Abstract
Objective
We investigated the relationship between cross-sectional area (CSA) of paravertebral muscle and trunk tilt at standing and walking in adult spinal deformity (ASD) surgery.
Summary of Background Data
Although the importance of back muscles for the development of spinal kyphosis was well described, the influence on maintaining the sagittal balance was unclear.
Methods
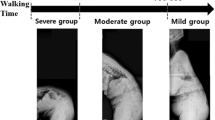
Forty-five female patients (mean age, 68.8 years) with ASD were studied. We measured sagittal vertical axis [SVA], pelvic tilt [PT], and pelvic incidence—lumbar lordosis [PI-LL]) by lateral spine radiograph. For the assessment of trunk tilt standing-trunk tilt angle (STA) by lateral standing radiograph, gait-trunk tilt angle (GTA) by lateral gait images, and the increasing trunk tilt angle (ITA) by subtracting the STA from the GTA were calculated. Using L1/2 and L4/5 axial MRI, the CSAs of bilateral multifidus muscles (MF) and elector spinae (ES) removed fat by Image J software were calculated. We examined the correlation between trunk tilt angle (STA, GTA, and ITA) and spinopelvic parameters (SVA, PT, and PI minus LL) and also the correlation among muscle CSA, trunk tilt angle (STA, GTA, and ITA), and Oswestry Disability Index (ODI).
Results
The mean STA, GTA, and ITA were 4.2°, 13.0°, and 8.8°, respectively. The CSAs of back muscles were 278 mm2 at L1/2 MF, 1,687 mm2 at L1/2 ES, 636 mm2 at L4/5 MF, and 1,355 mm2 at L4/5 ES, respectively. Trunk tilt angle had significant relations with spinopelvic parameters. Concerning about muscle CSA, significant correlations were observed between STA and L4/5 MF (r = –0.517), GTA and L1/2 ES (r = –0.461) and L4/5 MF (r = –0.476), and ITA and L1/2 ES(r = –0.429). ODI showed significant correlation with STA and GTA.
Conclusions
Paravertebral muscles were crucial to keep upright posture during walking as well as standing.
Similar content being viewed by others
References
Miyakoshi N, Hongo M, Maekawa S, et al. Back extensor strength and lumbar spinal mobility are predictors of quality of life in patients with postmenopausal osteoporosis. Osteoporos Int 2007;18:1397–403.
Sinaki M, Brey RH, Hughes CA, et al. Balance disorder and increased risk of falls in osteoporosis and kyphosis: significance of kyphotic posture and muscle strength. Osteoporos Int 2005;16:1004–10.
Hongo M, Miyakoshi N, Shimada Y, et al. Association of spinal curve deformity and back extensor strength in elderly women with osteoporosis in Japan and the United States. Osteoporos Int 2012;23:1029–34.
Miyakoshi N, Hongo M, Maekawa S, et al. Factors related to spinal mobility in patients with postmenopausal osteoporosis. Osteoporos Int 2005;16:1871–4.
Kasukawa Y, Miyakoshi N, Hongo M, et al. Relationships between falls, spinal curvature, spinal mobility and back extensor strength in elderly people. J Bone Miner Metab 2010;28:82–7.
Moal B, Bronsard N, Raya JG, et al. Volume and fat infiltration of spino-pelvic musculature in adults with spinal deformity. World J Orthop 2015;6:727–37.
Yagi M, Hosogane N, Watanabe K, et al. The paravertebral muscle and psoas for the maintenance of global spinal alignment in patient with degenerative lumbar scoliosis. Spine J 2016;16:451–8.
Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine 2005;30:2024–9.
Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine 2012;37:1077–82.
Lafage V, Schwab F, Skalli W, et al. Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine 2008;33:1572–8.
Arima H, Yamato Y, Hasegawa T, et al. Discrepancy between standing posture and sagittal balance during walking in adult spinal deformity patients. Spine 2017;42:E25–30.
