Abstract
Study Design
Retrospective analysis of propensity score–matched (PSM) observational cohorts.
Objectives
To evaluate and compare preoperative health-related quality of life (HRQoL) scores and radiographic measurements of young African and US adults with spinal deformity (ASD).
Summary of Background Data
Young ASD patients in the United States are motivated more to correct coronal and sagittal plane deformities than to alleviate pain. Motivations for surgical correction in young ASD patients in Africa have not been previously investigated.
Methods
Retrospective review of two large databases of African and US patients with ASD. African patients who underwent ASD surgery were PSM by age, gender, and pelvic tilt with US patients. Preoperative radiographic parameters and HRQoL scores (ODI, SRS-22r, back/leg pain) were compared between cohorts. Pearson correlations used to evaluate relationships between radiographic parameters and HRQoL scores.
Results
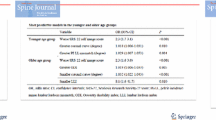
Fifty-four US patients (average age 22.9 ± 4.9 years; 0% African American) and 54 African patients (24.6 ± 7.2 years) met inclusion criteria. Compared to the United States, African patients had significantly lower body mass index (21.1 ± 3.3 vs. 24.6 ± 7.2) and more severe scoliosis, coronal malalignment, and sagittal malalignment (p <.05). Africans also had significantly better Oswestry Disability Index (12.8 vs. 17.7), worse Scoliosis Research Society questionnaire (SRS-22r)–Appearance (2.5 vs. 3.2), SRS-Function (3.3 vs. 3.9), and SRS-Total (3.2 vs. 3.5) scores than US patients (p <.05). SRS-Appearance scores correlated with Cobb angles of the upper thoracic (r = −0.321), thoracic (r = −0.277), and thoracolumbar (r = −0.300) curves for US patients. For African patients, global sagittal alignment and C7 inclination correlated with SRS-Appearance (r = −0.347,–0.346, respectively).
Conclusions
Young African ASD patients have significantly more severe deformity, less disability, and worse SRS-22r scores preoperatively than a matched cohort of US patients. Spinal deformity and associated poor self-image appear to be the major drivers of surgical intervention in this cohort. Global malalignment in African patients is most closely correlated with appearance scores and should be surgically addressed accordingly.
Level of Evidence
Level III.
Similar content being viewed by others
References
Ratahi ED, Crawford HA, Thompson JM, Barnes MJ. Ethnic variance in the epidemiology of scoliosis in New Zealand. J Pediatr Orthop 2002;22:784–7.
Segil C. The incidence of idiopathic scoliosis in the Bantu and white population groups in Johannesburg. J Bone 1974;56B:1974.
Daruwalla JS, Balasubramaniam P, Chay SO, et al. Idiopathic scoliosis. Prevalence and ethnic distribution in Singapore schoolchildren. J Bone Joint Surg Br 1985;67:182–4.
Gerard CS, O’Toole JE. Current techniques in the management of cervical myelopathy and radiculopathy. Neurosurg Clin N Am 2014;25:261–70.
Kebaish KM, Neubauer PR, Voros GD, et al. Scoliosis in adults aged forty years and older: prevalence and relationship to age, race, and gender. Spine (Phila Pa 1976) 2011;36:731–6.
Watanabe K, Lenke LG, Bridwell KH, et al. Cross-cultural comparison of the Scoliosis Research Society Outcomes Instrument between American and Japanese idiopathic scoliosis patients: are there differences? Spine (Phila Pa 1976) 2007;32:2711–4.
Verma K, Lonner BS, Hoashi JS, et al. Demographic factors affect Scoliosis Research Society-22 performance in healthy adolescents: a comparative baseline for adolescents with idiopathic scoliosis. Spine (Phila Pa 1976) 2010;35:2134–9.
Rillardon L, Levassor N, Guigui P, et al. [Validation of a tool to measure pelvic and spinal parameters of sagittal balance]. Rev Chir Orthop Reparatrice Appar Mot 2003;89:218–27.
