Abstract
Study Design
Cadaveric feasibility study and case report.
Objective
To determine if it is feasible to rotate pedicled vascularized bone graft (VBG) from L1 to S1 via a posterior approach.
Summary of Background Data
VBG has been used to successfully augment fusion rates in various skeletal pathologies. Pedicled VBG has numerous advantages over free-transfer VBG, including the maintenance of a robust vascular supply to the graft without the need for vascular anastomoses. Pedicled VBG options have not been well described for posterior lumbosacral fusion.
Methods
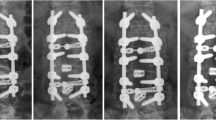
A multidisciplinary team of plastic surgeons and neurosurgeons hypothesized that it is feasible to rotate pedicled VBG from L1 to S1 via a posterior approach. In six cadavers, two VBG donor sites were evaluated: posterior element (PE-VBG) and iliac crest (IC-VBG). A single case report of a patient with lumbar Charcot joint treated with IC-VBG is also presented.
Results
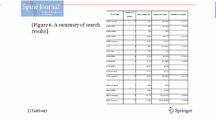
For the PE-VBG, the laminae and spinous processes were mobilized en bloc via Gill laminectomy on a unilateral sacrospinalis pedicle. Mean ± standard deviation (SD) length × width graft dimensions were 2.8±0.48 cm × 2.2±0.81 cm. The inter–transverse process (inter-TP) distance was less than the corresponding lamina length at all levels. For the IC-VBG, iliac crest was mobilized on a quadratus lumborum pedicle. Mean±SD length × width × thickness graft dimensions were 7.7±1.28 cm × 2.2±0.69 cm × 1.5±0.79 cm. The IC-VBGs reached from L1 (T12–S1) to S1 (S1–S3), and all IC-VBGs were able to cover three levels.
Conclusions
This feasibility cadaveric study and the case report are the first demonstrations that pedicled VBGs can be successfully applied to posterior lumbosacral spinal arthrodesis. Patients at high risk for nonunion may benefit from these strategies. Further clinical experience with these techniques is warranted.
Level of Evidence
Level IV.
Similar content being viewed by others
References
Berjano P, Langella F, Damilano M, et al. Fusion rate following extreme lateral lumbar interbody fusion. Eur Spine J 2015;24(suppl 3):369–71.
DePalma AF, Rothman RH. The nature of pseudarthrosis. Clin Orthop Relat Res 1968;59:113–8.
Grubb SA, Lipscomb HJ, Suh PB. Results of surgical treatment of painful adult scoliosis. Spine (Phila Pa 1976) 1994;19:1619–27.
Herkowitz HN, Sidhu KS. Lumbar spine fusion in the treatment of degenerative conditions: current indications and recommendations. J Am Acad Orthop Surg 1995;3:123–35.
Bradford DS, Ganjavian S, Antonious D, et al. Anterior strut-grafting for the treatment of kyphosis. Review of experience with forty-eight patients. J Bone Joint Surg Am 1982;64:680–90.
Bradford DS, Daher YH. Vascularised rib grafts for stabilisation of kyphosis. J Bone Joint Surg Br 1986;68:357–61.
Jenkins DH, Cheng DH, Hodgson AR. Stimulation of bone growth by periosteal stripping: a clinical study. J Bone Joint Surg Br 1975;57: 482–4.
Rajasekaran S, Soundarapandian S. Progression of kyphosis in tuberculosis of the spine treated by anterior arthrodesis. J Bone Joint Surg Am 1989;71:1314–23.
Han CS, Wood MB, Bishop AT, et al. Vascularized bone transfer. J Bone Joint Surg Am 1992;74:1441–9.
Noorda RJ, Wuisman PI, Fidler MW, et al. Severe progressive osteoporotic spine deformity with cardiopulmonary impairment in a young patient: a case report. Spine (Phila Pa 1976) 1999;24:489–92.
Weiland AJ, Moore JR, Daniel RK. Vascularized bone autografts: experience with 41 cases. Clin Orthop Relat Res 1983:87–95.
Winters HA, van Harten SM, van Royen BJ. The iliolumbar artery as the nutrient pedicle for an iliac crest graft: a new technique in reconstruction of the lumbar spine. Plast Reconstr Surg 2002;109:249–52.
Lonstein JE, Winter RB. Long multiple struts for severe kyphosis. Clin Orthop Relat Res 2002:130–8.
