Abstract
Study Design
Retrospective review of a prospectively collected database.
Objective
To assess the incidence of deep vein thrombosis (DVT) associated with single- versus multistage posterior-only complex spinal surgeries.
Summary of Background Data
Dividing the physiologic burden of spinal deformity surgery into multiple stages has been suggested as a potential means of reducing perioperative complications. DVT is a worrisome complication owing to its potential to lead to pulmonary embolism. Whether or not staging affects DVT incidence in this population is unknown.
Methods
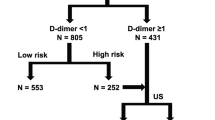
Consecutive patients undergoing either single- or multistage posterior complex spinal surgeries over a 12-year period at a single institution were eligible. All patients received lower extremity venous duplex ultrasonographic (US) examinations 2 to 4 days postoperatively in the single-stage group and 2 to 4 days postoperatively after each stage in the multistage group. Multivariate logistic regression was used to assess the independent contribution of staging to developing a DVT.
Results
A total of 107 consecutive patients were enrolled—26 underwent multistage surgery and 81 underwent single-stage surgery. The single-stage group was older (63 years vs. 45 years; p < .01) and had a higher Charlson comorbidity index (2.25 ± 1.27 vs. 1.23 ± 1.58; p < .01). More multistage patients had positive US tests than single-stage patients (5 of 26 vs. 6 of 81; 19% vs. 7%;p = .13). Adjusting for all the above-mentioned covariates, a multistage surgery was 8.17 (95% CI 0.35–250.6) times more likely to yield a DVT than a single-stage surgery.
Conclusions
Patients who undergo multistage posterior complex spine surgery are at a high risk for developing a DVT compared to those who undergo single-stage procedures. The difference in DVT incidence may be understated as the multistage group had a lower pre- and intraoperative risk profile with a younger age, lower medical comorbidities, and less per-stage blood loss.
Similar content being viewed by others
References
American Academy of Orthopaedic Surgeons. Deep vein thrombosis [OrthoInfo web site]. Available at: http://www5.aaos.org/dvt/main.cfm; 2015. Accessed June 16, 2016.
Sansone JM, del Rio AM, Anderson PA. The prevalence of and specific risk factors for venous thromboembolic disease following elective spine surgery. J Bone Joint Surg Am 2010;92:304–13.
Meyerding HW. Spondylolisthesis. Surg Gynecol Obstet 1932;54:371–7.
Shufflebarger HL, Grimm JO, Bui V, et al. Anterior and posterior spinal fusion: staged versus same-day surgery. Spine 1991;16:930–3.
Rhee JM, Bridwell KH, Lenke LG, et al. Staged posterior surgery for severe adult spinal deformity. Spine 2003;28:2116–21.
Mandelbaum BR, Tolo VT, McAfee PC, et al. Nutritional deficiencies after staged anterior and posterior spinal reconstructive surgery. Clin Orthop 1998;234:5–11.
Lapp MA, Bridwell KH, Lenke LG, et al. Prospective randomization of parenteral hyperalimentation for long fusions with spinal deformity: its effect on complications and recovery from postoperative malnutrition. Spine 2001;26:809–17.
Hu SS, Fontaine F, Kelly B, et al. Nutritional depletion in staged spinal reconstructive: the effect of total parenteral nutrition. Spine 1998;23:1401–5.
Ogilvie JW. Anterior and posterior spinal surgery: same day, staged, anterior first, posterior first, or simultaneous? Instr Course Lect 1996;45:99.
Yoshioka K, Murakami H, Demura S, et al. Prevalence and risk factors for development of venous thromboembolism after degenerative spinal surgery. Spine 2010;40:E301–6.
McClendon Jr J, O’shaughnessy BA, Smith TR, et al. Comprehensive assessment of prophylactic preoperative inferior vena cava filters for major spinal reconstruction in adults. Spine 2012;37:1122–9.
Uden A. Thromboembolic complications following scoliosis surgery in Scandinavia. Acta Orthop Scand 1979;50:175–8.
Hohl JB, Lee JY, Rayappa SP, et al. Prevalence of venous thromboembolic events after elective major thoracolumbar degenerative spine surgery. J Spinal Disord Tech 2015;28:E310–5.
Schairer WW, Pedtke AC, Hu SS. Venous thromboembolism after spine surgery. Spine 2014;39:911–8.
Jo Kim H, Kepler C, Cunningham M, et al. Pulmonary embolism in spine surgery. Spine 2011;36:177–9.
Alen Nourian A, Cunningham CM, Bagheri A, et al. Effect of anatomic variability and level of approach on perioperative vascular complications with anterior lumbar interbody fusion. Spine 2016;41:E73–7.
Piper K, Algattas H, DeAndrea-Lazarus IA, et al. Risk factors associated with venous thromboembolism in patients undergoing spine surgery. J Neurosurg Spine 2017;26:90–6.
Arcelus JI, Kudran JC, Caprini JA. Venous thromboembolism following major orthopedic surgery: what is the risk after discharge? Orthopedics 2006;29:506–16.
Edmonds MJ, Crichton TJ, Runciman WB, et al. Evidence-based risk factors for postoperative deep vein thrombosis. ANZ J Surg 2004;74:1082–97.
Schulte LM, O’Brien JR, Bean MC, et al. Deep vein thrombosis and pulmonary embolism after spine surgery: incidence and patient risk factors. Am J Orthop 2013;42:267–70.
Kim HJ, Walcott-Sapp S, Adler RS, et al. Thromboembolic complications following spine surgery assessed with spiral CT scans: DVT/PE following spine surgery. HSS J 2011;7:37–40.
Nelson HD, Humphrey LL, Nygren P, et al. Postmenopausal hormone replacement therapy. JAMA 2002;288:871–81.
Vandenbroucke JP, Rosing J, Bloemenkamp WKP, et al. Oral contraceptives and the risk of venous thrombosis. N Engl J Med 2001;344:1527–35.
Lau D, Berger MS, Khullar D, et al. The impact of smoking on neurosurgical outcomes. J Neurosurg 2013;119:1323–30.
Musallam KM, Rosendaal FR, Zaatari G, et al. Smoking and the risk of mortality and vascular and respiratory events in patients undergoing major surgery. JAMA Surg 2013;148:755–62.
Borstt-Krafek B, Fink AM, Lipp C, et al. Proximal extent of pelvic vein thrombosis and its association with pulmonary embolism. J Vasc Surg 2003;37:518–22.
Carpenter JP, Holland GA, Baum RA, et al. Magnetic resonance venography for the detection of deep vein thrombosis: a comparison with contrast venography and duplex Doppler ultrasonography. J Vasc Surg 1993;18:734–41.
Author information
Authors and Affiliations
Corresponding author
Additional information
CCE II (reports other from Renovis Surgical, other from Renovis Surgical, outside the submitted work); NLL (none); LF (none); CCE (none).
Rights and permissions
About this article
Cite this article
Edwards, C.C., Lessing, N.L., Ford, L. et al. Deep Vein Thrombosis After Complex Posterior Spine Surgery: Does Staged Surgery Make a Difference?. Spine Deform 6, 141–147 (2018). https://doi.org/10.1016/j.jspd.2017.08.012
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2017.08.012