Abstract
Study Design
Retrospective review of a prospective cohort.
Objective
To identify patient and surgical factors that alter the length of postoperative intensive care unit (ICU) stays after spinal fusion/ instrumentation in patients with neuromuscular scoliosis secondary to cerebral palsy (CP).
Summary of Background Data
High perioperative complication rates in patients with CP contribute to the practice of utilizing the ICU postoperatively for monitoring. However, this is costly and little is known regarding which patients truly need this increased acuity of care.
Methods
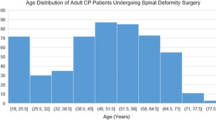
A prospective, multicenter database was queried for patients with CP who underwent spinal fusion and instrumentation. Patients with an ICU length of stay (LOS) ⩽1 day were assumed to not have required postoperative ICU admission. Demographic and surgical characteristics were compared between those with ICU LOS of ⩽1 day versus > 1 day. A classification and regression tree (CART) analysis was utilized to create a decision algorithm for postoperative ICU admission.
Results
Three hundred twenty-four patients were identified with a mean ICU LOS of 4.7 days (range 0–47). Sixty-eight patients (21%) had an ICU LOS ⩽1 day and 256 patients (79%) had an ICU LOS >1 day. CART analysis demonstrated that the institution where the surgery was performed was the primary predictor with two groups: sites that almost routinely had ICU stay > 1 day (92%) and those that were split (50.5% > 1 day). In the latter group, an operative time greater than 4 hours was a risk factor for a longer ICU stay.
Conclusion
Because of their heterogeneous makeup, CP patients should be evaluated individually and their postoperative disposition should not be based on institutional tradition but instead on objective surgical factors. For those patients with surgical times less than 4 hours, discussions should be held regarding the safety of a postoperative disposition to a regular floor.
Level of Evidence
Level III.
Similar content being viewed by others
References
Blair E. Epidemiology of the cerebral palsies. Orthop Clin North Am 2010;41:441–55.
Driscoll SW, Skinner J. Musculoskeletal complications of neuromuscular disease in children. Phys Med Rehabil Clin N Am 2008;19: 163–94. viii.
Brooks JT, Sponseller PD. What’s new in the management of neuromuscular scoliosis. J Pediatr Orthop 2016;36:627–33.
Sharma S, Wu C, Andersen T, et al, et al. Prevalence of complications in neuromuscular scoliosis surgery: a literature meta-analysis from the past 15 years. Eur Spine J 2013;22:1230–49.
Samdani AF, Belin EJ, Bennett JT, et al. Major perioperative complications after spine surgery in patients with cerebral palsy: assessment of risk factors. Eur Spine J 2016;25:795–800.
Jain A, Sponseller PD, Shah SA, et al. Incidence of and risk factors for loss of 1 blood volume during spinal fusion surgery in patients with cerebral palsy. J Pediatr Orthop 2017;37:e484–7.
Diefenbach C, Ialenti MN, Lonner BS, et al. Hospital cost analysis of neuromuscular scoliosis surgery. Bull Hosp Jt Dis 2013;71:272–7.
Breiman L, Friedman J, Stone C, et al. Classification and regression trees. Boca Raton, FL: Chapman and Hall/CRC; 1984.
Jain A, Sponseller PD, Shah SA, et al. Subclassification of GMFCS Level-5 cerebral palsy as a predictor of complications and health-related quality of life after spinal arthrodesis. J Bone Joint Surg Am 2016;98:1821–8.
Haber LL, Womack ED, Sathyamoorthy M, et al. Who needs a pediatric intensive care unit after posterior spinal fusion for adolescent idiopathic scoliosis? Spine Deform 2018;6:137–40.
Abu-Kishk I, Kozer E, Hod-Feins R, et al. Pediatric scoliosis surgery—is postoperative intensive care unit admission really necessary? Paediatr Anaesth 2013 ; 23:271–7.
Shan LQ, Skaggs DL, Lee C, et al. Intensive care unit versus hospital floor: a comparative study of postoperative management of patients with adolescent idiopathic scoliosis. J Bone Joint Surg Am 2013;95:e40.
Toovey R, Harvey A, Johnson M, et al. Outcomes after scoliosis surgery for children with cerebral palsy: a systematic review. Dev Med Child Neurol 2017;59:690–8.
