Abstract
Background
Transcranial motor evoked potential (TcMEP) is widely used intraoperatively to monitor spinal cord and nerve root function. To our knowledge, there is no report regarding TcMEP signal loss purely caused by patient positioning during the spinal procedure.
Purpose
The objective of this article is to report an intraoperative TcMEP signal loss of a patient with fixed sagittal imbalance posture along with mild hip contractures.
Study Design
A retrospective case report.
Methods
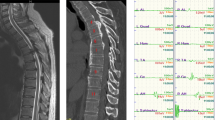
A 57-year-old man had fixed sagittal imbalance and flexed hip contractures. For a reconstruction surgery of T10 to the sacrum/ilium and L5 pedicle subtraction osteotomy (PSO), he was put in a prone position on a Jackson table. In order to accommodate his fixed hip flexion contracture, thigh pads were not used and pillows were placed under his bilateral thighs for cushioning. TcMEPs were used to assess lumbar nerve root function. Ten minutes after incision, bilateral vastus medialis TcMEPs were lost during spine exposure whereas all other data remained normal at baseline. The bilateral lower extremities were repositioned, with the knees flexed into a sling position to increase hip flexion. Five minutes after repositioning, the bilateral vastus medialis TcMEPs gradually improved and maintained baseline amplitude during the remainder of the surgery.
Results
No muscle weakness was detected immediately after surgery. The patient was discharged day 6 postoperatively with markedly improved posture and alignment.
Conclusion
Insufficient hip flexion in patients with fixed sagittal imbalance and hip flexion contractures may cause TcMEP signal changes in the quadriceps response. TcMEP monitoring of bilateral lower extremities is highly recommended for patients with sagittal imbalance and hip contractures, with consideration for lower extremity repositioning when data degradation does not correlate with the actual spinal procedure being performed.
Similar content being viewed by others
References
Duke K, Aubin CE, Dansereau J, Labelle H. Biomechanical simulations of scoliotic spine correction due to prone position and anaesthesia prior to surgical instrumentation. Clin Biomech (Bristol, Avon) 2005;20:923–31.
Harimaya K, Lenke LG, Mishiro T, et al. Increasing lumbar lordosis of adult spinal deformity patients via intraoperative prone positioning. Spine (Phila Pa 1976) 2009;34:2406–12.
Hazarika A, Rath GP. Modified prone positioning for dorsal spine surgery in a patient with postural deformity due to spasticity of lower limbs. J Clin Anesth 2014;26:582–4.
Sutter MA, Eggspuehler A, Grob D, et al. Multimodal intraoperative monitoring (MIOM) during 409 lumbosacral surgical procedures in 409 patients. Eur Spine J 2007;16(suppl 2):S221–8.
Lieberman JA, Lyon R, Feiner J, et al. The efficacy of motor evoked potentials in fixed sagittal imbalance deformity correction surgery. Spine 2008;33:E414–24.
Duke K, Aubin CE, Dansereau J, Labelle H. Computer simulation for the optimization of patient positioning in spinal deformity instrumentation surgery. Med Biol Eng Comput 2008;46:33–41.
Bjerke BT, Zuchelli DM, Nemani VM, et al. Prognosis of significant intraoperative neurophysiologic monitoring events in severe spinal deformity surgery. Spinal Deform 2017;5:117–23.
Eager M, Jahangiri F, Shimer A, et al. Intraoperative neuromonitoring: lessons learned from 32 case events in 2095 spine cases. Evid Based Spine Care J 2010;1:58–61.
Thirumala PD, Crammond DJ, Loke YK, et al. Diagnostic accuracy of motor evoked potentials to detect neurological deficit during idiopathic scoliosis correction: a systematic review. J Neurosurg Pediatr 2016;30:1–10.
Plata Bello J, Pérez-Lorensu PJ, Roldân-Delgado H, et al. Role of multimodal intraoperative neurophysiological monitoring during positioning of patient prior to cervical spine surgery. Spine (Phila Pa 1976) 2014;39:E989–93.
Tanaka S, Tashiro T, Gomi A, et al. Sensitivity and specificity in transcranial motor-evoked potential monitoring during neurosurgical operations. Surg Neuro Int 2011;2:111.
Mok JM, Lyon R, Lieberman JA, et al. Monitoring of nerve root injury using transcranial motor—evoked potentials in a pig model. Spine (Phila Pa 1976) 2008;33:E465–73.
Lyon R, Lieberman JA, Feiner J, Burch S. Relative efficacy of transcranial motor evoked potentials, mechanically-elicited electromyography, and evoked EMG to assess nerve root function during sustained retraction in a porcine model. Spine (Phila Pa 1976) 2009;34:E558–64.
Valone 3rd F, Lyon R, Lieberman J, Burch S. Efficacy of transcranial motor evoked potentials, mechanically elicited electromyography, and evoked electromyography to assess nerve root function during sustained compression in a porcine model. Spine (Phila Pa 1976) 2014;39:E989–93.
Epstein NE, Stecker MM. Intraoperative neuro-monitoring corner editorial: the need for preoperative SEP and MEP baselines in spinal surgery: why can’t we and our monitoring colleagues get this right? Surg Neurol Int 2014;5(Suppl 15):S548–51.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: XJL (none), LGL (other from Orthopaedic Research and Education Foundation [OREF] and Global Spine Outreach [GSO], other from Medtronic, DePuy-Synthes, K2M, grants from AOSpine, Setting Scoliosis Straight Foundation, EOS Imaging, Fox Family Foundation, Scoliosis Research Society, other from Medtronic, Quality Medical Publishing, other from BroadWater, AO Spine, other from Medtronic, outside the submitted work), ET (none), LAT (none), AT (none).
Rights and permissions
About this article
Cite this article
Li, X.J., Lenke, L.G., Thuet, E. et al. Prone Position—Induced Quadriceps Transcranial Motor Evoked Potentials Signal Loss—A Case Report. Spine Deform 6, 627–630 (2018). https://doi.org/10.1016/j.jspd.2018.02.008
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.02.008