Abstract
Design
Retrospective comparative study.
Objective
The purpose of this study is to measure SSI outcomes before and after implementation of our center’s multidisciplinary clinical pathway protocol for high-risk spinal surgery.
Background
Surgical site infections (SSIs) after spinal fusion harm patients and are associated with significant health care costs. Given the high rate of SSI in neuromuscular populations, there is a rationale to develop infection prevention strategies.
Methods
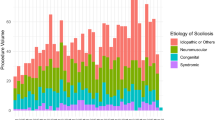
An institutional clinical pathway was created in 2012 and based on nationally published Best Practice Guidelines as well as hospital practices with a goal of reducing the rate of deep SSI in high-risk patients. Patient and procedure characteristics were compared prior to (2008–2011) and after (2012–2016) implementation of the pathway. Logistic regression using penalized maximum likelihood was used to assess differences in rate of infection before and after implementation.
Results
Cohorts of 132 and 115 high-risk patients were analyzed before and after pathway implementation. Rate of deep infections decreased from 8% to 1% of patients (p = .005). Preoperative antibiotics were dosed within 1 hour in 90% of the postpathway cohort. Redosing was successful in 94% of patients for first redose and 79% for second redose. Betadine irrigation was used in 76% of cases and vancomycin administered in 86%. Multivariable analysis determined that instances of compliant antibiotics dosing had 63% lower odds of infection compared with instances of noncompliance (p = .04).
Conclusions
Implementation of a multidisciplinary pathway aimed to reduce infection in patients at high risk for SSI after spinal fusion led to a significant reduction in deep SSI rate. It is impossible to attribute the drop in the deep SSI rate to any one factor. Our results demonstrate that adherence to a protocol using multiple strategies to reduce infection results in a lower SSI rate, lower care costs, and improved patient-related outcomes.
Level of Evidence
Level III.
Similar content being viewed by others
References
Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med 2013;173:2039–46.
Merkow RP, Ju MH, Chung JW, et al. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA 2015;313:483–95.
Hedequist D, Haugen A, Hresko T, Emans J. Failure of attempted implant retention in spinal deformity delayed surgical site infections. Spine (Phila Pa 1976) 2009;34:60–4.
Sponseller PD, Shah SA, Abel MF, et al. Infection rate after spine surgery in cerebral palsy is high and impairs results: multicenter analysis of risk factors and treatment. Clin Orthop Relat Res 2010;468:711–6.
Cahill PJ, Warnick DE, Lee MJ, et al. Infection after spinal fusion for pediatric spinal deformity: thirty years of experience at a single institution. Spine (Phila Pa 1976) 2010;35:1211–7.
Benson ER, Thomson JD, Smith BG, Banta JV. Results and morbidity in a consecutive series of patients undergoing spinal fusion for neuromuscular scoliosis. Spine (Phila Pa 1976) 1998;23: 2308–17; discussion 2318.
Banit DM, Iwinski Jr HJ, Talwalkar V, Johnson M. Posterior spinal fusion in paralytic scoliosis and myelomeningocele. J Pediatr Orthop 2001;21:117–25.
Geiger F, Parsch D, Carstens C. Complications of scoliosis surgery in children with myelomeningocele. Eur Spine J 1999;8:22–6.
Stella G, Ascani E, Cervellati S, et al. Surgical treatment of scoliosis associated with myelomeningocele. Eur J Pediatr Surg 1998;8(suppl 1):22–5.
Borkhuu B, Borowski A, Shah SA, et al. Antibiotic-loaded allograft decreases the rate of acute deep wound infection after spinal fusion in cerebral palsy. Spine (Phila Pa 1976) 2008;33:2300–4.
Tsirikos AI, Lipton G, Chang WN, et al. Surgical correction of scoliosis in pediatric patients with cerebral palsy using the unit rod instrumentation. Spine (Phila Pa 1976) 2008;33:1133–40.
Teli MG, Cinnella P, Vincitorio F, et al. Spinal fusion with Cotrel-Dubousset instrumentation for neuropathic scoliosis in patients with cerebral palsy. Spine (Phila Pa 1976) 2006;31:E441–7.
Szoke G, Lipton G, Miller F, et al. Wound infection after spinal fusion in children with cerebral palsy. J Pediatr Orthop 1998;18: 727–33.
Dias RC, Miller F, Dabney K, et al. Surgical correction of spinal deformity using a unit rod in children with cerebral palsy. J Pediatr Orthop 1996;16:734–40.
Barie PS, Eachempati SR. Surgical site infections. Surg Clin North Am 2005;85:1115–35. viii–ix.
Wenzel RP. Health care-associated infections: major issues in the early years of the 21st century. Clin Infect Dis 2007;45(suppl l):S85–8.
Ho C, Skaggs DL, Weiss JM, Tolo VT. Management of infection after instrumented posterior spine fusion in pediatric scoliosis. Spine (Phila Pa 1976) 2007;32:2739–44.
Glotzbecker MP, Garg S, Akbarnia BA, et al. Surgeon practices regarding infection prevention for growth friendly spinal procedures. J Child Orthop 2014;8:245–50.
Glotzbecker MP, Vitale MG, Shea KG, et al. Surgeon practices regarding infection prevention for pediatric spinal surgery. J Pediatr Orthop 2013;33:694–9.
Glotzbecker MP, Riedel MD, Vitale MG, et al. What’s the evidence? Systematic literature review of risk factors and preventive strategies for surgical site infection following pediatric spine surgery. J Pediatr Orthop 2013;33:479–87.
