Abstract
Study Design
Retrospective analysis of Nationwide Inpatient Sample (NIS) database.
Objective
To analyze trends in utilization and hospital charges for multilevel spinal curvature surgery in patients over 60 from 2004 to 2011.
Summary of Background Data
Multilevel spinal curvature has been increasingly recognized as a major source of morbidity in patients over sixty years of age. The economic burden of non-operative management for spinal curvature is elusive and likely underestimated. Though patient reported outcomes suggest that surgical treatment of spinal curvature may be superior to non-operative treatment in selected patients, surgical utilization trends remain unclear.
Methods
Data were obtained from the NIS between 2004 and 2011. The NIS is the largest all-payer inpatient care database with approximately eight million annual patient discharges throughout the United States. Analysis included patients over age 60 with a spinal curvature diagnosis treated with a multi-level spinal fusion (≥3 levels fused) determined by ICD-9-CM diagnosis and procedure codes. Population-based utilization rates were calculated from US census data.
Results
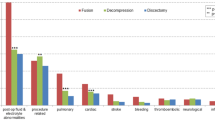
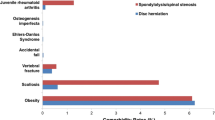
A total of 84,302 adult patients underwent multilevel spinal curvature surgery from 2004 to 2011. The annual number of ≥3 level spinal curvature fusions in patients over age 60 increased from 6,571 to 16,526, representing a 107.8% increase from 13.4 cases per 100,000 people in 2004 to 27.9 in 2011 (p <.001). Utilization rates in patients 65–69 years old experienced the greatest growth, increasing by 122% from 15.8 cases per 100,000 people to 35.1. Average hospital charges increased 108% from $90,557 in 2007 to $188,727 in 2011 (p < .001).
Conclusions
Rates of surgical management of multilevel spinal curvature increased from 2004 to 2011, exceeding growth of the 60+ age demographic during the same period. Growth was observed in all age demographics, and hospital charges consistently increased from 2004 to 2011 reflecting a per-user increase in expenditure.
Level of Evidence
III.
Similar content being viewed by others
References
Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976) 2005;30:1082–5.
Birknes JK, White AP, Albert TJ, et al. Adult degenerative scoliosis: a review. Neurosurgery 2008;63(3 suppl):94–103.
Pellisé F, Vila-Casademunt A, Ferrer M, et al. Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J 2015;24:3–11.
Otani K, Kikuchi S, Yabuki S, et al. Lumbar spinal stenosis has a negative impact on quality of life compared with other comorbidities: an epidemiological cross-sectional study of 1862 community-dwelling individuals. Sci World J 2013;2013:590652.
Paulus MC, Kalantar SB, Radcliff K. Cost and value of spinal deformity surgery. Spine (Phila Pa 1976) 2014;39:388–93.
Indrakanti SS, Weber MH, Takemoto SK, et al. Value-based care in the management of spinal disorders: a systematic review of cost-utility analysis. Clin Orthop Relat Res 2012;470:1106–23.
Hansson T, Hansson E, Malchau H. Utility of spine surgery: a comparison of common elective orthopaedic surgical procedures. Spine (Phila Pa 1976) 2008;33:2819–30.
Daubs MD, Lenke LG, Cheh G, et al. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976) 2007;32:2238–44.
Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus 2010;28:E1.
Yoshihara H, Yoneoka D. National trends in the surgical treatment for lumbar degenerative disc disease: US, 2000–2009. Spine J 2015;15:265–71.
Rajaee SS, Bae HW, Kanim LEA, Delamarter RB. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976) 2012;37:67–76.
Bae HW, Rajaee SS, Kanim LE. Nationwide trends in the surgical management of lumbar spinal stenosis. Spine (Phila Pa 1976) 2013;38:916–26.
Martin BI, Turner JA, Mirza SK, et al. Trends in health care expenditures, utilization, and health status among US adults with spine problems, 1997–2006. Spine (Phila Pa 1976) 2009;34:2077–84.
Smith JS, Shaffrey CI, Glassman SD, et al. Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine (Phila Pa 1976) 2011;36:817–24.
Berjano P, Lamartina C. Far lateral approaches (XLIF) in adult scoliosis. Eur Spine J 2013;22(suppl 2):S242–53.
Glassman SD, Carreon LY, Shaffrey CI, et al. The costs and benefits of nonoperative management for adult scoliosis. Spine (Phila Pa 1976) 2010;35:578–82.
Sansur CA, Smith JS, Coe JD, et al. Scoliosis Research Society morbidity and mortality of adult scoliosis surgery. Spine (Phila Pa 1976) 2011;36:E593–7.
