Abstract
Study Design
A repeated measurement, single-center, prospective study.
Objective
The purpose of this study is to compare and contrast the benefits of walking sticks versus a walker on the trunk and lower extremity muscular control in patients with adult degenerative scoliosis (ADS).
Summary of Background Data
ADS patients demonstrate an altered gait pattern. Walking aids help maintain mobility in those patients. Whereas a walker forces patients into kyphosis, the higher grips of walking sticks allows for more upright posture, arm swing, and improved sagittal alignment.
Methods
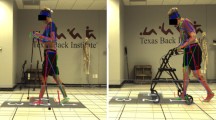
Twenty ADS patients with symptomatic degenerative scoliosis performed over-ground walking at self-selected speed under 3 testing conditions: 1) with walking sticks (WS); 2) with walker (WR); and 3) without any device (ND). Trunk and lower extremity peak muscle activation, time to peak muscle activity, muscle duration, muscle onset, and integrated electromyography (iEMG) were measured and compared.
Results
The use of WS produced increases in muscle activity in the external oblique (WS: 44.3% vs. WR: 7.4% of submaximum voluntary contraction [sMVC], p = .007) and medial gastrocnemius (WS: 78.8% vs ND: 43.7% of sMVC, p = .027) in comparison to the walker and no device, respectively. When using WS, shorter muscle activity time was observed for rectus femoris (WS: 62.9% vs. WR: 88.8% of gait cycle, p = .001), semitendinosus (WS: 64.3% vs. WR: 93.0% of gait cycle, p = .003), tibialis anterius (WS: 59.4% vs. WR: 85.1% of gait cycle, p = .001), and medial gastrocnemius (WS: 67.3% vs. WR: 98.0% of gait cycle, p = .006) in comparison to the walker.
Conclusions
The use of walking sticks can potentially promote trunk and lower extremity neuromuscular control and gait mechanics comparable to gait without any assistive devices. Although the differences in magnitudes between comparisons were small and should be cautiously interpreted on a case-by-case basis, based on this study’s results and our anecdotal experience treating patients with ADS, we recommend the use of walking sticks to assist with their gait prior to and after surgical intervention.
Level of Evidence
Level III.
Similar content being viewed by others
References
Kotwal S, Pumberger M, Hughes A, et al. Degenerative scoliosis: a review. HSS J 2011;7:257–64.
Kotwicki T, Chowanska J, Kinel E, et al. Optimal management of idiopathic scoliosis in adolescence. Adolesc Health Med Ther 2013;4:59–73.
Ploumis A, Transfledt EE, Denis F. Degenerative lumbar scoliosis associated with spinal stenosis. Spine J 2007;7:428–36.
Yang JH, Suh SW, Sung PS, et al. Asymmetrical gait in adolescents with idiopathic scoliosis. Eur Spine J 2013;22:2407–13.
Mahaudens P, Banse X, Mousny M, et al. Gait in adolescent idiopathic scoliosis: kinematics and electromyographic analysis. Eur Spine J 2009;18:512–21.
Kramers-de Quervain IA, Müller R, Stacoff A, et al. Gait analysis in patients with idiopathic scoliosis. Eur Spine J 2004;13:449–56.
Schizas CG, Quervain K, Stussi E, et al. Gait asymmetries in patients with idiopathic scoliosis using vertical forces measurement only. Eur Spine J 1998;7:95–8.
Chockalingam N, Dangerfield PH, Rahmatalla A, et al. Assessment of ground reaction force during scoliotic gait. Eur Spine J 2004; 13: 750–4.
Giakas G, Baltzopoulos V, Dangerfield PH, et al. Comparison of gait patterns between healthy and scoliotic patients using time and frequency domain analysis of ground reaction forces. Spine (Phila Pa 1976) 1996;21:2235–42.
Mahaudens P, Detrembleur C, Mousny M, et al. Gait in adolescent idiopathic scoliosis: energy cost analysis. Eur Spine J 2009;18: 1160–8.
Hopf C, Scheideckerm M, Steffanm K, et al. Gait analysis in idiopathic scoliosis before and after surgery: a comparison of the pre-and postoperative muscle activation pattern. Eur Spine J 1998;7: 6–11.
