Abstract
Study Design
Retrospective single-center.
Objectives
To investigate changes in pelvic incidence from flexion to extension. To assess interobserver error in the measurement of pelvic incidence.
Background
Pelvic incidence (PI) has been considered a static parameter since it was originally described. But recent studies have shown that PI can change with age and after spinal procedures. Changes in PI based on position have not been investigated.
Methods
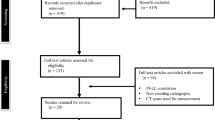
Seventy-two patients who had obtained flexion and extension radiographs of the lumbar spine were identified using strict inclusion and exclusion criteria. PI along with pelvic tilt (PT), sacral slope (SS), and lumbar lordosis were measured in both flexion and extension by two independent measurers. Variations in all parameters and interobserver measurement reliability were analyzed for the entire group.
Results
PI changed significantly from flexion to extension with a general tendency to decrease: mean (–0.94°), p <.044. However, these changes might have had opposite vectors, and exceeded | 6°| (measurement error) in 20% of cases, with a maximum of 12°. Inconsistencies in changes of SS, as opposed to PT from flexion to extension, were found to be the major factor determining changes in PI (p >.001). Obesity significantly contributed to differences in PI between flexion and extension (p = .003).
Conclusions
PI is a dynamic parameter that changes between flexion and extension. Changes in SS are the main factor involved in these changes, implicating movement through the sacroiliac joints as the cause. Obese patients have greater changes in PI from flexion to extension.
Level of Evidence
Level II.
Similar content being viewed by others
References
Legaye J, Duval-Beaupere G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 1998;7:99–103.
Le Huec JC, Aunoble S, Philippe L, Nicolas P. Pelvic parameters: origin and significance. Eur Spine J 2011;20(suppl 5):564–71.
Peleg S, Dar G, Steinberg N, et al. Sacral orientation revisited. Spine (Phila Pa 1976) 2007;32:E397–404.
Peleg S, Dar G, Medlej B, et al. Orientation of the human sacrum: anthropological perspectives and methodological approaches. Am J Phys Anthropol 2007;133:967–77.
Iyer S, Lenke LG, Nemani VM, et al. Variations in sagittal alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine (Phila Pa 1976) 2016;41:1826–36.
Inami S, Moridaira H, Takeuchi D, et al. Optimum pelvic incidence minus lumbar lordosis value can be determined by individual pelvic incidence. Eur Spine J 2016;25:3638–43.
Lee JH, Na KH, Kim JK, et al. Is pelvic incidence a constant, as everyone knows? Changes of pelvic incidence in surgically corrected adult sagittal deformity. Eur Spine J 2016;25:3707–14.
Noshchenko A, Hoffecker L, Cain CM, et al. Spinopelvic parameters in asymptomatic subjects without spine disease and deformity: a systematic review with meta-analysis. Clin Spine Surg 2017;30:392–403.
Schwab F, Patel A, Ungar B, et al. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35:2224–31.
Vleeming A, Schuenke MD, Masi AT, et al. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat 2012;221:537–67.
Adhia DB, Milosavjevic S, Tumilty S, et al. Innominate movement patterns, rotation trends and range of motion in individuals with low back pain of sacroiliac joint origin. Man Ther 2016;21:100–8.
Kibsgard TJ, Roise O, Sturesson B, et al. Radiosteriometric analysis of movement in the sacroiliac joint during a single-leg stance in patients with long-lasting pelvic girdle pain. Clin Biomech (Bristol, Avon) 2014;29:406–11.
Wang M, Dumas GA. Mechanical behavior of the female sacroiliac joint and influence of the anterior and posterior sacroiliac ligaments under sagittal loads. Clin Biomech (Bristol, Avon) 1998;13:293–9.
Carman DL, Browne RH, Birch JG Measurement of scoliosis and kyphosis radiographs. Intraobserver and interobserver variation. J Bone Joint Surg Am 1990;72:328–33.
Chen RQ, Hosogane N, Watanabe K, et al. Reliability analysis of spino-pelvic parameters in adult spinal deformity: a comparison of whole spine and pelvic radiographs. Spine (Phila Pa 1976) 2016;41:320–7.
Kuklo TR, Potter BK, Polly DW, et al. Reliability analysis for manual adolescent idiopathic scoliosis measurements. Spine (Phila Pa 1976) 2005;30:444–54.
Buckland AJ, Viqdorchik J, Schwab FJ, et al. Acetabular anteversion changes due to spinal deformity correction: bridging the gap between hip and spine surgeons. J Bone Joint Surg Am 2015;97:1913–20.
