Abstract
Introduction
Informed decision making for operative treatment of the skeletally mature adolescent idiopathic scoliosis (AIS) patient meeting surgical indications requires a discussion of differences in operative morbidity in adult scoliosis versus AIS. This study evaluated differences in operative data and outcomes between AIS and adult scoliosis patients based on an estimated natural history of curve progression.
Methods
Twenty-eight adult scoliosis patients (43.7 ± 15.8 years; 93% F) were 1:2 matched with 56 (Risser 4/5) AIS patients (15.7 ± 2.1 years) based on gender and curve type as vetted by 5 surgeons’ consensus in committee. Curve progression of 0.3°/year for the first 10 years following skeletal maturity and a 0.5°/year thereafter was assumed to estimate curve progression from AIS to adulthood for the adult counterpart. Operative data, complications, and quality of life (Scoliosis Research Society [SRS–22r] questionnaire) measures were evaluated, with a minimum 2-year follow-up.
Results
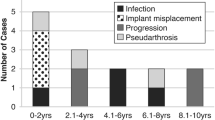
Postoperative major Cobb and percentage correction were similar between adult versus AIS, whereas operative time, percentage estimated blood loss (EBL; % total blood volume), length of hospital stay (LOS), and total spine levels fused were greater for adult patients (p < .05). No difference was found in EBL, operative time, or LOS when normalized by levels fused. Ten (36%) adult scoliosis patients were fused to the pelvis compared with none in AIS (p < .0001). Major complication rate was higher for adult versus AIS (25% vs. 5.4%; p < .05). Preoperative SRS-22r scores were worse for adult patients; however, they demonstrated greater improvement in SRS-22r than the AIS cohort at final follow-up. A higher percentage of adult patients reached the MCID in self-image domain than the AIS patients (92.3% vs. 61.8%; p = .0040).
Conclusion
Treatment of the adult scoliosis patient who has undergone an estimated natural history of progression is characterized by greater levels fused, operative time, and higher complication rates than the AIS counterpart. Longer-term follow-up of AIS is needed to define the benefits of early intervention of relatively asymptomatic adolescent patients versus late treatment of symptomatic disease in the adult.
Similar content being viewed by others
References
Available at: http://etext.srs.org/book/ (last access on 08/02/2016).
Weiss HR. Adolescent idiopathic scoliosis (AIS)—an indication for surgery? A systematic review of the literature. Disabil Rehabil 2008;30:799–807.
Weiss HR, Marc Moramarco M. Indication for surgical treatment in patients with adolescent Idiopathic Scoliosis—a critical appraisal. Patient Saf Surg 2013;7:17.
Negrini S. Approach to scoliosis changed due to causes other than evidence: patients call for conservative (rehabilitation) experts to join in team orthopedic surgeons. Disabil Rehabil 2008;30:731–41.
Westrick ER, Ward WT. Adolescent idiopathic scoliosis: 5-year to 20-year evidence-based surgical results. J Pediatr Orthop 2011;31(1 suppl):S61–8.
Weinstein SL, Zavala DC, Ponseti IV. Idiopathic scoliosis. Long term follow up and prognosis in untreated patients. J Bone Joint Surg Am 1981;63:702–12.
Weinstein SL. Idiopathic scoliosis. Natural history. Spine (Phila Pa 1976) 1986;11:780–3.
Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 1983;65:447–55.
Weinstein SL, Dolan LA, Spratt KF, et al. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA 2003;289:559–67.
Mayo NE, Goldberg MS, Poitras B, et al. The Ste-Justine Idiopathic Scoliosis Cohort Study. Part III: back pain. Spine (Phila Pa 1976) 1994;19:1573–81.
Ascani E, Bartolozzi P, Logroscino A, et al. Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine (Phila Pa 1976) 1986;11:784–9.
Mankin H, Graham J, Schauk J. Cardiopulmonary function in mild and moderate scoliosis. J Bone Joint Surg Am 1964;46:53–62.
Goldberg MS, Mayo NE, Poitras B, et al. The Ste-Justine Adolescent Idiopathic Scoliosis Cohort Study: Part II: perception of health, self and body image, and participation in physical activities. Spine (Phila Pa 1976) 1994;19:1562–72.
Danielsson AJ, Nachemson AL. Radiological findings and curve progression 22 years after treatment for adolescent idiopathic scoliosis: comparison of brace and surgical treatment with a matching control group of straight individuals. Spine (Phila Pa 1976) 2001;26:516–25.
Sponseller PD, Cohen MS, Nachemson AL, et al. Results of surgical treatment of adults with idiopathic scoliosis. J Bone Joint Surg Am 1987;69:667–75.
Dickson JH, Mirkovic S, Noble PC, et al. Results of operative treatment of idiopathic scoliosis in adults. J Bone Joint Surg Am 1995;77: 513–23.
Fon GT, Pitt MJ, Thies Jr AC. Thoracic kyphosis: range in normal subjects. AJR Am J Roentgenol 1980;134:979–83.
Crawford 3rd CH, Glassman SD, Bridwell KH, et al. The minimum clinically important difference in SRS-22R total score, appearance, activity and pain domains after surgical treatment of adult spinal deformity. Spine (Phila Pa 1976) 2015;40:377–81.
Carreon LY, Sanders JO, Diab M, et al; Spinal Deformity Study Group. The minimum clinically important difference in Scoliosis Research Society-22 Appearance, Activity, And Pain domains after surgical correction of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2010;35:2079–83.
