Abstract
Study Design
Longitudinal cohort.
Objectives
To determine the patient-reported functional outcomes and need for related surgical procedures in a US cohort of adolescent idiopathic scoliosis (AIS) patients with minimum 20-year follow-up.
Summary of Background Data
There is limited information regarding the long-term outcomes of scoliosis treatment in the US population.
Methods
A novel population of patients who underwent pediatric treatment for AIS with minimum 20-year follow-up was identified. Search of a single-center diagnostic registry generated 337 patients who fulfilled the inclusion criteria (AIS, curve magnitude >35°, and childhood treatment with bracing, surgery, or observation from 1975 to 1992). Any additional spine surgery as well as EQ5D, ODI, SRS 22, SAQ were determined. A total of 180 patients were included (mean of 30-year follow-up, range 20–37). Childhood treatment entailed bracing (41 patients), surgery (103 patients), and observation (36 patients).
Results
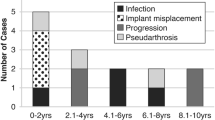
During the study period, only 1 of the 41 bracing patients underwent additional scoliosis-related spine surgery, whereas 5 of the 36 patients in the observation cohort underwent scoliosis surgery as adults. Seven of 103 childhood surgical patients required additional revision surgery as adults. Fifteen patients (4 braced, 7 fusion, and 4 observed) underwent chest wall surgery as adults. SRS scores were around 10% worse compared to population-based controls, with the exception of SRS mental health scores, which were similar to controls. Overall, 5.6% of patients were on disability, with no difference between operative and nonoperative groups.
Conclusion
We found a low rate of adult scoliosis surgery in the braced population, and a low rate of revision surgery at the 30-year follow-up in patients undergoing spine fusion for AIS between 1975 and 1992. No detected differences in patient-reported outcomes were found between the braced, surgical, and observed populations at a mean of 30 years’ follow-up.
Level of Evidence
Level III, therapeutic.
Similar content being viewed by others
References
Renshaw TS. Screening school children for scoliosis. Clin Orthop Relat Res 1988;229:26–33.
Weinstein SL. Adolescent idiopathic scoliosis: prevalence and natural history. Instr Course Lect 1989;38:115–28.
Rogala EJ, Drummond DS, Gurr J. Scoliosis: incidence and natural history. A prospective epidemiological study. J Bone Joint Surg Am 1978;60:173–6.
Shands Jr AR, Eisberg HB. The incidence of scoliosis in the state of Delaware; a study of 50,000 minifilms of the chest made during a survey for tuberculosis. J Bone Joint Surg Am 1955;37:1243–9.
Kane WJ. Scoliosis prevalence: a call for a statement of terms. Clin Orthop Relat Res 1977;126:43–6.
Bruszewski J, Kamza Z. Incidence of scoliosis based on an analysis of serial radiography [in Polish]. Chir Narzadow Ruchu Ortop Pol 1957;22:115–6.
Patynski J, Szczekot J, Szwaluk F. Scoliosis in the light of statistics [in Polish]. Chir Narzadow Ruchu Ortop Pol 1957;22:111–4.
Weinstein SL, Zavala DC, Ponseti IV. Idiopathic scoliosis: long-term follow-up and prognosis in untreated patients. J Bone Joint Surg Am 1981;63:702–12.
Aaro S, Ohlund C. Scoliosis and pulmonary function. Spine 1984;9: 220–2.
Edgar MA, Mehta MH. Long-term follow-up of fused and unfused idiopathic scoliosis. J Bone Joint Surg Br 1988;70:712–6.
Bridwell KH. Surgical treatment of idiopathic adolescent scoliosis. Spine 1999;24:2607–16.
Cuartas E, Rasouli A, O’Brien M, et al. Use of all-pedicle-screw constructs in the treatment of adolescent idiopathic scoliosis. J Am Acad Orthop Surg 2009;17:550–61.
Helenius I, Remes V, Lamberg T, et al. Long-term health-related quality of life after surgery for adolescent idiopathic scoliosis and spondylolisthesis. J Bone Joint Surg Am 2008;90:1231–9.
Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 1983;65:447–55.
Weinstein SL, Dolan LA, Spratt KF, et al. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA 2003;289:559–67.
Weinstein SL. Idiopathic scoliosis. Natural history. Spine 1986;11: 780–3.
Collis DK, Ponseti IV. Long-term follow-up of patients with idiopathic scoliosis not treated surgically. J Bone Joint Surg Am 1969;51:425–45.
Danielsson AJ, Wiklund I, Pehrsson K, et al. Health-related quality of life in patients with adolescent idiopathic scoliosis: a matched followup at least 20 years after treatment with brace or surgery. Eur Spine J 2001;10:278–88.
Danielsson AJ, Nachemson AL. Back pain and function 23 years after fusion for adolescent idiopathic scoliosis: a case-control study-—part II. Spine 2003;28:E373–83.
Danielsson AJ, Nachemson AL. Back pain and function 22 years after brace treatment for adolescent idiopathic scoliosis: a case-control study—part I. Spine 2003;28:2078–85; discussion 86.
Danielsson AJ, Romberg K, Nachemson AL. Spinal range of motion, muscle endurance, and back pain and function at least 20 years after fusion or brace treatment for adolescent idiopathic scoliosis: a case-control study. Spine 2006;31:275–83.