Ochi H, Baba T, Homma Y, et al. Importance of the spinopelvic factors on the pelvic inclination from standing to sitting before total hip arthroplasty. Eur Spine J 2016;25:3699–706.
DeMann Jr LE. Sacroiliac dysfunction in dancers with low back pain. Man Ther 1997;2:2–10.
Glantz SA. Primer of biostatistics. 6th ed. New York: McGraw-Hill Medical;2005. p. 520.
Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics 1989;45:255–68.
Tyrakowski M, Wojtera-Tyrakowska D, Siemionow K. Influence of pelvic rotation on pelvic incidence, pelvic tilt, and sacral slope. Spine (Phila Pa 1976) 2014;39:E1276–83.
Goetzen M, Kl Ortner, Lindtner RA, et al. A simple approach for the preoperative assessment of sacral morphology for percutaneous SI screw fixation. Arch Orthop Trauma Surg 2016;136:1251–7.
Mahato NK. Variable positions of the sacral auricular surface: classification and importance. Neurosurg Focus 2010;28:E12.
Aurouer N, Obeid I, Pointillart V, et al. Computerized preoperative planning for correction of sagittal deformity of the spine. Surg Radiol Anat 2009;31:781–92.
Sun XY, Zhang XN, Hai Y. Optimum pelvic incidence minus lumbar lordosis value after operation for patients with adult degenerative scoliosis. Spine J 2017;17:983–9.
Than KD, Park P, Fu KM, et al. Clinical and radiographic parameters associated with best versus worst clinical outcomes in minimally invasive spinal deformity surgery. J Neurosurg Spine 2016;25:21–5.
Xu L, Qin X, Zhang W, et al. Estimation of the ideal lumbar lordosis to be restored from spinal fusion surgery: a predictive formula for Chinese population. Spine (Phila Pa 1976) 2015;40:1001–5.
Yamato Y, Hasegawa T, Kobayashi S, et al. Calculation of the target lumbar lordosis angle for restoring an optimal pelvic tilt in elderly patients with adult spinal deformity. Spine (Phila Pa 1976) 2016;41:E211–7.
Yagi M, Kaneko S, Yato Y, et al. Walking sagittal balance correction by pedicle subtraction osteotomy in adults with fixed sagittal imbalance. Eur Spine J 2016;25:2488–96.
Yagi M, Ohne H, Konomi T, et al. Walking balance and compensatory gait mechanisms in surgically treated patients with adult spinal deformity. Spine J 2017;17:409–17.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: NS (none), AN (none), EB (grants from OMeGA, Globus, Aesculap, SI Bone, VertiFlex, Medicrea, Medtronic, Orthofix, Integra LifeSciences Corporation, Pfizer, Spinal Kinetics, Synthes, Anschutz Foundation, and from Mainstay, outside the submitted work), VP (grants and personal fees from Aesculap and Medtronic; grants from Stryker, SI Bone, Musculoskeletal Transplant Foundation, and National Institutes of Health; personal fees from Biomet, Baxter; grants from Synthes, Orthofix, Orthopaedic Research and Education Foundation [OREF], and Anschutz Foundation, outside the submitted work), CC (grants from Medtronic Sofamor-Danek, Aesculap, SI Bone, VertiFlex, Medicrea, Orthofix, Integra Life Sciences Corporation, Pfizer, Spinal Kinetics, DePuy Synthes, Musculoskeletal Transplant Foundation, National Institutes of Health, and Medacta; personal fees from DePuy Synthes, DePuy Synthes, Globus Medical, and NuVasive, outside the submitted work), DOY (grants from Medtronic Sofamor-Danek, Aesculap, SI Bone, VertiFlex, Medicrea, Orthofix, Integra Life Sciences Corporation, Pfizer, Spinal Kinetics, DePuy Synthes, Musculoskeletal Transplant Foundation, National Institutes of Health, and Medacta, outside the submitted work), CK (grants from Medtronic Sofamor-Danek, Aesculap, SI Bone, VertiFlex, Medicrea, Orthofix, Integra Life Sciences Corporation, Pfizer, Spinal Kinetics, DePuy Synthes, Musculoskeletal Transplant Foundation, and National Institutes of Health; other from Medacta; grants from Fellowship Funding, outside the submitted work).
Institutional review board approval was obtained from the Colorado Multiple Institutional Review Board, protocol number 16-2150.
Rights and permissions
About this article
Cite this article
Schroeder, N., Noschenko, A., Burger, E. et al. Pelvic Incidence Changes Between Flexion and Extension. Spine Deform 6, 753–761 (2018). https://doi.org/10.1016/j.jspd.2018.03.008
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.03.008