Shin AY, Bishop AT. Vascularized bone grafts for scaphoid nonunions and Kienböck’s disease. Orthop Clin North Am 2001;32:263–77. viii.
Arata MA, Wood MB. Cooney 3rd WP Revascularized segmental diaphyseal bone transfers in the canine: an analysis of viability. J Reconstr Microsurg 1984;1:11–9.
Cutting CB, McCarthy JG. Comparison of residual osseous mass between vascularized and nonvascularized onlay bone transfers. Plast Reconstr Surg 1983;72:672–5.
Aydinli U, Akin S, Tirelioglu O, et al. A new autogenous graft choice in pelvic reconstructions: free vascularized rib (a case report). Arch Orthop Trauma Surg 2006;126:57–62.
Kim CW, Abrams R, Lee G, et al. Use of vascularized fibular grafts as a salvage procedure for previously failed spinal arthrodesis. Spine (Phila Pa 1976) 2001;26:2171–5.
Meyers AM, Noonan KJ, Mih AD, et al. Salvage reconstruction with vascularized fibular strut graft fusion using posterior approach in the treatment of severe spondylolisthesis. Spine (Phila Pa 1976) 2001;26: 1820–4.
Chen ZC, Fan KF, Wu WC, et al. Fusion of the lumbar spine with a free vascularized fibular bone graft: case report. Changgeng Yi Xue Za Zhi 1998;21:463–8.
Hubbard LF, Herndon JH, Buonanno AR. Free vascularized fibula transfer for stabilization of the thoracolumbar spine. A case report. Spine (Phila Pa 1976) 1985;10:891–3.
Ackerman DB, Rose PS, Moran SL, et al. The results of vascularized-free fibular grafts in complex spinal reconstruction. J Spinal Disord Tech 2011;24:170–6.
Aliano KA, Agulnick M, Cohen B, et al. Spinal reconstruction for osteomyelitis with free vascularized fibular grafts using intraabdominal recipient vessels: a series of three cases. Microsurgery 2013;33:560–6.
Lu DC, Wang V, Chou D. The use of allograft or autograft and expandable titanium cages for the treatment of vertebral osteomyelitis. Neurosurgery 2009;64:122–9; discussion 129–30.
Yelizarov VG, Minachenko VK, Gerasimov OR, et al. Vascularized bone flaps for thoracolumbar spinal fusion. Ann Plast Surg 1993;31:532–8.
Lewis SJ, Kulkarni AG, Rampersaud YR, et al. Posterior column reconstruction with autologous rib graft after en bloc tumor excision. Spine (Phila Pa 1976) 2012;37:346–50.
Wilden JA, Moran SL, Dekutoski MB, et al. Results of vascularized rib grafts in complex spinal reconstruction. J Bone Joint Surg Am 2006;88:832–9.
Robertson PA, Wray AC. Natural history of posterior iliac crest bone graft donation for spinal surgery: a prospective analysis of morbidity. Spine (Phila Pa 1976) 2001;26:1473–6.
Ahlmann E, Patzakis M, Roidis N, et al. Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. J Bone Joint Surg Am 2002;84:716–20.
Nocini PF, Bedogni A, Valsecchi S, et al. Fractures of the iliac crest following anterior and posterior bone graft harvesting: review of the literature and case presentation. Minerva Stomatol 2003;52:441–8. 448–452.
Quinones-Hinojosa A, Jun P, Jacobs R, et al. General principles in the medical and surgical management of spinal infections: a multidisciplinary approach. Neurosurg Focus 2004;17:E1.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: MAB (none), MAM (none), JSC (none), KKA (none), JDT (none), SWC (none), MCP (none), EMR (none), UKK (none).
This study was funded by grants from the Barrow Neurological Foundation and the Newsome Family Endowed Chair of Neurosurgery.
The authors thank the Neuroscience Publications staff at Barrow Neurological Institute for assistance with illustrations and manuscript preparation.
Rights and permissions
About this article
Cite this article
Bohl, M.A., Mooney, M.A., Catapano, J.S. et al. Pedicled Vascularized Bone Grafts for Posterior Lumbosacral Fusion: A Cadaveric Feasibility Study and Case Report. Spine Deform 6, 498–506 (2018). https://doi.org/10.1016/j.jspd.2018.02.006
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.02.006