Abstract
Introduction
There is minimal literature regarding when dressing changes should be performed. We present the dressing change protocol adopted by our institution. The purpose of this study was to provide an update of our experience with this dressing change protocol over a 15-year period.
Methods
Effective January 2005, we implemented our universal protocol of no dressing changes for five days after surgery. Reviewing a health system administrative database, all spine surgery cases involving instrumentation performed at our institution were captured. Surgical site infection (SSI) cases: superficial, deep, and organ space as defined by the Centers for Disease Control and Prevention (CDC), were identified by reviewing an infection control database. Fisher exact test was used to compare SSI rates in all instrumented fusion cases from January 1999 to December 2004 (prior to implementation of the dressing change protocol) to those from January 2005 to December 2013 (after the protocol was initiated).
Results
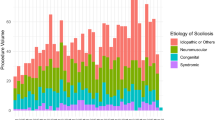
A total of 8,631 instrumented spine fusions were performed at a single institution from 1999 to 2013. Overall, after instituting our universal no-dressing-change protocol, SSI rates for all cervical, thoracic, and lumbar instrumented cases combined decreased from 3.9% (97/2473) to 0.93% (57/6158) (p <.0001). The reduction in SSI rates was most significant for posterior cervical and posterior lumbar surgeries. After our dressing change protocol was implemented, we saw an improvement in SSI rates for posterior cervical instrumented cases from 3.2% (6/186) to 0.50% (4/815) (p =.0041). Posterior lumbar instrumented fusion SSI rates dropped from 5.5% (65/1179) to 1.1% (32/2890) (p <.0001).
Conclusion
Dressing changes in the immediate postoperative period are not necessary. Applying a sterile dressing in the operating room may serve as a barrier to nosocomial pathogens during hospitalization. Our data suggest this dressing change protocol may lead to reduced SSI risk. Leaving the original postoperative surgical dressing intact is safe, simple, and cost-effective.
Similar content being viewed by others
References
Wimmer C, Gluch H, Franzreb M, Ogon M. Predisposing factors for infection in spine surgery: a survey of 850 spinal procedures. J Spinal Disord 1998;11:124–8.
Smith JS, Shaffrey CI, Sansur CA, et al. Rates of infection after spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 2011;36:556–63.
Weinstein MA, McCabe JP, Cammisa FPJ. Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord 2000;13:422–6.
Omeis IA, Dhir M, Sciubba DM, et al. Postoperative surgical site infections in patients undergoing spinal tumor surgery: incidence and risk factors. Spine (Phila Pa 1976) 2011;36:1410–9.
Abbey DM, Turner DM, Warson JS, et al. Treatment of postoperative wound infections following spinal fusion with instrumentation. J Spinal Disord 1995;8:278–83.
Picada R, Winter RB, Lonstein JE, et al. Postoperative deep wound infection in adults after posterior lumbosacral spine fusion with instrumentation: incidence and management. J Spinal Disord 2000;13:42–5.
Demura S, Kawahara N, Murakami H, et al. Surgical site infection in spinal metastasis: risk factors and countermeasures. Spine (Phila Pa 1976) 2009;34:635–9.
Tenney JH, Vlahov D, Salcman M, Ducker TB. Wide variation in risk of wound infection following clean neurosurgery. Implications for perioperative antibiotic prophylaxis. J Neurosurg 1985;62:243–7.
Kirkland KB, Briggs JP, Trivette SL, et al. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol 1999;20:725–30.
de Lissovoy G, Fraeman K, Hutchins V, et al. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control 2009;37:387–97.
Whitehouse JD, Friedman ND, Kirkland KB, et al. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol 2002;23:183–9.
Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection. Infect Control Hosp Epidemiol 1999;20:250–64.
Horan TC, Gaynes RP, Martone WJ, et al. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol 1992;13:606–8.
Watanabe M, Sakai D, Matsuyama D, et al. Risk factors for surgical site infection following spine surgery: efficacy of intraoperative saline irrigation. J Neurosurg Spine 2010;12:540–6.
Savage JW, Anderson PA. An update on modifiable factors to reduce the risk of surgical site infections. Spine J 2013;13:1017–29.
Blam OG, Vaccaro AR, Vanichkachorn JS, et al. Risk factors for surgical site infection in the patient with spinal injury. Spine (Phila Pa 1976) 2003;28:1475–80.
Fang A, Hu SS, Endres N, Bradford DS. Risk factors for infection after spinal surgery. Spine (Phila Pa 1976) 2005;30:1460–5.
Levi AD, Dickman CA, Sonntag VK. Management of postoperative infections after spinal instrumentation. J Neurosurg 1997;86:975–80.
Sweet FA, Roh M, Sliva C. Intrawound application of vancomycin for prophylaxis in instrumented thoracolumbar fusions. Spine (Phila Pa 1976) 2011;36:2084–8.
Khan NR, Thompson CJ, DeCuypere M, et al. A meta-analysis of spinal surgical site infection and vancomycin powder. J Neurosurg Spine 2014;21:1–10.
Massie JB, Heller JG, Abitbol JJ, et al. Postoperative posterior spinal wound infections. Clin Orthop Relat Res 1992:99–108.
Lonstein J, Winter R, Moe J, Gaines D. Wound infection with Harrington instrumentation and spine fusion for scoliosis. Clin Orthop Relat Res 1973:222–33.
Ahn DK, Park HS, Kim TW, et al. The degree of bacterial contamination while performing spine surgery. Asian Spine J 2013;7:8–13.
Christodoulou AG, Givissis P, Symeonidis PD, et al. Reduction of postoperative spinal infections based on an etiologic protocol. Clin Orthop Relat Res 2006;444:107–13.
Tegaderm, http://2014.igem.org/wiki/images/9/9f/SheffieldTimeline2.pdf. Accessed December 6, 2016.
Kirsner RS, Eaglstein WH. The wound healing process. Dermatol Clin 1993;11:629–40.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: None.
Rights and permissions
About this article
Cite this article
Bains, R.S., Kardile, M., Mitsunaga, L.K. et al. Postoperative Spine Dressing Changes Are Unnecessary. Spine Deform 5, 396–400 (2017). https://doi.org/10.1016/j.jspd.2017.04.005
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2017.04.005