Abstract
Study Design
A retrospective review of patients who underwent posterior spinal fusion (PSF) and returned within 90 days with an acute infection.
Objectives
The study motive is to identify and understand the risk factors associated with failure of retaining spinal implants and failure to treat acute infection.
Background
The natural history of early surgical site infection (SSI) (less than 3 months) after PSF is not known and removing the implants early after PSF risks pseudarthrosis and deformity progression.
Methods
Patients ranging from 1999 to 2011 with surgical site infections (SSIs) who required irrigation and debridement within 3 months of PSF were identified from 4 institutions. Univariable and multivariable regression analysis were used to identify risk factors associated with failure of acute infection treatment.
Results
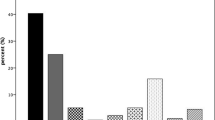
Eighty-two patients (59 female, 23 male) with a mean age of 13.6 years were identified. Median follow-up after initial surgery was 33 months (range: 12–112 months). Sixty-two (76%) were treated successfully with acute treatment and did not return with recurrent infection (cleared infection, group C); 20 (24%) returned later with chronic infection (recurrent infection, group R). Multivariable analysis indicated that patients with stainless steel implants (OR = 6.4, 95% CI = 1.7–32.1; p =.009) and older subjects (OR = 1.3, 95% CI = 1.0–1.6; p =.03) were more likely to present with recurrent infection. There was no difference between the groups with regard to the initial time of presentation post fusion, proportion of non-idiopathic diagnosis, rate of positive cultures, culture species, presence of fusion to pelvis, and time on antibiotic treatment.
Conclusions
Seventy-six percent of patients presenting with an SSI less than 3 months after PSF did not require implant removal to clear their infection. Early postoperative SSIs can be treated with retention or implant exchange. Older patients and patients with stainless steel instrumentation are more likely to present with a late recurrent infection compared to other metals.
Level of Evidence
Level III.
Similar content being viewed by others
References
Glotzbecker MP, Riedel MD, Vitale MG, et al. What’s the evidence? Systematic literature review of risk factors and preventive strategies for surgical site infection following pediatric spine surgery. J Pediatr Orthop 2013;33:479–87.
Glotzbecker MP, Vitale MG, Shea KG, et al. Surgeon practices regarding infection prevention for pediatric spinal surgery. J Pediatr Orthop 2013;33:694–9.
Hedequist D, Haugen A, Hresko T, et al. Failure of attempted implant retention in spinal deformity delayed surgical site infections. Spine (Phila Pa 1976) 2009;34:60–4.
Mackenzie WG, Matsumoto H, Williams BA, et al. Surgical site infection following spinal instrumentation for scoliosis: a multicenter analysis of rates, risk factors, and pathogens. J Bone Joint Surg Am 2013;95:800–6. S1-2.
Canavese F, Gupta S, Krajbich JI, et al. Vacuum-assisted closure for deep infection after spinal instrumentation for scoliosis. J Bone Joint Surg Br 2008;90:377–81.
van Rhee MA, de Klerk LW, Verhaar JA. Vacuum-assisted wound closure of deep infections after instrumented spinal fusion in six children with neuromuscular scoliosis. Spine J 2007;7:596–600.
Rohmiller MT, Akbarnia BA, Raiszadeh K, et al. Closed suction irrigation for the treatment of postoperative wound infections following posterior spinal fusion and instrumentation. Spine (Phila Pa 1976) 2010;35:642–6.
Vitale MG, Riedel MD, Glotzbecker MP, et al. Building consensus: development of a Best Practice Guideline (BPG) for surgical site infection (SSI) prevention in high-risk pediatric spine surgery. J Pediatr Orthop 2013;33:471–8.
Clark CE, Shufflebarger HL. Late-developing infection in instrumented idiopathic scoliosis. Spine (Phila Pa 1976) 1999;24:1909–12.
Richards BR, Emara KM. Delayed infections after posterior TSRH spinal instrumentation for idiopathic scoliosis: revisited. Spine (Phila Pa 1976) 2001;26:1990–6.
Richards BS. Delayed infections following posterior spinal instrumentation for the treatment of idiopathic scoliosis. J Bone Joint Surg Am 1995;77:524–9.
Di Silvestre M, Bakaloudis G, Lolli F, et al. Late-developing infection following posterior fusion for adolescent idiopathic scoliosis. Eur Spine J 2011;20(suppl 1):S121–7.
Rihn JA, Lee JY, Ward WT. Infection after the surgical treatment of adolescent idiopathic scoliosis: evaluation of the diagnosis, treatment, and impact on clinical outcomes. Spine (Phila Pa 1976) 2008;33:289–94.
Gristina AG, Price JL, Hobgood CD, et al. Bacterial colonization of percutaneous sutures. Surgery 1985;98:12–9.
Cahill PJ, Warnick DE, Lee MJ, et al. Infection after spinal fusion for pediatric spinal deformity: thirty years of experience at a single institution. Spine (Phila Pa 1976) 2010;35:1211–7.
Ho C, Skaggs DL, Weiss JM, et al. Management of infection after instrumented posterior spine fusion in pediatric scoliosis. Spine (Phila Pa 1976) 2007;32:2739–44.
Muschik M, Lück W, Schlenzka D. Implant removal for late-developing infection after instrumented posterior spinal fusion for scoliosis: reinstrumentation reduces loss of correction. A retrospective analysis of 45 cases. Eur Spine J 2004;13:645–51.
Arens S, Schlegel U, Printzen G, et al. Influence of materials for fixation implants on local infection an experimental study of steel versus titanium dcp in rabbits. J Bone Joint Surg Br 1996;78:647–51.
Soultanis KC, Pyrovolou N, Zahos KA, et al. Late postoperative infection following spinal instrumentation: stainless steel versus titanium implants. J Surg Orthop Adv 2008;17:193–9.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures
MPG (other from Medtronic, from null, outside the submitted work), JAG (none), PEM (none), MJT (none), DLS (grants from POSNA & SRS, personal fees from Biomet; Medtronic, non-financial support from Growing Spine Study Group, Growing Spine Foundation, Medtronic Strategic Advisory Board, nonfinancial support from Scoliosis Research Society, personal fees from Expert testimony, personal fees from Biomet; Medtronic; Stryker, other from Wolters Kluwer Health–Lippincott Williams & Wilkins; Biomet Spine, personal fees from Stryker; Biomet, Medtronic, other from Medtronic, outside the submitted work; in addition, DLS has a patent Medtronic issued), MGV (personal fees and other from Stryker, Biomet, grants, personal fees and nonfinancial support from SRS, POSNA, CWSDSG, OREF OMeGA, CSSG FoxPSDSG, personal fees from CSSG, POSSNA, during the conduct of the study; personal fees and other from Stryker, Biomet, grants, personal fees and non-financial support from SRS, POSNA, CWSDSG, OREF OMeGA, CSSG FoxPSDSG, personal fees from CSSG, POSSNA, outside the submitted work), JMF (personal fees from Biomet, personal fees from LWW, outside the submitted work), KKB (none), GIP (none), BNA (none), DJH (none).
This study received institutional review board approval from the Office of Clinical Investigation, Boston Children’s Hospital (No. IRB-P00007600).
Rights and permissions
About this article
Cite this article
Glotzbecker, M.P., Gomez, J.A., Miller, P.E. et al. Management of Spinal Implants in Acute Pediatric Surgical Site Infections: A Multicenter Study. Spine Deform 4, 277–282 (2016). https://doi.org/10.1016/j.jspd.2016.02.001
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2016.02.001