Pehrsson K, Larsson S, Oden A, et al. Long-term follow-up of patients with untreated scoliosis. A study of mortality, causes of death, and symptoms. Spine 1992;17:1091–6.
Verma K, Lonner B, Hoashi JS, et al. Demographic factors affect Scoliosis Research Society-22 performance in healthy adolescents: a comparative baseline for adolescents with idiopathic scoliosis. Spine 2010;35:2134–9.
Denoel C, Aguirre MF, Bianco G, et al. Idiopathic scoliosis and breast asymmetry. J Plast Reconstr Aesthet Surg 2009;62:1303–8.
Normelli H, Sevastik JA, Ljung G, et al. The symmetry of the breasts in normal and scoliotic girls. Spine 1986;11:749–52.
Fowles JV, Drummond DS, L’Ecuyer S, et al. Untreated scoliosis in the adult. Clin Orthop Relat Res 1978;134:212–7.
Baldus C, Bridwell K, Harrast J, et al. The Scoliosis Research Society Health-Related Quality of Life (SRS-30) age-gender normative data: an analysis of 1346 adult subjects unaffected by scoliosis. Spine 2011;36:1154–62.
Danielsson AJ, Nachemson AL. Childbearing, curve progression, and sexual function in women 22 years after treatment for adolescent idiopathic scoliosis: a case-control study. Spine 2001;26:1449–56.
Danielsson AJ, Hasserius R, Ohlin A, et al. Body appearance and quality of life in adult patients with adolescent idiopathic scoliosis treated with a brace or under observation alone during adolescence. Spine 2012;37:755–62.
Danielsson AJ, Hasserius R, Ohlin A, et al. Health-related quality of life in untreated versus brace-treated patients with adolescent idiopathic scoliosis: a long-term follow-up. Spine 2010;35:199–205.
Danielsson AJ, Hasserius R, Ohlin A, et al. A prospective study of brace treatment versus observation alone in adolescent idiopathic scoliosis: a follow-up mean of 16 years after maturity. Spine 2007;32:2198–207.
Simony A, Hansen EJ, Carreon LY, et al. Health-related quality-of-life in adolescent idiopathic scoliosis patients 25 years after treatment. Scoliosis 2015; 10:22.
Simony A, Christensen SB, Carreon LY, et al. Radiological outcomes in adolescent idiopathic scoliosis patients more than 22 years after treatment. Spine Deform 2015;3:436–9.
Mariconda M, Galasso O, Barca P, et al. Minimum 20-year follow-up results of Harrington rod fusion for idiopathic scoliosis. Eur Spine J 2005;14:854–61.
Niemeyer T, Bovingloh AS, Grieb S, et al. Low back pain after spinal fusion and Harrington instrumentation for idiopathic scoliosis. Int J Orthop 2005;29:47–50.
Helenius I, Remes V, Yrj€onen T, et al. Comparison of long-term function and radiological outcomes after Harrington instrumentation and spondylodesis in adolescent idiopathic scoliosis: a review of 78 patients. Spine 2002;15:176–80.
Paonessa KJ, Engler GL. Back pain and disability after Harrington rod fusion to the lumbar spine for scoliosis. Spine (Phila Pa 1976) 1992; 17(8 suppl):S249–53.
Holman J, Carroll KL, Murray KA, et al. Long-term follow up of open reduction surgery for developmental dislocation of the hip. J Pediatr Orthop 2012;32:121–4.
Larson AN, Sucato DJ, Herring JA, et al. A prospective multicenter study of Legg-Calvé-Perthes disease: functional and radiographic outcomes of nonoperative treatment at a mean follow-up of twenty years. J Bone Joint Surg Am 2012;94:584–92.
Newton PO, Marks MC, Bastrom TP, et al. Surgical treatment of Lenke 1 main thoracic idiopathic scoliosis: results of a prospective, multicenter study. Spine 2013;38:328–38.
Carreon LY, Sanders JO, Diab M, et al. Patient satisfaction after surgical correction of adolescent idiopathic scoliosis. Spine 2011;36:965–8.
Campos M, Dolan L, Weinstein S. Unanticipated revision surgery in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2012;37: 1048–53.
Mignemi M, Tran D, Ramo B, Richards BS. Repeat surgical interventions following “definitive” instrumentation and fusion for idiopathic scoliosis: 25-year update. Spine Deform 2018;6:409–16.
Healthcare Cost and Utilization Project: HCUP Projections Mortality/Orthopedic Procedures 2003 to 2012, Report #2012-03. Available at: https://www.hcup-us.ahrq.gov/reports/projections/2012-03.pdf.
Weinstein JN, Lurie JD, Olson PR, et al. United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine 2006;31:2707–14.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: ANL (grants from Scoliosis Research Society, during the conduct of the study; personal fees from K2M and Orthopediatrics, outside the submitted work), FB (none), AA (none), YMB (none), VT (none), DWP (none), MJY (none).
Funding: This study was funded by the Directed Research Grant from the Scoliosis Research Society.
IRB approval: Mayo Clinic IRB: 16-008732 and 12-000004.
Rights and permissions
About this article
Cite this article
Larson, A.N., Baky, F., Ashraf, A. et al. Minimum 20-Year Health-Related Quality of Life and Surgical Rates After the Treatment of Adolescent Idiopathic Scoliosis. Spine Deform 7, 417–427 (2019). https://doi.org/10.1016/j.jspd.2018.09.003
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.09.003