Abstract
Study Design
Retrospective analysis of relevant in-hospital patient records from the New York State Inpatient Database.
Objective
We aimed to assess reoperation risk in adolescent idiopathic scoliosis (AIS) by surgeon and hospital operative volume.
Summary of Background Data
The need for early reoperation can be devastating for patient and family, is a burden to the physician and adds significant cost. Previous studies have shown improved outcomes associated with higher volume surgeons and hospitals, but reoperation events have not yet been explored.
Methods
The 2008-2011 New York State Inpatient Database was queried using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for adolescent idiopathic scoliosis patients aged 10-21 undergoing spine arthrodesis. Patient identifiers and revisit linkage variables were used to identify reoperation events. Annual surgeon and hospital volumes were stratified into tertiles (low, medium, high) via identifier codes. The relative risk of reoperation after spine arthrodesis was computed based on relevant patient inpatient stays.
Results
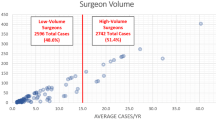
Over 2008 to 2011, a total of 3,928 primary fusion operations for AIS were identified. The overall rate of reoperation after spine fusion for idiopathic scoliosis was 7. 1%. Low volume surgeons performed less than 6 AIS fusions per year, medium volume surgeons performed less than 43, and high volume surgeons performed from 43 to 228. Reoperation after a primary fusion for adolescent idiopathic scoliosis showed reduced frequency among higher volume surgeons (14. 1% for low vs. 5. 1% for high, p<0. 001, see Table for Hospitals).
Conclusions
Early reoperation after spine fusion for idiopathic scoliosis is seen more frequently in lower volume institutions and surgeons. Appreciating the resources and limitations at a clinician’s institution is important to developing practices to prevent these devastating events. This work also has implications for strategies that aim to direct limited healthcare resources to centers with low complication rates.
Similar content being viewed by others
References
Hibbs RA. An operation for progressive spinal deformities: a preliminary report of three cases from the service of the orthopaedic hospital. 1911. Clin Orthop Relat Res 2007;2:17–20.
Dasenbrock HH, Clarke MI, Witham TF, Sciubba DM, Gokaslan ZL, Bydon A. The impact of provider volume on the outcomes after surgery for lumbar spinal stenosis. Neurosurgery 2012;2:1346–53; discussion 1353-4.
Farjoodi P, Skolasky RL, Riley LH. The effects of hospital and surgeon volume on postoperative complications after lumbar spine surgery. Spine 2011;2:2069–75.
Shervin N, Rubash HE, Katz JN. Orthopaedic procedure volume and patient outcomes: a systematic literature review. Clin Orthop Relat Res 2007;2:35–41.
Luft HS, Bunker JP, Enthoven AC. Should operations be regionalized? The empirical relation between surgical volume and mortality. N EnglJ Med 1979;2:1364–9.
Lonner BS, Auerbach JD, Estreicher MB, Kean KE. Thoracic pedicle screw instrumentation: the learning curve and evolution in technique in the treatment of adolescent idiopathic scoliosis. Spine 2009;2:2158–64.
Cahill PJ, Pahys JM, Asghar J, et al. The effect of surgeon experience on outcomes of surgery for adolescent idiopathic scoliosis. J Bone Joint Surg 2014;2:1333–9.
Reames DL, Smith JS, Fu K-MG, et al. Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society Morbidity and Mortality database. Spine 2011;2:1484–91.
Mohamad F, Parent S, Pawelek J, et al. Perioperative complications after surgical correction in neuromuscular scoliosis. J Pediatr Orthop 2007;2:392–7.
Coe JD, Arlet V, Donaldson W, et al. Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine 2006;2:345–9.
Patil CG, Santarelli J, Lad SP, Ho C, Tian W, Boakye M. Inpatient complications, mortality, and discharge disposition after surgical correction of idiopathic scoliosis: a national perspective. Spine J 2008;2:904–10.
Herwaldt LA, Cullen JJ, Scholz D, et al. A prospective study of outcomes, healthcare resource utilization, and costs associated with postoperative nosocomial infections. Infect Control Hosp Epidemiol 2006;2:1291–8.
Sponseller PD, LaPorte DM, Hungerford MW, Eck K, Bridwell KH, Lenke LG. Deep wound infections after neuromuscular scoliosis surgery: a multicenter study of risk factors and treatment outcomes. Spine 2000;2:2461–6.
Sponseller PD, Shah SA, Abel MF, Newton PO, Letko L, Marks M. Infection rate after spine surgery in cerebral palsy is high and impairs results: multicenter analysis of risk factors and treatment. Clin Orthop Relat Res 2010;2:711–6.
Glassman SD, Carreon LY, Djurasovic M, et al. RhBMP-2 versus iliac crest bone graft for lumbar spine fusion: a randomized, controlled trial in patients over sixty years of age. Spine 2008;2:2843–9.
Carreon LY, Glassman SD, Djurasovic M, et al. RhBMP-2 versus iliac crest bone graft for lumbar spine fusion in patients over 60 years of age: a cost-utility study. Spine 2009;2:238–43.
Bohl DD, Russo GS, Basques BA, et al. Variations in data collection methods between national databases affect study results: a comparison of the nationwide inpatient sample and national surgical quality improvement program databases for lumbar spine fusion procedures. J Bone Joint Surg 2014;96:e193.
AHRQ Quality Control. Available at: http://www. hcup-us.ahrq.gov/db/quality.jsp#procedures. Accessed December 13, 2014.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no copyrighted material to report.
The authors attest that appropriate institutional IRB approval was obtained for this study.
No funding sources were obtained for this study.
Rights and permissions
About this article
Cite this article
Paul, J.C., Lonner, B.S., Vira, S. et al. High-Volume Hospitals and Surgeons Experience Fewer Early Reoperation Events After Adolescent Idiopathic Scoliosis Surgery. Spine Deform 3, 496–501 (2015). https://doi.org/10.1016/j.jspd.2015.03.005
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2015.03.005