Abstract
Study Design
Retrospective review.
Objectives
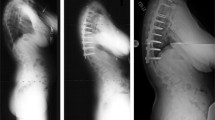
To identify factors associated with successful outcomes in patients treated with vertebral body stapling (VBS) for idiopathic scoliosis.
Summary of Background Data
The standard of care for moderate scoliosis (20°–45°) consists of observation and bracing with the goal of halting curve progression. Although several recent studies have confirmed the efficacy of bracing in altering the natural history of scoliosis, bracing is not universally effective. Recent studies have demonstrated that VBS is a safe and viable treatment for some young patients with scoliosis at risk for progression. The identification of factors associated with successful outcomes in VBS for idiopathic scoliosis would better define the population likely to benefit from VBS.
Methods
We retrospectively reviewed all patients from a single institution treated with VBS who met previously defined inclusion criteria. Successful treatment was defined as avoidance of a fusion and a final Cobb angle no more than 10° greater than the pretreatment Cobb angle.
Results
We identified 63 patients who met inclusion criteria. The patients underwent VBS at a mean age of 10.78 years and had a mean follow-up of 3.62 years (minimum 2 years). The mean pre-op Cobb angle for stapled thoracic curves was 29.5°. Seventy-four percent of the patients who had VBS of the thoracic curve have avoided progression and/or fusion, and the mean Cobb angle at most recent follow-up was 21.8°. The mean preoperative Cobb angle for lumbar curves was 31.1°. Eighty-two percent of the patients who had VBS of the lumbar curve have avoided progression and/or fusion, and their mean Cobb angle at follow-up was 21.6°.
Conclusion
VBS is effective at preventing progression and fusion for moderate idiopathic scoliosis in immature patients. The complication rates are low.
Similar content being viewed by others
References
Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013;369:1512–21.
Allington NJ, Bowen JR. Adolescent idiopathic scoliosis: treatment with the Wilmington brace. A comparison of full-time and parttime use. J Bone Joint Surg Am 1996;78:1056–62.
Karol LA. Effectiveness of bracing in male patients with idiopathic scoliosis. Spine (Phila Pa 1976) 2001;26:2001–5.
Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am 1995;77:815–22.
Rowe DE, Bernstein SM, Riddick MF, et al. A meta-analysis of the efficacy of non-operative treatments for idiopathic scoliosis. J Bone Joint Surg Am 1997;79:664–74.
Karol LA. Effect of compliance counseling on brace use and success in patients with adolescent idiopathic scoliosis. J Bone Joint Surg Am 2016;98:9–14.
Charles YP, Daures JP, de Rosa V, Dimeglio A. Progression risk of idiopathic juvenile scoliosis during pubertal growth. Spine (Phila Pa 1976) 2006;31:1933–42.
Katz DE, Herring JA, Browne RH, et al. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am 2010;92:1343–52.
Helfenstein A, Lankes M, Ohlert K, et al. The objective determination of compliance in treatment of adolescent idiopathic scoliosis with spinal orthoses. Spine (Phila Pa 1976) 2006;31:339–44.
Zuege RC, Kempken TG, Blount WP. Epiphyseal stapling for angular deformity at the knee. J Bone Joint Surg Am 1979;61:320–9.
Stevens PM, Maguire M, Dales MD, Robins AJ. Physeal stapling for idiopathic genu valgum. J Pediatr Orthop 1999;19:645–9.
Mente PL, Aronsson DD, Stokes IA, Iatridis JC. Mechanical modulation of growth for the correction of vertebral wedge deformities. J Orthop Res 1999;17:518–24.
Nachlas IW, Borden JN. The cure of experimental scoliosis by directed growth control. J Bone Joint Surg Am 1951;33:24–34.
Braun JT, Ogilvie JW, Akyuz E, et al. Experimental scoliosis in an immature goat model: a method that creates idiopathic-type deformity with minimal violation of the spinal elements along the curve. Spine (Phila Pa 1976) 2003;28:2198–203.
Braun JT, Ogilvie JW, Akyuz E, et al. Fusionless scoliosis correction using a shape memory alloy staple in the anterior thoracic spine of the immature goat. Spine (Phila Pa 1976) 2004;29:1980–9.
Betz RR, Kim J, D’Andrea LP, et al. An innovative technique of vertebral body stapling for the treatment of patients with adolescent idiopathic scoliosis: a feasibility, safety, and utility study. Spine (Phila Pa 1976) 2003;28(20 suppl):S255–65.
Betz RR, Ranade A, Samdani AF, et al. Vertebral body stapling: a fusionless treatment option for a growing child with moderate idiopathic scoliosis. Spine (Phila Pa 1976) 2010;35:169–76.