Lindh M. Energy expenditure during walking in patients with scoliosis: the effect of surgical correction. Spine 1978;3:122–34.
Haddas R, Lieberman IH. A method to quantify the cone of economy. Eur Spine J 2018;27:1178–87.
DeLuca PA, Davis 3rd RB, Ounpuu S, et al. Alterations in surgical decision making in patients with cerebral palsy based on three-dimensional gait analysis. J Pediatr Orthop 1997;17:608–14.
Ounpuu S, Davis R, DeLuca P. Joint kinetics: methods, interpretation and treatment decision-making in children with cerebral palsy and myelomeningocele. Gait Posture 1996;4:62–78.
Õunpuu S, DeLuca PA, Davis RB. The role of hip flexor and hamstring surgery on pelvic and hip motion in persons with cerebral palsy: an examination of the pre and post operative kinematics and kinetics. Gait Posture 1997;5:152.
Ko SU, Ling SM, Schreiber C, et al. Gait patterns during different walking conditions in older adults with and without knee Osteoarthritis—results from the Baltimore Longitudinal Study of Aging. Gait Posture 2011;33:205–10.
Dettman MA, Linder MT, Sepic SB. Relationship among walking performance, postural stability and functional assessments of the hemiplegic patient. Am J Phys Med 1987;66:77–90.
Patla AE. Neurobiomechanical bases for the control of human locomotion. In: Bronstein AM, Brandt T, Woollacott MH, editors. Clinical disorders of balance, posture and gaited. London: Arnold; 1996.
Hardi I, Bridenbaugh SA, Gschwind YJ, et al. The effect of three different types of walking aids on spatio-temporal gait parameters in community-dwelling older adults. Aging Clin Exp Res 2014;26: 221–8.
Marks R. The effect of restricting arm swing during normal locomotion. Biomed Sci Instrum 1997;33:209–15.
Alkjær T, Larsen PK, Pedersen G, et al. Biomechanical analysis of rollator walking. Biomed Eng Online 2006;5:2.
Willson J, Torry MR, Decker MJ, et al. Effects of walking poles on lower extremity gait mechanics. Med Sci Sports Exerc 2001;33:142–7.
Jeong YG, Jeong YJ, Kim T, et al. A randomized comparison of energy consumption when using different canes, inpatients after stroke. Clin Rehabil 2015;29:129–34.
Bechard DJ, Birmingham TB, Zecevic AA, et al. The effect of walking poles on the knee adduction moment in patients with varus gonarthrosis. Osteoarthr Cartil 2012;20:12.
Robertson GE, Caldwell GE, Hamill J, et al. Research methods in biomechanicsed. Champaign, IL: Human Kinetics; 2013.
Bogdanis GC. Effects of physical activity and inactivity on muscle fatigue. Front Physiol 2012;3:142.
Clark BC, Manini TM, Ordway NR, Ploutz-Snyder LL. Leg muscle activity during walking with assistive devices at varying levels of weight bearing. Arch Phys Med Rehabil 2004;85: 1555–60.
Schultz A, Andersson G, Ortengren R, et al. Loads on the lumbar spine. Validation of a biomechanical analysis by measurements of intradiscal pressures and myoelectric signals. J Bone Joint Surg Am 1982;64:713–20.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: RH (grants from AlphaTec Inc. and the Cervical Spine Research Society), IHL (personal fees and other from Mazor Robotics; other from Bionik Laboratories and Stryker; personal fees from Safe Orthopaedics, Globus Spine, Misonix, Medtronic, and SIBone, outside the submitted work), RSK (none).
Sources of Support: None.
IRB Approval: The study was approved by the Western Institutional Review Board for the Protection of Human Subjects (IRB approval no.: 20151780).
Rights and permissions
About this article
Cite this article
Haddas, R., Lieberman, I.H. & Kakar, R.S. A Comparison of Muscular Activity During Gait Between Walking Sticks and a Walker in Patients With Adult Degenerative Scoliosis. Spine Deform 7, 454–466 (2019). https://doi.org/10.1016/j.jspd.2018.09.067
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.09.067