Abstract
Study Design
Retrospective case-control matched cohort from a single institution.
Objective
To examine the contribution of nonmechanical factors to the incidence of proximal junctional failure (PJF) after adult spinal deformity (ASD) surgery.
Summary of Background Data
Multiple studies have reported on the prevalence of PJF following surgery for ASD. However, little is known about the contribution of nonmechanical factors to the incidence of PJF.
Methods
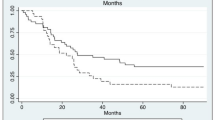
We identified a consecutive series of ASD patients who required revision surgery for PJF between 2013 and 2015. A matched cohort of ASD patients who did not develop PJF after surgical correction was identified based on age, gender, preoperative deformity type, number of fusion levels, and the lower instrumented vertebra level. We compared medical and surgical histories in the matched cohorts, with particular attention to the prevalence of preoperative neurologic comorbidities that might affect standing balance. Preoperative, immediate postoperative, and follow-up radiographs were reviewed to document specific characteristics of mechanical failure that resulted in PJF and required revision surgery.
Results
Twenty-eight cases of PJF requiring revision surgery were identified. The prevalence rates of preoperative neurologic comorbidities in PJF cohort were significantly higher than in non-PJF cohort (75% vs. 32%, p < .001). Neurologic comorbidities included prior stroke (4), metabolic encephalopathy (2), Parkinson disease (1), seizure disorder (1), cervical and thoracic myelopathy (7), diabetic neuropathy (4), and other neuropathy (4). The mean preoperative sagittal vertical axis in PJF cohort was more positive compared with the non-PJF cohort (144 mm vs. 65 mm, p = .009) There were no significant differences in immediate postoperative or follow-up radiographic parameters between cohorts.
Conclusions
In this study, risk factors identified for the development of PJF included nonmechanical neurologic comorbidities, emphasizing the need to look beyond radiographic alignment in order to reduce the incidence of PJF.
Level of Evidence
Level 3.
Similar content being viewed by others
References
Schwab F, el-Fegoun AB, Gamez L, et al. A lumbar classification of scoliosis in the adult patient: preliminary approach. Spine (Phila Pa 1976) 2005;30:1670–3.
Arlet V, Aebi M. Junctional spinal disorders in operated adult spinal deformities: present understanding and future perspectives. Eur Spine J 2013;22(Suppl 2):S276–95.
Rose PS, Bridwell KH, Lenke LG, et al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976) 2009;34:785–91.
Smith JS, Bess S, Shaffrey CI, et al. Dynamic changes of the pelvis and spine are key to predicting postoperative sagittal alignment after pedicle subtraction osteotomy: a critical analysis of preoperative planning techniques. Spine (Phila Pa 1976) 2012;37: 845–53.
Le Huec JC, Leijssen P, Duarte M, et al. Thoracolumbar imbalance analysis for osteotomy planification using a new method: FBI technique. Eur Spine J 2011;20(Suppl 5):669–80.
Glassman SD, Hamill CL, Bridwell KH, et al. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 2007;32:2764–70.
Crawford 3rd CH, Carreon LY, Bridwell KH, et al. Long fusions to the sacrum in elderly patients with spinal deformity. Eur Spine J 2012;21:2165–9.
Bhagat S, Vozar V, Lutchman L, et al. Morbidity and mortality in adult spinal deformity surgery: Norwich Spinal Unit experience. Eur Spine J 2013;22(Suppl l):S42–6.
Weistroffer JK, Perra JH, Lonstein JE, et al. Complications in long fusions to the sacrum for adult scoliosis: minimum five-year analysis of fifty patients. Spine (Phila Pa 1976) 2008;33:1478–83.
Charosky S, Guigui P, Blamoutier A, et al. Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients. Spine (Phila Pa 1976) 2012;37:693–700.
Scheer JK, Tang JA, Smith JS, et al. Reoperation rates and impact on outcome in a large, prospective, multicenter, adult spinal deformity database: clinical article. J Neurosurg Spine 2013;19:464–70.
Cho SK, Bridwell KH, Lenke LG, et al. Major complications in revision adult deformity surgery: risk factors and clinical outcomes with 2- to 7-year follow-up. Spine (Phila Pa 1976) 2012;37: 489–500.
Glattes RC, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 2005;30:1643–9.
Kim YJ, Bridwell KH, Lenke LG, et al. Sagittal thoracic decompensation following long adult lumbar spinal instrumentation and fusion to L5 or S1: causes, prevalence, and risk factor analysis. Spine (Phila Pa 1976) 2006;31:2359–66.
Hostin R, McCarthy I, O’Brien M, et al. Incidence, mode, and location of acute proximal junctional failures after surgical treatment of adult spinal deformity. Spine (Phila Pa 1976) 2013;38: 1008–15.
Hart RA, McCarthy I, Ames CP, et al. Proximal junctional kyphosis and proximal junctional failure. Neurosurg Clin N Am 2013;24: 213–8.
Hart R, McCarthy I, O’Brien M, et al. Identification of decision criteria for revision surgery among patients with proximal junctional failure after surgical treatment of spinal deformity. Spine (Phila Pa 1976) 2013;38:E1223–7.
Kim YJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 2008;33:2179–84.
Kim HJ, Lenke LG, Shaffrey CI, et al. Proximal junctional kyphosis as a distinct form of adjacent segment pathology after spinal deformity surgery: a systematic review. Spine (Phila Pa 1976) 2012;37: S144–64.
Mendoza-Lattes S, Ries Z, Gao Y, et al. Proximal junctional kyphosis in adult reconstructive spine surgery results from incomplete restoration of the lumbar lordosis relative to the magnitude of the thoracic kyphosis. Iowa Orthop J 2011;31:199–206.
Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976) 2012;37:1479–89.
Maruo K, Ha Y, Inoue S, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 2013;38:E1469–76.
Kim HJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis results in inferior SRS pain subscores in adult deformity patients. Spine (Phila Pa 1976) 2013;38:896–901.
Lau D, Clark AJ, Scheer JK, et al. Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976) 2014;39:2093–102.
Glassman SD, Dimar 2nd JR, Carreon LY. Revision rate after adult deformity surgery. Spine Deform 2015;3:199–203.
Daubs MD, Lenke LG, Cheh G, et al. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976) 2007;32:2238–44.
Inoue S, Khashan M, Fujimori T, et al. Analysis of mechanical failure associated with reoperation in spinal fusion to the sacrum in adult spinal deformity. J Orthop Sci 2015;20:609–16.
Glassman SD, Coseo MP, Carreon LY. Sagittal balance is more than just alignment: why PJK remains an unresolved problem. Scoliosis Spinal Disord 2016;11:1.
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83.
O’Brien M, Kuklo T, Blanke K, et al. Spinal deformity study group radiographic measurement manual. Memphis, TN: Medtronic Sofamor Danek USA, Inc.; 2005.
Ames CP, Smith JS, Scheer JK, et al. Impact of spinopelvic alignment on decision making in deformity surgery in adults: a review. J Neurosurg Spine 2012;16:547–64.
Yoshida G, Yasuda T, Togawa D, et al. Craniopelvic alignment in elderly asymptomatic individuals: analysis of 671 cranial centers of gravity. Spine (Phila Pa 1976) 2014;39:1121–7.
Banno T, Togawa D, Arima H, et al. The cohort study for the determination of reference values for spinopelvic parameters (T1 pelvic angle and global tilt) in elderly volunteers. Eur Spine J 2016;25: 3687–93.
Arima H, Yamato Y, Hasegawa T, et al. Discrepancy between standing posture and sagittal balance during walking in adult spinal deformity patients. Spine (Phila Pa 1976) 2017;42: E25–30.
Fairbank JC, Couper J, Davies JB, et al. The Oswestry low back pain disability questionnaire. Physiotherapy 1980;66:271–3.
EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199–208.
Lee GA, Betz RR, Clements 3rd DH, et al. Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine (Phila Pa 1976) 1999;24:795–9.
Kim HJ, Bridwell KH, Lenke LG, et al. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976) 2014;39:E576–80.
Bridwell KH, Lenke LG, Cho SK, et al. Proximal junctional kyphosis in primary adult deformity surgery: evaluation of 20 degrees as a critical angle. Neurosurgery 2013;72:899–906.
O’Leary PT, Bridwell KH, Lenke LG, et al. Risk factors and outcomes for catastrophic failures at the top of long pedicle screw constructs: a matched cohort analysis performed at a single center. Spine (Phila Pa 1976) 2009;34:2134–9.
Wang J, Zhao Y, Shen B, et al. Risk factor analysis of proximal junctional kyphosis after posterior fusion in patients with idiopathic scoliosis. Injury 2010;41:415–20.
Cammarata M, Aubin CE, Wang X, et al. Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine (Phila Pa 1976) 2014;39: E500–7.
Kebaish KM, Martin CT, O’Brien JR, et al. Use of vertebroplasty to prevent proximal junctional fractures in adult deformity surgery: a biomechanical cadaveric study. Spine J 2013;13:1897–903.
Hart RA, Prendergast MA, Roberts WG, et al. Proximal junctional acute collapse cranial to multi-level lumbar fusion: a cost analysis of prophylactic vertebral augmentation. Spine J 2008;8: 875–81.
Hassanzadeh H, Gupta H, Jain A, et al. Significant effect on the incidence of proximal junctional kyphosis and outcome in adults after long posterior spinal fusion. Spine Deform 2013;1: 299–305.
Bourghli A, Guerin P, Vital JM, et al. Posterior spinal fusion from T2 to the sacrum for the management of major deformities in patients with Parkinson disease: a retrospective review with analysis of complications. J Spinal Disord Tech 2012;25:E53–60.
Babat LB, McLain RF, Bingaman W, et al. Spinal surgery in patients with Parkinson’s disease: construct failure and progressive deformity. Spine (Phila Pa 1976) 2004;29:2006–12.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: HA (personal fees from Norton Healthcare, outside the submitted work), SDG (employee of Norton Healthcare, grants to institution from Norton Healthcare, patents and royalties from Medtronic), JRD (consultancy fees from Medtronic and DePuy; personal fees from Medtronic, DePuy, and Norton Healthcare; patents from Medtronic, royalties, and other from JBJS Highlights, Spine, Spine Deformity, JAAOS and Global Spine; is a member of the SRS Board), YM (none), LYC (other from Spine, other from Spine Journal, other from University of Louisville, other from Scoliosis Research Society, personal fees from Washington University, personal fees from AO Spine, personal fees from Norton Healthcare, grants from Orthopedic Research and Educational Fund, grants from Scoliosis Research Society, grants from the Norton Healthcare James R. Petersdorf Fund, personal fees from University of Louisville, personal fees from Association for Collaborative Spine Research, personal fees from Center for Spine Surgery and Research, Region of Southern Denmark, other from NuVasive, outside the submitted work).
Rights and permissions
About this article
Cite this article
Arima, H., Glassman, S.D., Dimar, J.R. et al. Neurologic Comorbidities Predict Proximal Junctional Failure in Adult Spinal Deformity. Spine Deform 6, 576–586 (2018). https://doi.org/10.1016/j.jspd.2018.01.008
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2018.01.008