Milbrandt EB, Kersten A, Rahim MT, et al. Growth of intensive care unit resource use and its estimated cost in Medicare. Crit Care Med 2008;36:2504–10.
Evans J, Kobewka D, Thavorn K, et al. The impact of reducing intensive care unit length of stay on hospital costs: evidence from a tertiary care hospital in Canada. Can J Anaesth 2018;65:627–35.
Bendon AA, George KA, Patel D. Perioperative complications and outcomes in children with cerebral palsy undergoing scoliosis surgery. Paediatr Anaesth 2016;26:970–5.
Nishnianidze T, Bayhan IA, Abousamra O, et al. Factors predicting postoperative complications following spinal fusions in children with cerebral palsy scoliosis. Eur Spine J 2016;25:627–34.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
This study was conducted at Rady Children’s Hospital, San Diego, CA.
Author disclosures: JTB (grants from OMeGA Medical Grants Association and Setting Scoliosis Straight Foundation, during the conduct of the study), BY (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; grants and personal fees from K2M and DePuy Synthes Spine; personal fees from NuVasive, Medtronic, Orthopediatrics, Stryker, and Globus; grants from Setting Scoliosis Straight Foundation, outside the submitted work; in addition, BY has a patent K2M with royalties paid), CEB (grants from Setting Scoliosis Straight Foundation, during the conduct of the study), TPB (grants from Setting Scoliosis Straight Foundation to her institution, during the conduct of the study), PDS (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; personal fees from DePuy Synthes Spine, personal fees from Globus, outside the submitted work), SAS (grants from Setting Scoliosis Straight Foundation from DePuy Synthes Spine and K2M in support of Harms Study Group research, during the conduct of the study; personal fees from DePuy Synthes Spine and K2M, outside the submitted work), AS (grants and other from Setting Scoliosis Straight Foundation, during the conduct of the study; personal fees from DePuy Synthes Spine, Ethicon, Globus Medical, Misonix, Stryker, and Zimmer Biomet; other from Scoliosis Research Society and Children’s Spine Study Group, outside the submitted work), PJC (personal fees from Biogen, Inc. and NuVasive, Inc., outside the submitted work; and board or committee member, AAOS; editorial or governing board, Journal of Bone and Joint Surgery—American and Spine Deformity; board or committee member, Pediatric Orthopaedic Society of North America; board or committee member, Scoliosis Research Society), FM (grants from Setting Scoliosis Straight Foundation, during the conduct of the study), PON (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; grants and other from Setting Scoliosis Straight Foundation; other from Rady Children’s Specialists; grants, personal fees, and nonfinancial support from DePuy Synthes Spine; grants and other from SRS; grants from EOS imaging; personal fees from Thieme Publishing; grants from NuVasive; other from Electrocore; personal fees from Cubist; other from International Pediatric Orthopedic Think Tank; grants, nonfinancial support, and other from Orthopediatrics; grants, personal fees, and nonfinancial support from K2M; grants and nonfinancial support from Alphatech, outside the submitted work; in addition, PON has a patent “Anchoring Systems and Methods for Correcting Spinal Deformities” [8540754] with royalties paid to DePuy Synthes Spine, a patent “Low Profile Spinal Tethering Systems” [8123749] licensed to DePuy Spine, Inc., a patent “Screw Placement Guide” [7981117] licensed to DePuy Spine, Inc., a patent “Compressor for Use in Minimally Invasive Surgery” [7189244] licensed to DePuy Spine, Inc., and a patent “Posterior Spinal Fixation” pending to K2M), Harms Study Group (grants from DePuy Synthes Spine and K2M, Inc., during the conduct of the study; grants from EOS Imaging, Zimmer Biomet, Medtronic Spine, Ellipse, SpineGuard, Globus, Stryker, NuVasive, Mazor Robotics, and OrthoPediatrics, outside the submitted work).
IRB approval was obtained for this study.
Rights and permissions
About this article
Cite this article
Brooks, J.T., Yaszay, B., Bartley, C.E. et al. Do All Patients With Cerebral Palsy Require Postoperative Intensive Care Admission After Spinal Fusion?. Spine Deform 7, 112–117 (2019). https://doi.org/10.1016/j.jspd.2018.06.003
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.06.003