Weis JC, Betz RR, Clements DH, Balsara RK. Prevalence of perioperative complications after anterior spinal fusion for patients with idiopathic scoliosis. J Spinal Disord 1997;10:371–5.
Betz RR, D’Andrea LP, Mulcahey MJ, Chafetz RS. Vertebral body stapling procedure for the treatment of scoliosis in the growing child. Clin Orthop Relat Res 2005:55-60.
Lonner BS, Auerbach JD, Estreicher M, et al. Video-assisted thoracoscopic spinal fusion compared with posterior spinal fusion with thoracic pedicle screws for thoracic adolescent idiopathic scoliosis. J Bone Joint Surg Am 2009;91:398–408.
Newton PO, Upasani VV, Lhamby J, et al. Surgical treatment of main thoracic scoliosis with thoracoscopic anterior instrumentation. Surgical technique. J Bone Joint Surg Am 2009;91(suppl 2):233–48.
Cuddihy L, Danielsson AJ, Cahill PJ, et al. Vertebral body stapling versus bracing for patients with high-risk moderate idiopathic scoliosis. Biomed Res Int 2015;2015:438452.
Aulisa AG, Guzzanti V, Falciglia F, et al. Lyon bracing in adolescent females with thoracic idiopathic scoliosis: a prospective study based on SRS and SOSORT criteria. BMC Musculoskelet Disord 2015;16:316.
Jarvis J, Garbedian S, Swamy G. Juvenile idiopathic scoliosis: the effectiveness of part-time bracing. Spine (Phila Pa 1976) 2008;33:1074–8.
Lange JE, Steen H, Gunderson R, Brox JI. Long-term results after Boston brace treatment in late-onset juvenile and adolescent idiopathic scoliosis. Scoliosis 2011;6:18.
Aulisa AG, Guzzanti V, Marzetti E, et al. Brace treatment in juvenile idiopathic scoliosis: a prospective study in accordance with the SRS criteria for bracing studies—SOSORT award 2013 winner. Scoliosis 2014;9:3.
Clayson D, Luz-Alterman S, Cataletto MM, Levine DB. Long-term psychological sequelae of surgically versus nonsurgically treated scoliosis. Spine (Phila Pa 1976) 1987;12:983–6.
Misterska E, Glowacki M, Latuszewska J. Female patients’ and parents’ assessment of deformity- and brace-related stress in the conservative treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2012;37:1218–23.
Kwan MK, Zeyada HE, Chan CY. Prediction of curve correction using alternate level pedicle screw placement in patients with adolescent idiopathic scoliosis (AIS) Lenke 1 and 2 using supine side bending (SB) and fulcrum bending (FB) radiograph. Spine (Phila Pa 1976) 2015;40:1605–12.
Cheung KM, Cheng EY, Chan SC, et al. Outcome assessment of bracing in adolescent idiopathic scoliosis by the use of the SRS-22 questionnaire. Int Orthop 2007;31:507–11.
Liu RW, Teng AL, Armstrong DG, et al. Comparison of supine bending, push-prone, and traction under general anesthesia radiographs in predicting curve flexibility and postoperative correction in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2010;35:416–22.
Vidyadhara S, Mak KC. Predicting flexibility to bracing in adolescent idiopathic scoliosis using supine radiographs. J Orthop Surg (Hong Kong) 2008;12:89–95.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures
PJC (other from AAOS, POSNA, SRS, JBJS-A, and Spine Deformity, outside the submitted work); MA (none); ED (none); JPG (none); AFS (personal fees from DePuy Synthes Spine, Ethicon, Globus Medical, Misonix, Stryker, and Zimmer Biomet, outside the submitted work); JMP (personal fees from DePuy Synthes Spine and Globus Medical, outside the submitted work); RRB (personal fees from DePuy Synthes Spine, Globus Medical, Medtronic, and Zimmer Biomet; personal fees and other from Abyrx, Apifix, and SpineGuard; other from Advanced Vertebral Solutions, MiMedx, Orthobond, and Medovex, outside the submitted work).
The device(s)/drug(s) that is/are the subject of this manuscript is/are not FDA-approved for this indication and is/are not commercially available in the United States.
Rights and permissions
About this article
Cite this article
Cahill, P.J., Auriemma, M., Dakwar, E. et al. Factors Predictive of Outcomes in Vertebral Body Stapling for Idiopathic Scoliosis. Spine Deform 6, 28–37 (2018). https://doi.org/10.1016/j.jspd.2017.03.004
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2017.03.004
Keywords
- Vertebral body stapling
- Moderate idiopathic scoliosis
- Juvenile idiopathic scoliosis
- Adolescent idiopathic scoliosis