Bridwell KH, Shufflebarger HL, Lenke LG, et al. Parents’ and patients’ preferences and concerns in idiopathic adolescent scoliosis: a cross-sectional preoperative analysis. Spine (Phila Pa 1976) 2000;25:2392–9.
Auerbach JD, Lonner BS, Errico TJ, et al. Quantification of intradiscal pressures below thoracolumbar spinal fusion constructs: is there evidence to support “saving a level”? Spine (Phila Pa 1976) 2012;37:359–66.
Marks M, Newton PO, Petcharaporn M, et al. Postoperative segmental motion of the unfused spine distal to the fusion in 100 patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2012;37:826–32.
Green DW, Lawhorne 3rd TW, Widmann RF, et al. Long-term magnetic resonance imaging follow-up demonstrates minimal transitional level lumbar disc degeneration after posterior spine fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2011;36:1948–54.
Kepler CK, Meredith DS, Green DW, Widmann RF. Long-term outcomes after posterior spine fusion for adolescent idiopathic scoliosis. Curr Opin Pediatr 2012;24:68–75.
Samdani AF, Ames RJ, Kimball JS, et al. Anterior vertebral body tethering for idiopathic scoliosis: two-year results. Spine (Phila Pa 1976) 2014;39:1688–93.
Samdani AF, Ames RJ, Kimball JS, et al. Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: one-year results on the first 32 patients. Eur Spine J 2015;24:1533–9.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: BSL (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; grants from Setting Scoliosis Straight Foundation, personal fees from DePuy Synthes Spine, personal fees from K2M, Paradigm Spine, Spine Search, and Ethicon; nonfinancial support from Spine Deformity Journal; grants from AO Spine, John and Marcella Fox Fund Grant, and the Orthopaedic Research and Education Foundation [OREF], outside the submitted work), YR (grants from Setting Scoliosis Straight Foundation, during the conduct of the study), SB (grants from Setting Scoliosis Straight Foundation, grants from International Spine Study Group Foundation, during the conduct of the study; grants from DePuy Synthes spine, grants from k2 medical, grants from NuVasive, grants from Innovasis, grants from Stryker spine, grants from Medtronic, outside the submitted work; in addition, SB has a patent NuVasive pending, a patent Innovasis pending, and a patent k2 medical with royalties paid), MK (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; grants from Cervical Spine Research Society [CSRS], OREF, Cerapedics, AOSpine, Barnes Jewish Foundation, Fox Family Foundation, and Patient-Centered Outcomes Research Institute, outside the submitted work), HJK (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; personal fees from K2M, Zimmer-Biomet, grants from International Spine Study Group [ISSGF], grants and personal fees from AO Spine, outside the submitted work; in addition, HJK has a patent null pending), BY (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; grants and personal fees from K2M and DePuy Synthes Spine; personal fees from NuVasive, Medtronic, Orthopediatrics, Stryker, and Globus; grants from Setting Scoliosis Straight Foundation, outside the submitted work; in addition, BY has a patent with K2M with royalties paid), VL (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; grants from DePuy Spine, NuVasive, K2M, Stryker; personal fees from NuVasive, DePuy Spine, Medicrea, MSD, and K2M; other from Nemaris INC, outside the submitted work), MM (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; personal fees from Setting Scoliosis Straight, outside the submitted work), FM (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; other from DePuy Synthes Canada, outside the submitted work), CIS (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; grants from ISSG, personal fees from Medtronic, NuVasive, Zimmer-Biomet, K2M, and Stryker; grants from National Institutes of Health [NIH], AOSpine North America [AO], and Department of Defense, outside the submitted work; in addition, CIS has a patent Medtronic with royalties paid, a patent NuVasive with royalties paid, and a patent Zimmer-Biomet with royalties paid), PON (grants from Setting Scoliosis Straight Foundation, during the conduct of the study; grants and other from Setting Scoliosis Straight Foundation; other from Rady Children’s Specialists; grants and personal fees from DePuy Synthes Spine; personal fees from Law firm of Carroll, Kelly, Trotter, Franzen & McKenna; personal fees from Law firm of Smith, Haughey, Rice & Roegge; grants from NIH and OREF; grants and other from Scoliosis Research Society [SRS]; grants from EOS Imaging; personal fees from Thieme Publishing; other from NuVasive; personal fees from Ethicon Endosurgery; other from Electrocore; personal fees from Cubist; other from International Orthopedic Think Tank and from Orthopediatrics Institutional Support; personal fees from K2M, outside the submitted work; in addition, PON has a patent “Anchoring Systems and Methods for Correcting Spinal Deformities” [8540754] with royalties paid to DePuy Synthes Spine ent “Screw Placement Guide” [7981117] issued to DePuy Spine, Inc.; and a patent “Compressor for Use in Minimally Invasive Surgery” [7189244] issued to DePuy Spine, Inc).
Funding: Research grant funding was received by Setting Scoliosis Straight Foundation to support Harms Study Group’s research.
No Funding support was received for any aspect of the submitted work by the International Spine Study Group. Grants from DePuy were received by the International Spine Study Group for data collection.
IRB Approval: Institutional review board approval was obtained for this study from all participating sites.
Rights and permissions
About this article
Cite this article
Lonner, B.S., Ren, Y., Bess, S. et al. Surgery for the Adolescent Idiopathic Scoliosis Patients After Skeletal Maturity: Early Versus Late Surgery. Spine Deform 7, 84–92 (2019). https://doi.org/10.1016/j.jspd.2018.05.012
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.05.012