinal deformity. Spine (Phila Pa 1976) 2015;40:1674–80.
Hassanzadeh H, Jain A, El Dafrawy MH, et al. Clinical results and functional outcomes of primary and revision spinal deformity surgery in adults. J Bone Joint Surg Am 2013;95:1413–9.
Linville DA, Bridwell KH, Lenke LG, et al. Complications in the adult spinal deformity patient having combined surgery. Does revision increase the risk? Spine (Phila Pa 1976) 1999;24: 355–63.
Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health 2011;39:30–3.
Schmidt M, Schmidt SAJ, Sandegaard JL, et al. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015;7:449–90.
Andersen TF, Madsen M, Jorgensen J, et al. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 1999;46:263–8.
Schmidt M, Pedersen L, S0rensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 2014;29: 541–9.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83.
Thygesen SK, Christiansen CF, Christensen S, et al. The predictive value of ICD-10 diagnostic coding used to assess Charlson Comorbidity Index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol 2011;11:83.
Varadhan R, Weiss CO, Segal JB, et al. Evaluating health outcomes in the presence of competing risks. Med Care 2010;48: S96–105.
Maier SP, Smith JS, Schwab FJ, et al. Revision surgery after 3-column osteotomy in 335 patients with adult spinal deformity. Spine (Phila Pa 1976) 2014;39:881–5.
Nandyala SV, Marquez-Lara A, Fineberg SJ, et al. Complications after lumbar spine surgery between teaching and nonteaching hospitals. Spine (Phila Pa 1976) 2014;39:417–23.
Fineberg SJ, Oglesby M, Patel AA, et al. Outcomes of cervical spine surgery in teaching and non-teaching hospitals. Spine (Phila Pa 1976) 2013;38:1089–96.
Sanchez-Mariscal F, Gomez-Rice A, Izquierdo E, et al. Survivorship analysis after primary fusion for adult scoliosis. Prognostic factors for reoperation. Spine J 2014;14:1629–34.
Danish Health Authority. Specialeplanen 2010. Available at: https://www.sst.dk/da/planlaegning/specialeplanlaegning/gaeldende-specialeplan/~/media/DF5C1EF862324853B81BEA9D13366BAA.ashx.
McCarthy IM, Hostin RA, O’Brien MF, et al. Analysis of the direct cost of surgery for four diagnostic categories of adult spinal deformity. Spine J 2013;13:1843–8.
Yeramaneni S, Robinson C, Hostin R. Impact of spine surgery complications on costs associated with management of adult spinal deformity. Curr Rev Musculoskelet Med 2016;9:327–32.
Fischer CR, Terran J, Lonner B, et al. Factors predicting cost-effectiveness of adult spinal deformity surgery at 2 years. Spine Deform 2014;2:415–22.
Terran J, McHugh BJ, Fischer CR, et al. Surgical treatment for adult spinal deformity: projected cost effectiveness at 5–year follow-up. Ochsner J 2014;14:14–22.
McCarthy I, O’Brien M, Ames C, et al. Incremental cost-effectiveness of adult spinal deformity surgery: observed quality-adjusted life years with surgery compared with predicted quality-adjusted life years without surgery. Neurosurg Focus 2014;36:E3.
Uribe JS, Deukmedjian AR, Mummaneni PV, et al. Complications in adult spinal deformity surgery: an analysis of minimally invasive, hybrid, and open surgical techniques. Neurosurg Focus 2014;36: E15.
Sethi RK, Pong RP, Leveque J-C, et al. The Seattle Spine Team approach to adult deformity surgery: a systems-based approach to perioperative care and subsequent reduction in perioperative complication rates. Spine Deform 2014;2:95–103.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: FTP (none), MLL (none), ABP (none), BD (grants from K2M, grants from Globus Medical, outside the submitted work), MG (grants from K2M, grants from Medtronic, outside the submitted work).
IRB approval: The Danish National Ethics Committee waived the need for approval.
This work was supported by an institutional research grant from Medtronic.
Rights and permissions
About this article
Cite this article
Pitter, F.T., Lindberg-Larsen, M., Pedersen, A.B. et al. Revision Risk After Primary Adult Spinal Deformity Surgery: A Nationwide Study With Two-Year Follow-up. Spine Deform 7, 619–626 (2019). https://doi.org/10.1016/j.jspd.2018.10.006
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.10.006