Bae J, Theologis AA, Jang JS, et al. Impact of fatigue on maintenance of upright posture: dynamic assessment of sagittal spinal deformity parameters after walking 10 minutes. Spine 2017;42:733–9.
Lee JC, Cha JG, Kim Y, et al. Quantitative analysis of back muscle degeneration in the patients with the degenerative lumbar flat back using a digital image analysis: comparison with the normal controls. Spine 2008;33:318–25.
Roussouly P, Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 2010;19:1824–36.
Protopsaltis T, Schwab F, Bronsard N, et al. The T1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am 2014;96:1631–40.
Obeid I, Boissiere L, Yilgor C, et al. Global tilt: a single parameter incorporating spinal and pelvic sagittal parameters and least affected by patient positioning. Eur Spine J 2016;25:3644–9.
Shiba Y, Taneichi H, Inami S, et al. Dynamic global sagittal alignment evaluated by three-dimensional gait analysis in patients with degenerative lumbar kyphoscoliosis. Eur Spine J 2016;25:2572–9.
Dubousset J. Reflections of an orthopaedic surgeon on patient care and research into the condition of scoliosis. J Pediatr Orthop 2011;31: S1–8.
Hanada EY, Johnson M, Hubley-Kozey C. A comparison of trunk muscle activation amplitudes during gait in older adults with and without chronic low back pain. PMR 2011;3:920–8.
Marras WS, Jorgensen MJ, Granata KP, et al. Female and male trunk geometry: size and prediction of the spine loading trunk muscles derived from MRI. Clin Biomech 2001;16:38–46.
Belavý DL, Armbrecht G, Richardson CA, et al. Muscle atrophy and changes in spinal morphology: is the lumbar spine vulnerable after prolonged bed-rest? Spine 2011;36:137–45.
Shahidi B, Parra CL, Berry DB, et al. Contribution of lumbar spine pathology and age to paraspinal muscle size and fatty infiltration. Spine 2017;42:616–22.
Hides JA, Richardson CA, Jull GA. Magnetic resonance imaging and ultrasonography of the lumbar multifidus muscle. Comparison of two different modalities. Spine 1995;20:54–8.
Stokes MJ, Cooper RG, Morris G, et al. Selective changes in multifidus dimensions in patients with chronic low back pain. Eur Spine J 1992; 1: 38–42.
Lee HI, Song J, Lee HS, et al. Association between cross-sectional areas of lumbar muscles on magnetic resonance imaging and chronicity of low back pain. Ann Rehabil Med 2011;35:852–9.
Barrey C, Roussouly P, Le Huec JC, et al. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J 2013;22:S834–41.
Katzman WB, Sellmeyer DE, Stewart AL, et al. Changes in flexed posture, musculoskeletal impairments, and physical performance after group exercise in community-dwelling older women. Arch Phys Med Rehabil 2007;88:192–9.
Ball JM, Cagle P, Johnson BE, et al. Spinal extension exercises prevent natural progression of kyphosis. Osteoporos Int 2008;20:481.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: TB (none), HA (none), TH (none), YY (none), DT (other from Donated Fund Laboratory, personal fees from Journal of Bone and Joint Surgery, outside the submitted work), GY (none), TY (none), SO (other from Donated Fund Laboratory, outside the submitted work), YM (none), HU (none), YM (none).
The manuscript submitted does not contain information about medical device(s)/drug(s).
This study was approved by the Institutional Review Board of Hamamatsu University School of Medicine. All study participants provided informed consent, and the study design was approved by the appropriate ethics review boards.
Rights and permissions
About this article
Cite this article
Banno, T., Arima, H., Hasegawa, T. et al. The Effect of Paravertebral Muscle on the Maintenance of Upright Posture in Patients With Adult Spinal Deformity. Spine Deform 7, 125–131 (2019). https://doi.org/10.1016/j.jspd.2018.06.008
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.06.008