Akbar M, Terran J, Ames CP, Lafage V, Schwab F. Use of Surgimap Spine in sagittal plane analysis, osteotomy planning, and correction calculation. Neurosurg Clin N Am 2013;24:163–72.
Rajnics P, Pomero V, Templier A, et al. Computer-assisted assessment of spinal sagittal plane radiographs. J Spinal Disord 2001;14:135–42.
Wu W, Liang J, Du Y, Tan X. Reliability and reproducibility analysis of the Cobb angle and assessing sagittal plane by computer-assisted and manual measurement tools. BMC Musculoskelet Disord 2014;15:33.
Schwab F, Ungar B, Blondel B, et al. SRS-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 2012;37:1077–82.
Bess S, Boachie-Adjei O, Burton D, et al. Pain and disability determine treatment modality for older patients with adult scoliosis, while deformity guides treatment for younger patients. Spine (Phila Pa 1976) 2009;34:2186–90.
Carreon LY, Sanders JO, Diab M, et al. Patient satisfaction after surgical correction of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2011;36:965–8.
Morse LJ, Kawakami N, Lenke LG, et al. Culture and ethnicity influence outcomes of the Scoliosis Research Society Instrument in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2012;37:1072–6.
Fukuhara S, Bito S, Green J, et al. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol 1998;51:1037–44.
Fukuhara S, Ware JE, Kosinski M, et al. Psychometric and clinical tests of validity of the Japanese SF-36 Health Survey. J Clin Epidemiol 1998;51:1045–53.
Verma K, Lonner B, Toombs CS, et al. International utilization of the SRS-22 instrument to assess outcomes in adolescent idiopathic scoliosis: what can we learn from a medical outreach group in Ghana? J Pediatr Orthop 2014;34:503–8.
Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol 1993;46:1417–32.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Conflicts of Interest and Source of Funding
This Study was partially funded by the International Spine Study Group through a grant from Depuy Synthes Spine.
Author disclosures
BYH (none); MFR (none); BGD (none); SB (grants from Grant from DePuy Synthes for International Spine Study Group Foundation [ISSGF], during the conduct of the study; grants and personal fees from K2 Medical, grants and personal fees from NuVasive, grants and personal fees from Innovasis, personal fees from Allosource, grants from Stryker, grants from Medtronic, personal fees from Pioneer, outside the submitted work); AAT (none); JKS (none); FJS (other from Nemaris INC, grants from AO, grants from SRS, grants from DePuy Synthesis Spine, personal fees from K2M, personal fees from NuVasive, personal fees from Medicrea, personal fees from MSD, personal fees from Biomet, personal fees from K2M, personal fees from MSD, outside the submitted work); VL (other from Nemaris INC, grants from DePuy Synthesis Spine, grants from NIH, grants from SRS, personal fees from Medcrea, personal fees from MSD, personal fees from DePuy, outside the submitted work); CPA (personal fees from UCSF, personal fees from DePuy, personal fees from Stryker, personal fees from Medtronic, personal fees from Biomet Spine, personal fees from Stryker, personal fees from Doctors Research Group, outside the submitted work; in addition, CPA has a patent Fish & Richardson, P.C. licensed); RH (none); JA (none); OB-A (grants from DePuy, personal fees and non-financial support from K2M, during the conduct of the study; grants and personal fees from K2M, outside the submitted work; in addition, OB-A has a patent K2M with royalties paid, and a patent WEIGAO with royalties paid).
Rights and permissions
About this article
Cite this article
Harris, B.Y., Roth, M.F., Diebo, B.G. et al. Investigating the Universality of Preoperative Health-Related Quality of Life (HRQoL) for Surgically Treated Spinal Deformity in Young Adults: A Propensity Score–Matched Comparison Between African and US Populations. Spine Deform 4, 351–357 (2016). https://doi.org/10.1016/j.jspd.2016.03.006
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2016.03.006