Newman K, Ponsky T, Kittle K. Appendicitis 2000: variability in practice, outcomes, and resource utilization at thirty pediatric hospitals. J Pediatr Surg 2003;38:372–9; discussion 372–9.
Vitale MG, Riedel MD, Glotzbecker MP, et al. Building consensus: development of a Best Practice Guideline (BPG) for surgical site infection (SSI) prevention in high-risk pediatric spine surgery. J Pediatr Orthop 2013;33:471–8.
National Healthcare Safety Network, Centers for Disease Control and Prevention. Surgical site infection (SSI) event. 2017. Available at: http://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf.
McMaster MJ. Anterior and posterior instrumentation and fusion of thoracolumbar scoliosis due to myelomeningocele. J Bone Joint Surg Br 1987;69:20–5.
Osebold WR, Mayfield JK, Winter RB, Moe JH. Surgical treatment of paralytic scoliosis associated with myelomeningocele. J Bone Joint Surg Am 1982;64:841–56.
Berry JG, Glotzbecker MP, Rodean J, et al. Comorbidities and complications of spinal fusion for scoliosis. Pediatrics 2017, 1–10;139.
Mistovich RJ, Jacobs LJ, Campbell RM, et al. Infection control in pediatric spinal deformity surgery: a systematic and critical analysis review. JBJS Rev 2017;5:e3.
Chundamala J, Wright JG. The efficacy and risks of using povidoneiodine irrigation to prevent surgical site infection: an evidence-based review. Can J Surg 2007;50:473–81.
Cheng MT, Chang MC, Wang ST, et al. Efficacy of dilute betadine solution irrigation in the prevention of postoperative infection of spinal surgery. Spine (Phila Pa 1976) 2005;30:1689–93.
Menekse G, Kuscu F, Suntur BM, et al. Evaluation of the time-dependent contamination of spinal implants: prospective randomized trial. Spine (Phila Pa 1976) 2015;40:1247–51.
Bible JE, O’Neill KR, Crosby CG, et al. Implant contamination during spine surgery. Spine J 2013;13:637–40.
Halpin RJ, Sugrue PA, Gould RW, et al. Standardizing care for high-risk patients in spine surgery: the Northwestern high-risk spine protocol. Spine 2010;35:2232–8.
Sethi RK, Pong RP, Leveque JC, et al. The Seattle Spine Team approach to adult deformity surgery: a systems-based approach to perioperative care and subsequent reduction in perioperative complication rates. Spine Deform 2014;2:95–103.
Pronovost P, Weast B, Rosenstein B, et al. Implementing and validating a comprehensive unit-based safety program. J Patient Saf 2005;1:33–40.
Mackenzie WS, McLeod L, Wang K, et al. Team approach: preventing surgical site infections in pediatric scoliosis surgery. JBJS Rev 2018;6:e2.
Berry JG, Glotzbecker M, Rodean J, et al. Perioperative spending on spinal fusion for scoliosis for children with medical complexity. Pediatrics 2017;140:e20171233.
Milstone AM, Maragakis LL, Townsend T, et al. Timing of preoperative antibiotic prophylaxis: a modifiable risk factor for deep surgical site infections after pediatric spinal fusion. Pediatr Infect Dis J 2008;27:704–8.
Kang DG, Holekamp TF, Wagner SC, Lehman Jr RA. Intrasite vancomycin powder for the prevention of surgical site infection in spine surgery: a systematic literature review. Spine J 2015;15:762–70.
Kanj WW, Flynn JM, Spiegel DA, et al. Vancomycin prophylaxis of surgical site infection in clean orthopedic surgery. Orthopedics 2013;36:138–46.
Sethi R, Yanamadala V, Burton DC. Using lean process improvement to enhance safety and value in orthopaedic surgery: the case of spine surgery. J Am Acad Orthop Surg 2017;25:e244–50.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: MG (other from DePuy Synthes, Medtronic, Zimmer BioMet, NuVasive, and Orthobullets; other from Member of Growing Spine Study Group [GSSG], Children Spine Study Group [CSSG], The Harms Study Group [HSG], outside the submitted work), MT (none), PM (none), JB (none), MPH, LC (none), AG (none), MEM (none), MTH (nonfinancial support from Medtronics and NuVasive; personal fees from Boston Brace international, outside the submitted work; board of directors of the Pediatric Orthopaedic Society of North America [POSNA]; and committee chair, Scoliosis Research Society), SG (grants from Scoliosis Research Society; other from Octapharma, outside the submitted work), JE (personal fees from Biomet, DePuy, Medtronic Sofamor Danek, and Synthes; other from Journal of Pediatric Orthopedics, outside the submitted work), RB (none), BS (nonfinancial support from Orthopediatrics; other from American Academy of Orthopaedic Surgeons [AAOS], Orthopaedic Research Society, POSNA, and Scoliosis Research Society, outside the submitted work), DH (other from AAOS and POSNA, outside the submitted work).
IRB Approval:
No funding was received for this work from any of the following organizations: National Institutes of Health (NIH); Welcome Trust; Howard Hughes Medical Institute (HHM).
Rights and permissions
About this article
Cite this article
Glotzbecker, M., Troy, M., Miller, P. et al. Implementing a Multidisciplinary Clinical Pathway Can Reduce the Deep Surgical Site Infection Rate After Posterior Spinal Fusion in High-Risk Patients. Spine Deform 7, 33–39 (2019). https://doi.org/10.1016/j.jspd.2018.06.010
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.06.010