Bridwell KH, Baldus C, Berven S, et al. Changes in radiographic and clinical outcomes with primary treatment adult spinal deformity surgeries from two years to three- to five-years follow-up. Spine (Phila Pa 1976) 2010;35:1849–54.
Crawford CH, Carreon LY, Bridwell KH, Glassman SD. Long fusions to the sacrum in elderly patients with spinal deformity. Eur Spine J 2012;21:2165–9.
Kim Y, Bridwell K, Lenke L. Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Joint Surg 2006;88:721–8.
Schairer WW, Carrer A, Sing DC, et al. Hospital readmission rates after surgical treatment of primary and metastatic tumors of the spine. Spine (Phila Pa 1976) 2014;39:1801–8.
Glassman SD, Dimar JR, Carreon LY. Revision rate after adult deformity surgery. Spine Deform 2015;3:199–203.
Youssef JA, Orndorff DO, Patty CA, et al. Current status of adult spinal deformity. Glob Spine J 2013;3:51–62.
Yadla S, Maltenfort MG, Ratliff JK, Harrop JS. Adult scoliosis surgery outcomes: a systematic review. Neurosurg Focus 2010;28:E3.
Lapp MA, Bridwell KH, Lenke LG, et al. Long-term complications in adult spinal deformity patients having combined surgery: a comparison of primary to revision patients. Spine (Phila Pa 1976) 2001;26:973–83.
Weinstein J, Lurie J, Olson P. United States trends and regional variations in lumbar spine surgery: 1992–2003. Spine (Phila Pa 1976) 2006;31:2707–14.
Hassanzadeh H, Jain A, El Dafrawy MH, et al. Three-column osteotomies in the treatment of spinal deformity in adult patients 60 years old and older: outcome and complications. Spine (Phila Pa 1976) 2013;38:726–31.
Kim HJ, Buchowski JM, Zebala LP, et al. RhBMP-2 is superior to iliac crest bone graft for long fusions to the sacrum in adult spinal deformity: 4- to 14-year follow-up. Spine (Phila Pa 1976) 2013;38:1209–15.
Crandall DG, Revella J, Patterson J, et al. Transforaminal lumbar interbody fusion with rhBMP-2 in spinal deformity, spondylolisthesis, and degenerative disease-part 1: large series diagnosis related outcomes and complications with 2- to 9-year follow-up. Spine (Phila Pa 1976) 2013;38:1128–36.
Boden SD. Overview of the biology of lumbar spine fusion and principles for selecting a bone graft substitute. Spine (Phila Pa 1976) 2002;27:26–31.
Carragee EJ, Hurwitz EL, Weiner BK. A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned. Spine J 2011;11:471–91.
Smith ZA, Fessler RG. Paradigm changes in spine surgery: evolution of minimally invasive techniques. Nat Rev Neurol 2012;8:443–50.
Deyo RA, Mirza SK. Trends and variations in the use of spine surgery. Clin Orthop Relat Res 2006;443:139–46.
Horst PK, Choo K, Bharucha N, Vail TP. Topics in training. J Bone Joint Surg 2015;97:869–75.
Tamariz L, Harkins T, Nair V. A systematic review of validated methods for identifying venous thromboembolism using administrative and claims data. Pharmacoepidemiol Drug Saf 2012;21:154–62.
Martin BI, Lurie JD, Tosteson ANA, et al. Indications for spine surgery: validation of an administrative coding algorithm to classify degenerative diagnoses. Spine (Phila Pa 1976) 2014;39:769–79.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures
DCS (none); RK (none); JDS (none); LNM (none); SB (personal fees from Consulting, grants from Spine Fellowship Grant: AO Spine, Globus, Nuvasive, outside the submitted work); SHB (personal fees from board membership: Globus Medical, Medtronic, Stryker; personal fees from consultancy: Medtronic, Stryker; grants from AO Spine, NIH, NSF, Globus Medical; personal fees from lectures: Stryker, Globus, Medtronic, RTI; personal fees from royalties: Medtronic; personal fees from stock/stock options: Simpirica Spine, Providence Medical, outside the submitted work).
This publication was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number TL1 TR000144. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Rights and permissions
About this article
Cite this article
Sing, D.C., Khanna, R., Shaw, J.D. et al. Increasing Rates of Surgical Management of Multilevel Spinal Curvature in Elderly Patients. Spine Deform 4, 365–372 (2016). https://doi.org/10.1016/j.jspd.2016.03.005
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2016.03.005